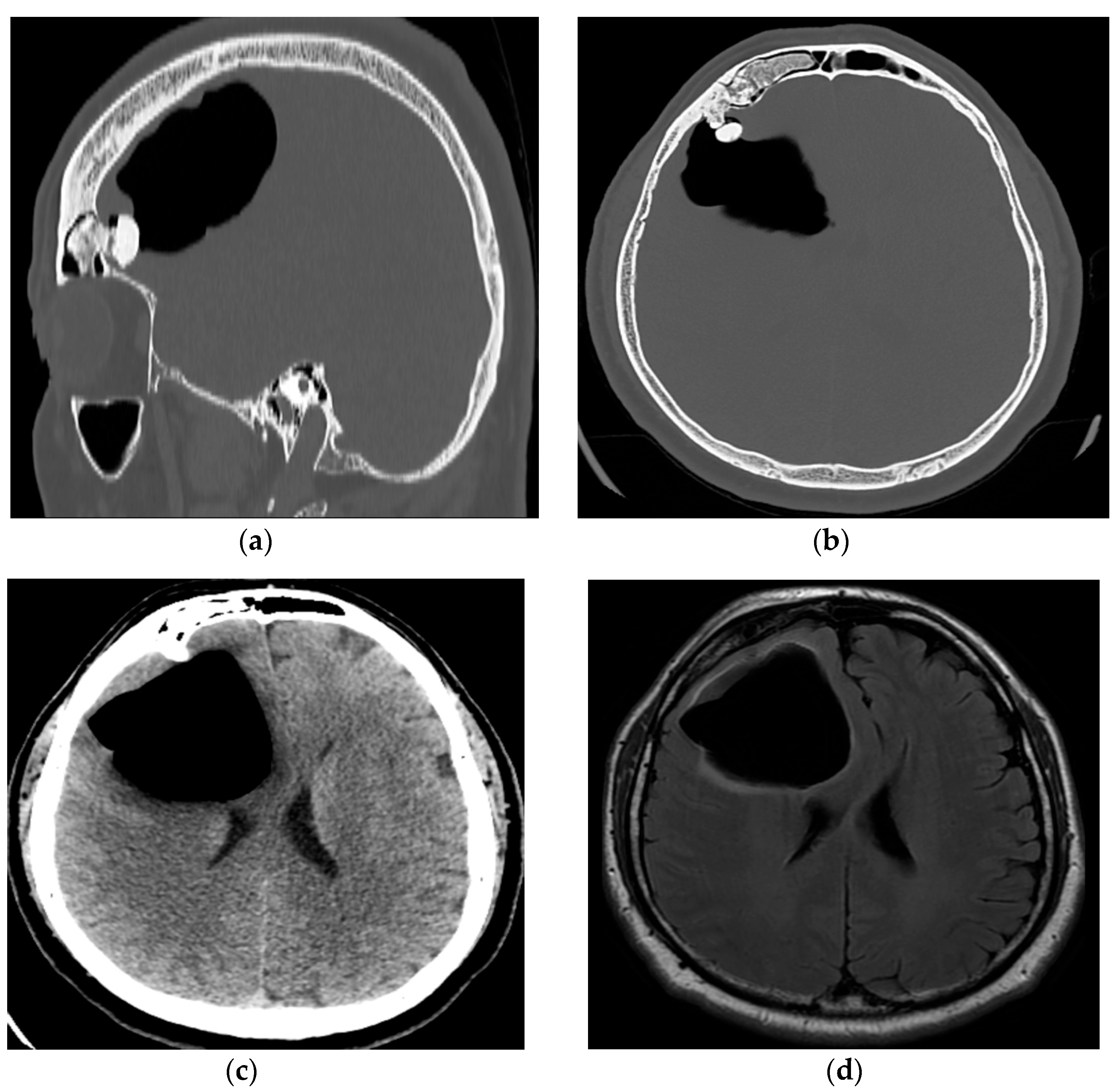
Air Travel-Triggered Tension Pneumocephalus Caused by a Frontal Sinus Osteoma: Case Report
Abstract
1. Introduction and Clinical Significance
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Markham, J.W. The clinical features of pneumocephalus based upon a survey of 284 cases with report of 11 additional cases. Acta Neurochir. 1967, 16, 1–78. [Google Scholar] [CrossRef] [PubMed]
- Webber-Jones, J.E. Tension pneumocephalus. J. Neurosci. Nurs. 2005, 37, 272–276. [Google Scholar] [CrossRef] [PubMed]
- Huneidi, A.H.; Afshar, F. Chronic spontaneous tension pneumocephalus due to benign frontal sinus osteoma. Br. J. Neurosurg. 1989, 3, 389–392. [Google Scholar] [CrossRef]
- Munshi, N.H.; Ramakrishnan, V. Pneumocephalus following sneeze suppression. Radiol. Case Rep. 2023, 18, 1527–1529. [Google Scholar] [CrossRef] [PubMed]
- Albert, A.; Allbright, R.; Nichols, T.; Farley, E.; Vijayakumar, S. Pneumocephalus after the Treatment of an Inoperable Superior Sulcus Tumor with Chemoradiation. Case Rep. Oncol. Med. 2017, 2017, 3016517. [Google Scholar] [CrossRef]
- Gupta, M.; Kumar Varma, K.K.; Singh Chhabra, H. A rare case of concomitant pneumocephalus and pneumorachis after lumbar spine surgery with late presenting dural leak. Spinal Cord Ser. Cases 2019, 5, 86. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.H.; Hui, Y.Y.; Wong, O.F.; Ma, H.M. A teenager with head injury. Hong Kong J. Emerg. Med. 2018, 25, 37–38. [Google Scholar] [CrossRef]
- L’Hommedieu, L.M.; Dingeldein, M.W.; Tomei, K.L.; Kilbane, B.J. Acute Management of Tension Pneumocephalus in a Pediatric Patient: A Case Report. J. Emerg. Med. 2018, 54, 112–115. [Google Scholar] [CrossRef] [PubMed]
- Bichsel, O.; Hauck, A.; Oertel, M. Air travel with pneumocephalus: A systematic review. Acta Neurochir. 2022, 164, 2395–2400. [Google Scholar] [CrossRef]
- Amato-Watkins, A.; Rao, V.M.; Leach, P. Air travel after intracranial surgery: A survey of advice given to patients by consultant neurosurgeons in the UK. Br. J. Neurosurg. 2013, 27, 9–11. [Google Scholar] [CrossRef]
- Lim, E.; Lan, B.L.; Ooi, E.H.; Low, H.L. Pneumocephalus and air travel: An experimental investigation on the effects of aircraft cabin pressure on intracranial pressure. Sci. Rep. 2020, 10, 13626. [Google Scholar] [CrossRef] [PubMed]
- Kamide, T.; Nakada, M.; Hayashi, Y.; Hayashi, Y.; Uchiyama, N.; Hamada, J. Intraparenchymal pneumocephalus caused by ethmoid sinus osteoma. J. Clin. Neurosci. 2009, 16, 1487–1489. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Castedo, J.; Ferreira, A.P.; Camacho, Ó. Hyperbaric oxygen therapy in the treatment of pneumocephalus associated with epidural block: Case report. Braz. J. Anesthesiol. 2021, 71, 295–298. [Google Scholar] [CrossRef]
- Rathore, Y.S.; Gupta, D.; Sathyarthi, G.; Mahapatra, A. Extradural hematoma with delayed onset pneumocephalus and contré-coup injury. Indian J. Neurotrauma 2010, 7, 75–77. [Google Scholar] [CrossRef]
- Abu-Hamdiyah, O.J.; Al Sharie, S.; Awadi, S.; Khamees, A.; Athamneh, M.J. Pneumocephalus secondary to a spinal surgery: A literature review and a case report. Int. J. Surg. Case Rep. 2021, 86, 106342. [Google Scholar] [CrossRef]
- Kankane, V.K.; Jaiswal, G.; Gupta, T.K. Posttraumatic delayed tension pneumocephalus: Rare case with review of literature. Asian J. Neurosurg. 2016, 11, 343–347. [Google Scholar] [CrossRef] [PubMed]
- Kwon, J.; Rha, H.K.; Park, H.K.; Chough, C.K.; Joo, W.I.; Cho, S.H.; Gu, W.; Moon, W.; Han, J. Proper Management of Posttraumatic Tension Pneumocephalus. Korean J. Neurotrauma 2017, 13, 158–161. [Google Scholar] [CrossRef]
- Sandhu, G.; Gonzalez-Zacarias, A.; Fiorda-Diaz, J.; Soghomonyan, S.; Abdel-Rasoul, M.; Prevedello, L.M.; Uribe, A.A.; Stoicea, N.; Targonski, D.; Prevedello, D.M.; et al. A prospective randomized clinical trial to evaluate the impact of intraoperative ventilation with high oxygen content on the extent of postoperative pneumocephalus in patients undergoing craniotomies. Br. J. Neurosurg. 2019, 33, 119–124. [Google Scholar] [CrossRef] [PubMed]
- Mahabir, R.C.; Szymczak, A.; Sutherland, G.R. Intracerebral pneumatocele presenting after air travel. J. Neurosurg. 2004, 101, 340–342. [Google Scholar] [CrossRef] [PubMed]
- Aaron, K.A.; Eltawil, Y.; Fernandez-Miranda, J.C.; Jackler, R.K. Spontaneous Otogenic Pneumocephalus Triggered by Air Travel. Otol. Neurotol. 2024, 45, e68–e70. [Google Scholar] [CrossRef]
- Jensen, M.B.; Adams, H.P. Pneumocephalus after air travel. Neurology 2004, 63, 400–401. [Google Scholar] [CrossRef]
- Javan, R.; Duszak, R., Jr.; Eisenberg, A.D.; Eggers, F.M. Spontaneous pneumocephalus after commercial air travel complicated by meningitis. Aviat. Space Environ. Med. 2011, 82, 1153–1156. [Google Scholar] [CrossRef] [PubMed]
- Pollaers, K.; Kuthubutheen, J. Spontaneous Otogenic Pneumocephalus due to Frequent Plane Travelling. Case Rep. Otolaryngol. 2019, 2019, 8768506. [Google Scholar] [CrossRef] [PubMed]
- Donovan, D.J.; Iskandar, J.I.; Dunn, C.J.; King, J.A. Aeromedical evacuation of patients with pneumocephalus: Outcomes in 21 cases. Aviat. Space Environ. Med. 2008, 79, 30–35. [Google Scholar] [CrossRef]
- Ruddick, B.; Tomlin, J. Pneumocephalus and neurosurgery in rotary aircrew. Aerosp. Med. Hum. Perform. 2015, 86, 59–61. [Google Scholar] [CrossRef] [PubMed]
- Arifianto, M.R.; Ma’ruf, A.Z.; Ibrahim, A.; Bajamal, A.H. Interhemispheric and Infratentorial Subdural Empyema with Preseptal Cellulitis as Complications of Sinusitis: A Case Report. Pediatr. Neurosurg. 2018, 53, 128–133. [Google Scholar] [CrossRef]
- Nicoli, T.K.; Oinas, M.; Niemelä, M.; Mäkitie, A.A.; Atula, T. Intracranial Suppurative Complications of Sinusitis. Scand. J. Surg. 2016, 105, 254–262. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Djurdjevic, A.; Lepic, M.; Djurdjevic, J.; Stankovic, S.; Pavlicevic, G. Air Travel-Triggered Tension Pneumocephalus Caused by a Frontal Sinus Osteoma: Case Report. Reports 2025, 8, 10. https://doi.org/10.3390/reports8010010
Djurdjevic A, Lepic M, Djurdjevic J, Stankovic S, Pavlicevic G. Air Travel-Triggered Tension Pneumocephalus Caused by a Frontal Sinus Osteoma: Case Report. Reports. 2025; 8(1):10. https://doi.org/10.3390/reports8010010
Chicago/Turabian StyleDjurdjevic, Aleksandar, Milan Lepic, Jovana Djurdjevic, Svetozar Stankovic, and Goran Pavlicevic. 2025. "Air Travel-Triggered Tension Pneumocephalus Caused by a Frontal Sinus Osteoma: Case Report" Reports 8, no. 1: 10. https://doi.org/10.3390/reports8010010
APA StyleDjurdjevic, A., Lepic, M., Djurdjevic, J., Stankovic, S., & Pavlicevic, G. (2025). Air Travel-Triggered Tension Pneumocephalus Caused by a Frontal Sinus Osteoma: Case Report. Reports, 8(1), 10. https://doi.org/10.3390/reports8010010





