Social Isolation as a Precipitating Factor for Charles Bonnet Syndrome in a Patient with Mild Visual Deterioration
Abstract
1. Introduction
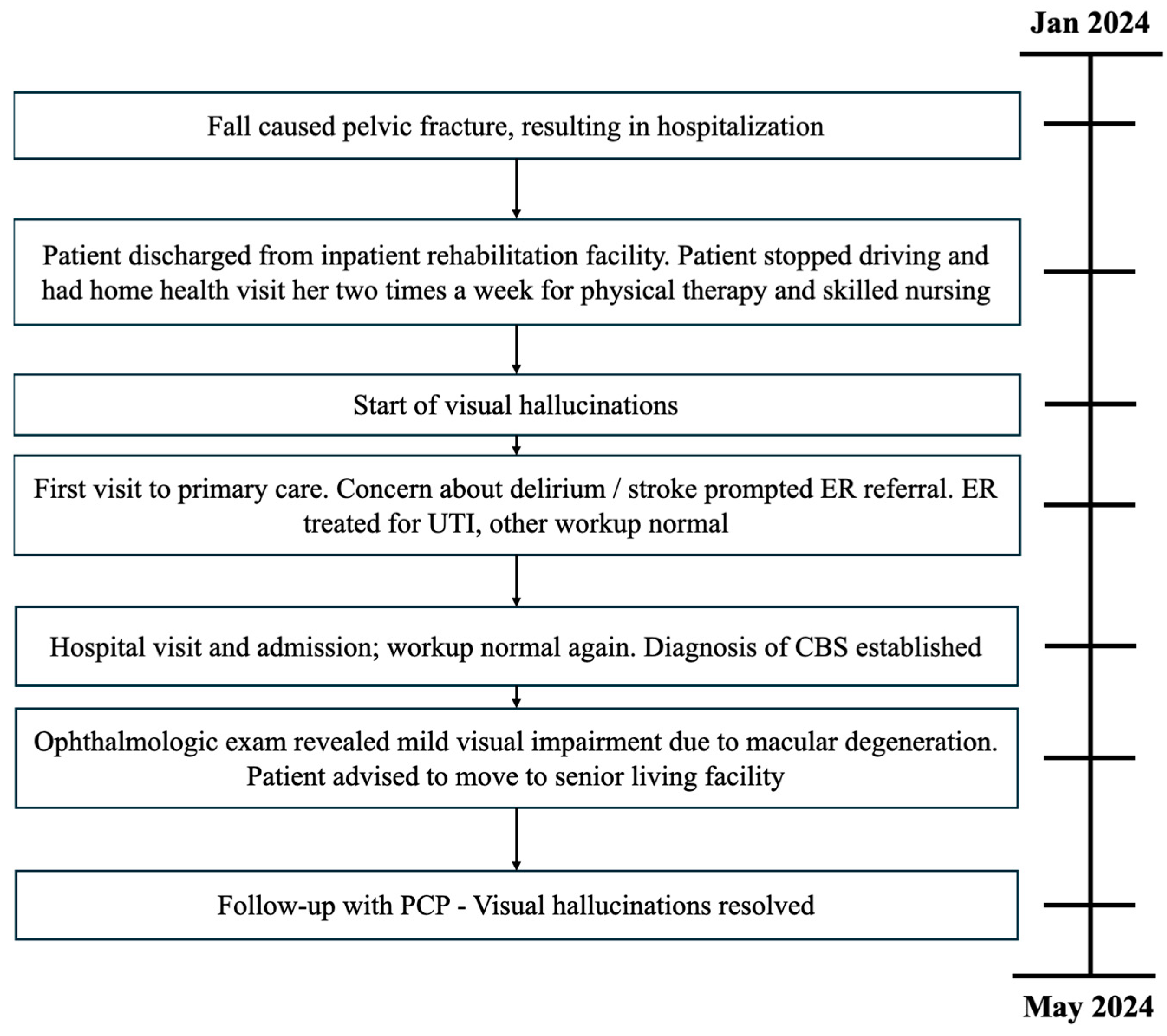
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jackson, M.L.; Ferencz, J. Cases: Charles Bonnet syndrome: Visual loss and hallucinations. CMAJ 2009, 181, 175–176. [Google Scholar] [CrossRef] [PubMed]
- Jan, T.; Del Castillo, J. Visual hallucinations: Charles bonnet syndrome. West. J. Emerg. Med. 2012, 13, 544–547. [Google Scholar] [CrossRef] [PubMed]
- Maruzairi, H.; Joo, C.L. A Case Report on Charles Bonnet Syndrome. Iran. J. Psychiatry 2022, 17, 240–242. [Google Scholar] [CrossRef] [PubMed]
- Kompella, S.; Kaushal, S.; Khan, S.A.; Alvarez Villalba, C.L. A Case Report and Review: Charles Bonnet Syndrome Plus With Dementia. HCA Healthc. J. Med. 2022, 3, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Kelson, M.; Santos, T.; Athanasios, A.; Fitzsimmons, A. Out of sight, am I losing my mind? A case report on Visual ReleHallucinations—Charles Bonnet Syndrome. Psychiatry Res. Case Rep. 2022, 1, 100036. [Google Scholar] [CrossRef]
- Russell, G.; Burns, A. Charles Bonnet syndrome and cognitive impairment: A systematic review. Int. Psychogeriatr. 2014, 26, 1431–1443. [Google Scholar] [CrossRef] [PubMed]
- Voit, M.; Jerusik, B.; Chu, J. Charles Bonnet Syndrome as Another Cause of Visual Hallucinations. Cureus 2021, 13, e12922. [Google Scholar] [CrossRef] [PubMed]
- Jones, L.; Ditzel-Finn, L.; Enoch, J.; Moosajee, M. An overview of psychological and social factors in Charles Bonnet syndrome. Ther. Adv. Ophthalmol. 2021, 13, 25158414211034715. [Google Scholar] [CrossRef] [PubMed]
- Reichert, D.P.; Seriès, P.; Storkey, A.J. Charles Bonnet syndrome: Evidence for a generative model in the cortex? PLoS Comput. Biol. 2013, 9, e1003134. [Google Scholar] [CrossRef]
- Jones, L.; Ditzel-Finn, L.; Potts, J.; Moosajee, M. Exacerbation of visual hallucinations in Charles Bonnet syndrome due to the social implications of COVID-19. BMJ Open Ophthalmol. 2021, 6, e000670. [Google Scholar] [CrossRef]
- Menon, G.J.; Rahman, I.; Menon, S.J.; Dutton, G.N. Complex visual hallucinations in the visually impaired: The Charles Bonnet Syndrome. Surv. Ophthalmol. 2003, 48, 58–72. [Google Scholar] [CrossRef] [PubMed]
- Holroyd, S.; Rabins, P.V.; Finkelstein, D.; Lavrisha, M. Visual hallucinations in patients from an ophthalmology clinic and medical clinic population. J. Nerv. Ment. Dis. 1994, 182, 273–276. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, N.R., Jr. Social isolation in older adults: An evolutionary concept analysis. J. Adv. Nurs. 2009, 65, 1342–1352. [Google Scholar] [CrossRef] [PubMed]
- Jacob, A.; Prasad, S.; Boggild, M.; Chandratre, S. Charles Bonnet syndrome-elderly people and visual hallucinations. BMJ 2004, 26, 1552–1554. [Google Scholar] [CrossRef] [PubMed]
- Lang, U.E.; Stogowski, D.; Schulze, D.; Domula, M.; Schmidt, E.; GaLLinat, J.; Tugtekin, S.M.; Felber, W. Charles Bonnet Syndrome: Successful treatment of visual hallucinations due to vision loss with selective serotonin reuptake inhibitors. J. Psychopharmacol. 2006, 21, 553–555. [Google Scholar] [CrossRef] [PubMed]
- Teunisse, R.J.; Zitman, F.G.; Raes, D.C. Clinical evaluation of 14 patients with the Charles Bonnet syndrome (isolated visual hallucinations). Compr. Psychiatry 1994, 35, 70–75. [Google Scholar] [CrossRef] [PubMed]
- Panayiotopoulos, C.P. Visual phenomena and headache in occipital epilepsy: A review, a systematic study and differentiation from migraine. Epileptic Disord. 1999, 1, 205–216. [Google Scholar] [CrossRef]
- Lepore, F.E. Spontaneous visual phenomena with visual loss: 104 patients with lesions of retinal and neural afferent pathways. Neurology 1990, 40, 444–447. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Ramos, J.R.; Ortoll, R.; Paulson, G.W. Visual hallucinations associated with Parkinson disease. Arch. Neurol. 1996, 53, 1265–1268. [Google Scholar] [CrossRef]
- Goodwin, D.W.; Alderson, P.; Rosenthal, R. Clinical significance of hallucinations in psychiatric disorders. A study of 116 hallucinatory patients. Arch. Gen. Psychiatry 1971, 24, 76–80. [Google Scholar] [CrossRef]
- Turner, R.C.; Lichstein, P.R.; Peden, J.G., Jr.; Busher, J.T.; Waivers, L.E. Alcohol withdrawal syndromes: A review of pathophysiology, clinical presentation, and treatment. J. Gen. Intern. Med. 1989, 4, 432–444. [Google Scholar] [CrossRef] [PubMed]
- Szucs, A.; Janszky, J.; Holló, A.; Migléczi, G.; Halász, P. Misleading hallucinations in unrecognized narcolepsy. Acta Psychiatr. Scand. 2003, 108, 314–316, discussion 316–317. [Google Scholar] [CrossRef] [PubMed]
| Authors, Year | Age | Vision Loss Etiology | Visual Acuity | Key Findings | Treatment |
|---|---|---|---|---|---|
| Jackson et al., 2009 [1] | 69 | Exudative age-related macular degeneration | 20/70 (OD), 20/50 (OS) | Abrupt change in vision 16 months prior to the onset of visual hallucinations | Intraocular ranibizumab injections to prevent visual deterioration |
| Jan et al., 2012 [2] | 86 | Open-angle glaucoma, macular degeneration, cataracts | 20/50 (OD) 20/100 (OS) | Abrupt decline in vision in a week, 30/30 Mini Mental Status Exam (MMSE) | Visual correction |
| Maruzairi et al., 2022 [3] | 63 | Bilateral retinal detachment, cataract s/p intraocular lens implant in right eye | None provided | Visual hallucinations associated with persecutory delusion due to worsening vision in right eye, symptoms resolved upon closing eyes and prayer | Treatments of Quetiapine and Zolpidem |
| Kompella et al., 2022 [4] | 67 | Diabetic retinopathy and bilateral sensorineural hearing loss | None provided | Veteran experiencing visual and musical hallucinations for few days, associated depression and mild dementi | Reassurance; trial of antipsychotics worsened symptoms |
| Kelson et al., 2022 [5] | 93 | Bilateral cataracts | 20/50 (OD) 20/60 (OS) | Visual hallucinations with mild cognitive impairment, sudden 2 week decline in visual acuity, 25/30 MMSE | Motivational interviewing, supportive psychotherapy, assisted living facility |
| Voit et al., 2021 [7] | 68 | Right-sided ptosis, blepharoplasty, infarct in the right posterior occipital lobe | 20/40 (OD) 20/60 (OS) | Hallucinations in left visual field, subacute infarct in the right posterior occipital lobe | Neurology and ophthalmology follow-up at tertiary center |
| Jacob et al., 2004 [14] | 87 | Registered blind due to advanced macular degeneration | 1/60 (OD) 1/60 (OS) | Confused for early dementia | Reassurance |
| Lang et al., 2006 [15] | 78 | Registered blind | Hand motion | Four-week history of depression, hallucinations occurring for one year | Treatment of Venlafaxine |
| Right Eye (OD) | Left Eye (OS) | |
|---|---|---|
| Visual Acuity Testing | ||
| Distant | 20/60 | 20/25 |
| Near | 20/50 | 20/70 |
| Fundoscopic Exam | ||
| Cup to Disc Ratio (C) | 0.3 (Normal) | 0.3 (Normal) |
| Optic Nerve | Peri-papillary atrophy present | Peri-papillary atrophy present |
| Vitreous | (−) Shafer’s sign (negative) | (−) Shafer’s sign (negative) |
| Retinal Exam | 2+ Drusen2+ Retinal Pigment Epithelium (RPE) Changes 1+ Geographic Atrophy Vessels within normal limits Retina is flat and attached 360° | 1+ Drusen 1+ Retinal Pigment Epithelium (RPE) Changes Vessels within normal limits Retina is flat and attached 360° |
| Etiology | Typical Features | Duration of Hallucinations | Triggers for Hallucinations | Insight | Associated Symptoms |
|---|---|---|---|---|---|
| Charles Bonnet Syndrome (CBS) [11,16] | Complex and detailed images of people, animals, or intricate patterns | Variable—usually minutes | Sensory deprivation | Intact | Visual impairment with either cerebrovascular disease, cortical atrophy on brain imaging, or social deprivation |
| Migraine [16] | Simple | Minutes to hours | Lack of sleep, menses, certain foods, stress | Intact | Headache, nausea, vomiting, photophobia |
| Seizures [17] | Simple | Seconds | None | Intact | Convulsions, post-ictal headache |
| Retinal Pathology [18] | Simple, such as flashing lights | Seconds | Vitreous detachment triggered usually by valsalva | Intact | Possible vision loss and abnormal fundoscopic exam |
| Parkinson’ Disease [19] | Simple or complex | Mutes | None | Variable, related to cognitive status | Parkinsonism |
| Psychiatric Illness [20] | Complex | Variable | None | Absent | Disordered thoughts, delusions |
| Alcohol Withdrawal [21] | Complex | Persistent until treated | Stopping alcohol suddenly | Impaired | Confusion, agitation |
| Narcolepsy [22] | Complex | Minutes | Falling to or awakening from sleep | Intact | Sleep disorders such as excessive daytime sleepiness, cataplexy, sleep paralysis |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bhat, S.P.; Shipchandler, A.; Tokunaga, C. Social Isolation as a Precipitating Factor for Charles Bonnet Syndrome in a Patient with Mild Visual Deterioration. Reports 2024, 7, 65. https://doi.org/10.3390/reports7030065
Bhat SP, Shipchandler A, Tokunaga C. Social Isolation as a Precipitating Factor for Charles Bonnet Syndrome in a Patient with Mild Visual Deterioration. Reports. 2024; 7(3):65. https://doi.org/10.3390/reports7030065
Chicago/Turabian StyleBhat, Shriya Prakash, Abeezar Shipchandler, and Chris Tokunaga. 2024. "Social Isolation as a Precipitating Factor for Charles Bonnet Syndrome in a Patient with Mild Visual Deterioration" Reports 7, no. 3: 65. https://doi.org/10.3390/reports7030065
APA StyleBhat, S. P., Shipchandler, A., & Tokunaga, C. (2024). Social Isolation as a Precipitating Factor for Charles Bonnet Syndrome in a Patient with Mild Visual Deterioration. Reports, 7(3), 65. https://doi.org/10.3390/reports7030065






