Leukocyte-Platelet-Rich Fibrin in Bone Regeneration after Periapical Surgery: A 30-Month Follow-Up Clinical Report
Abstract
1. Introduction
2. Case Presentation
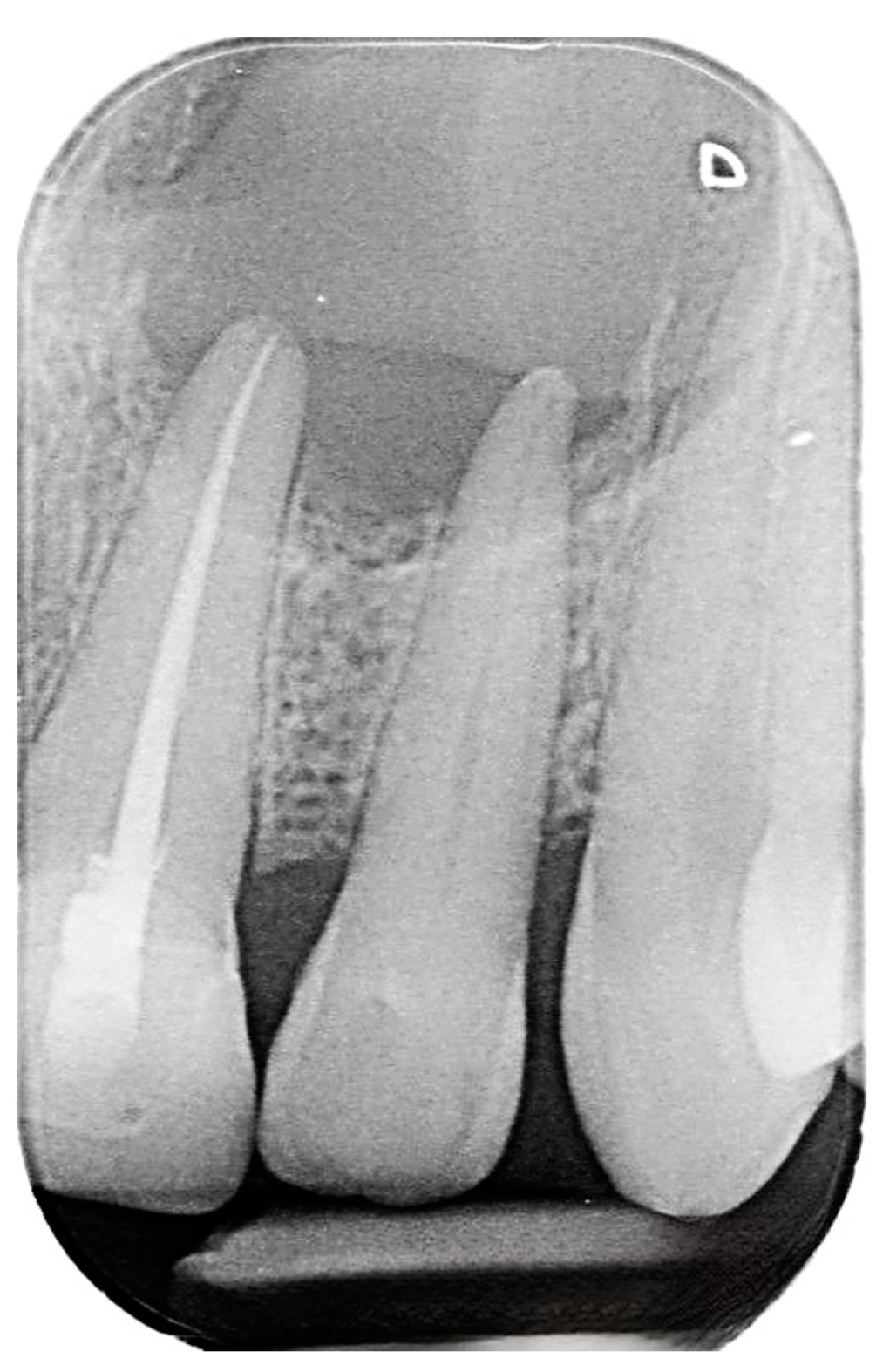
2.1. Chief Complaints History and Clinical Findings
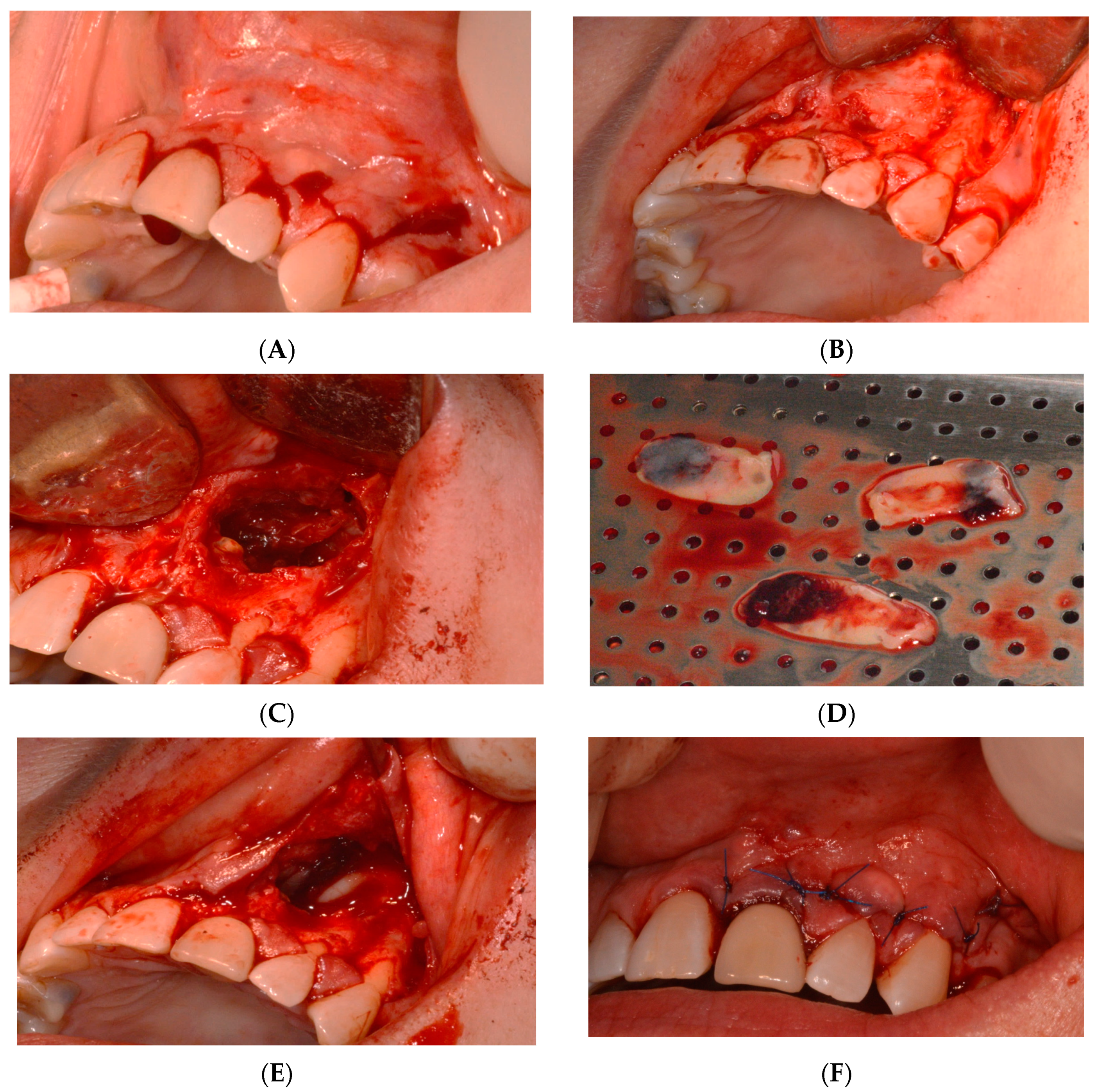
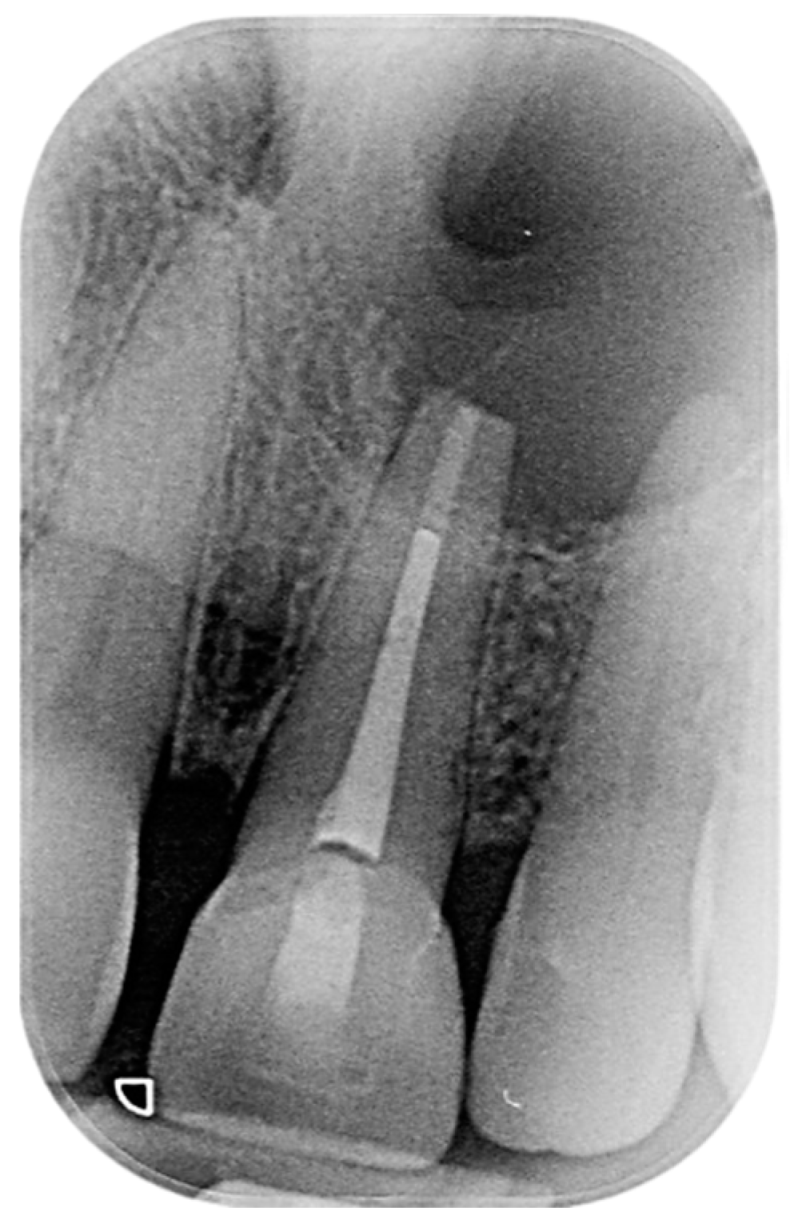
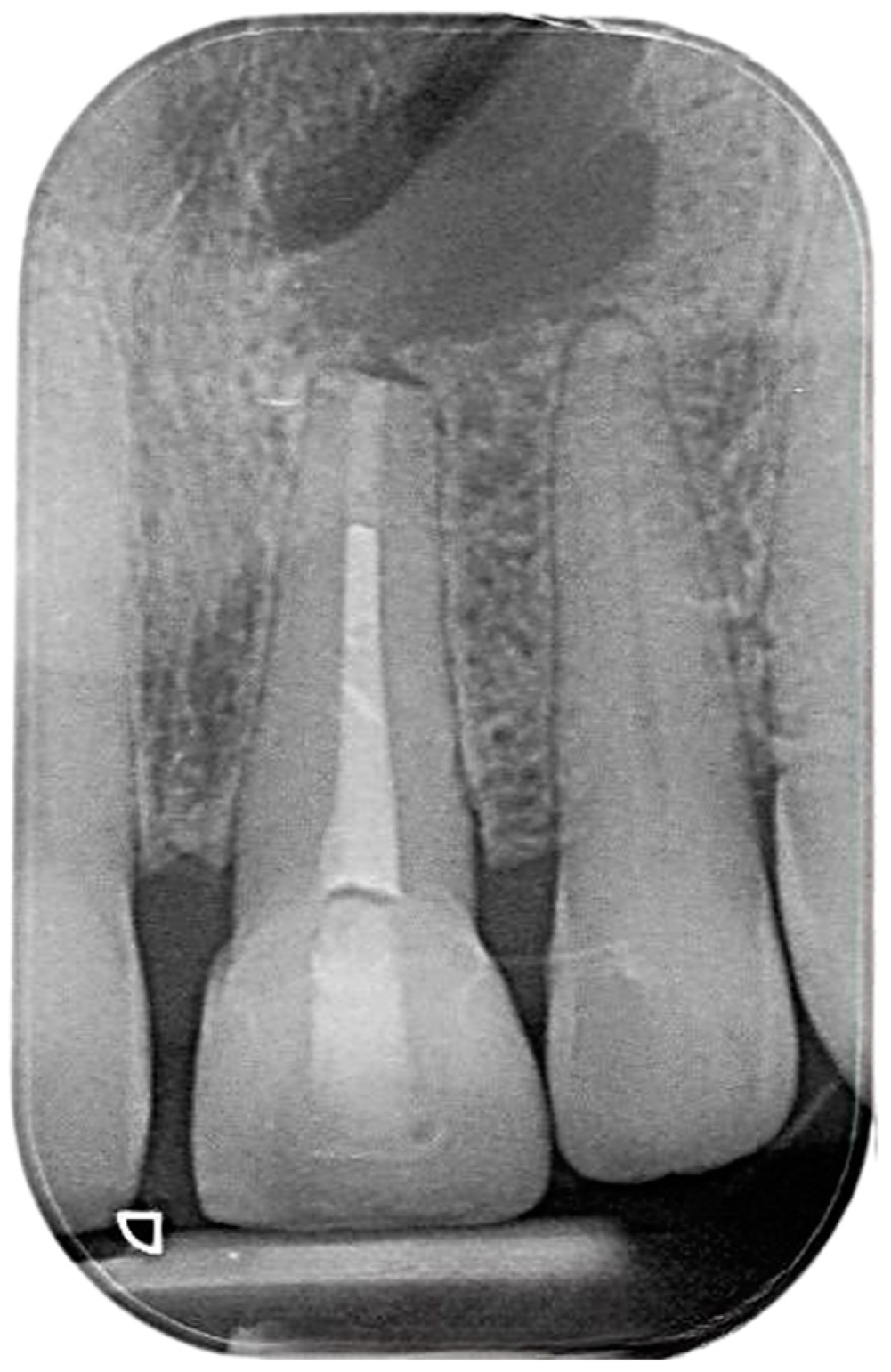
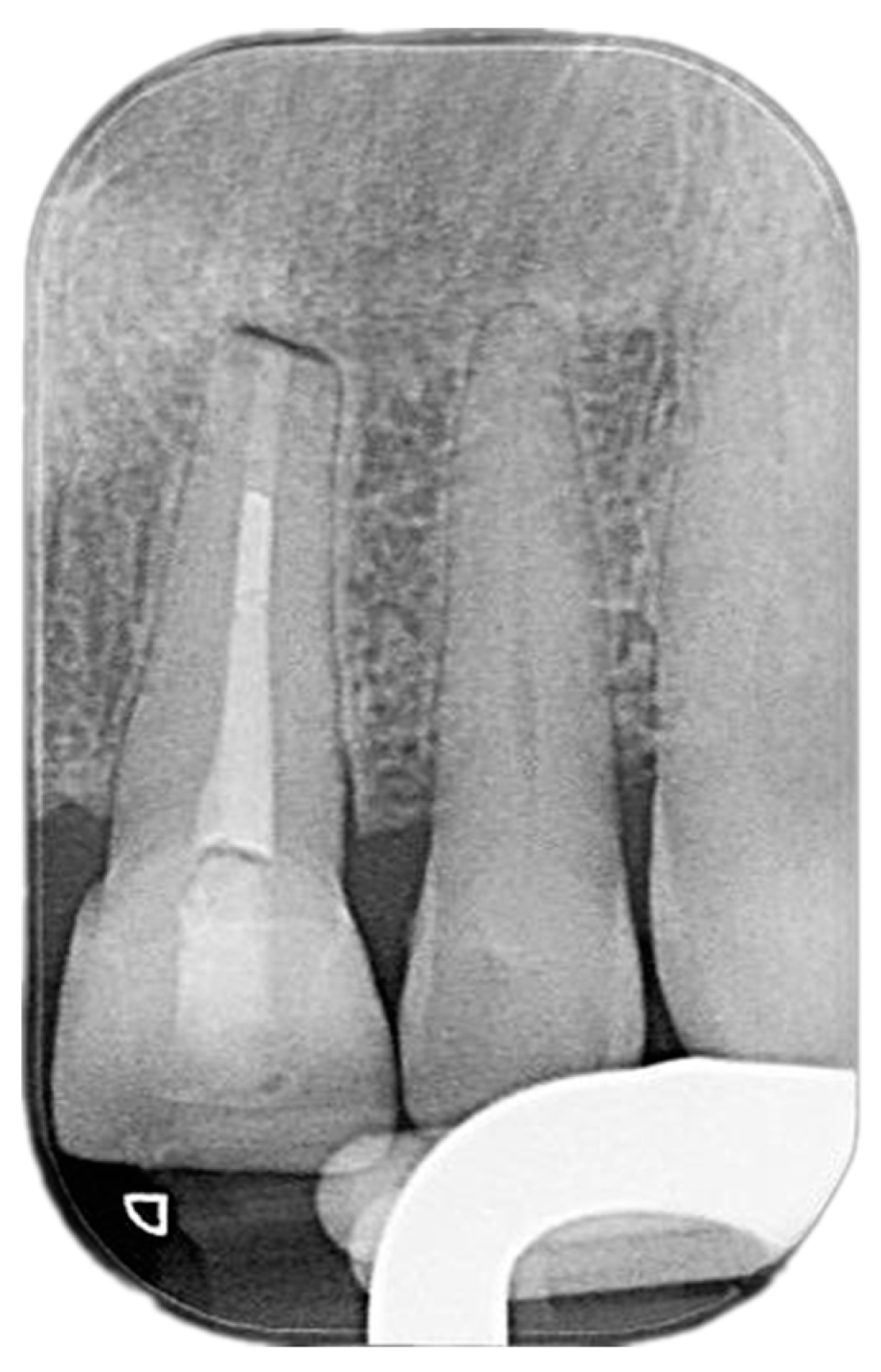
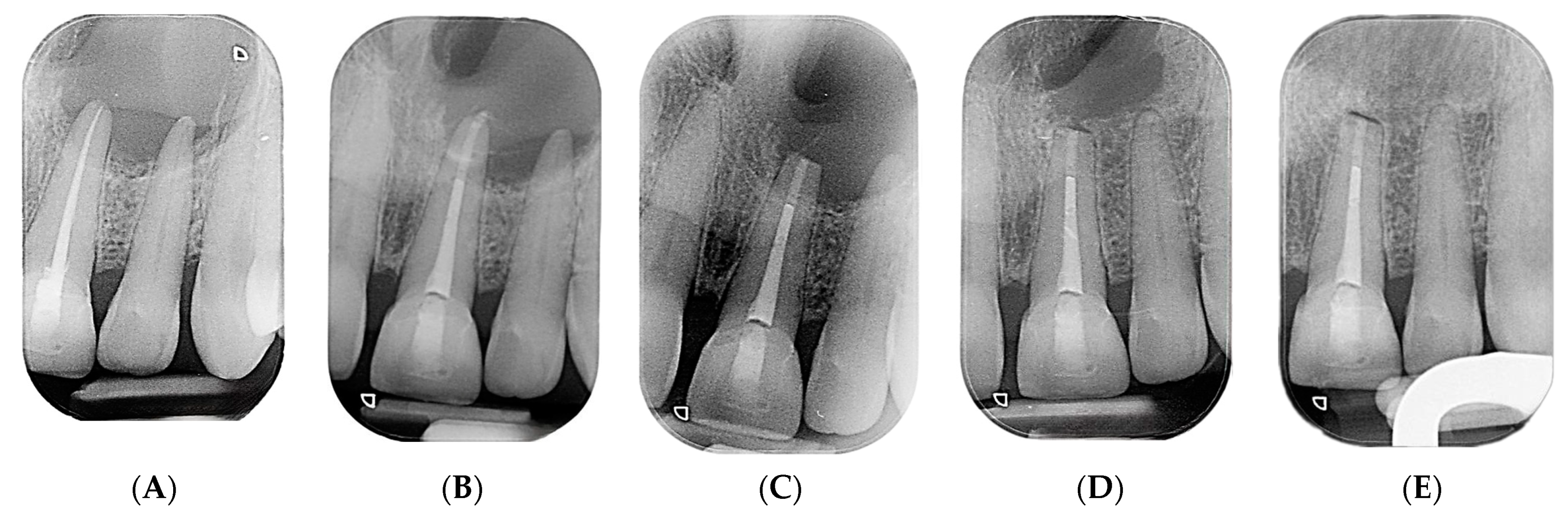
2.2. Delivery of Treatment
2.3. L’PRF Preparation
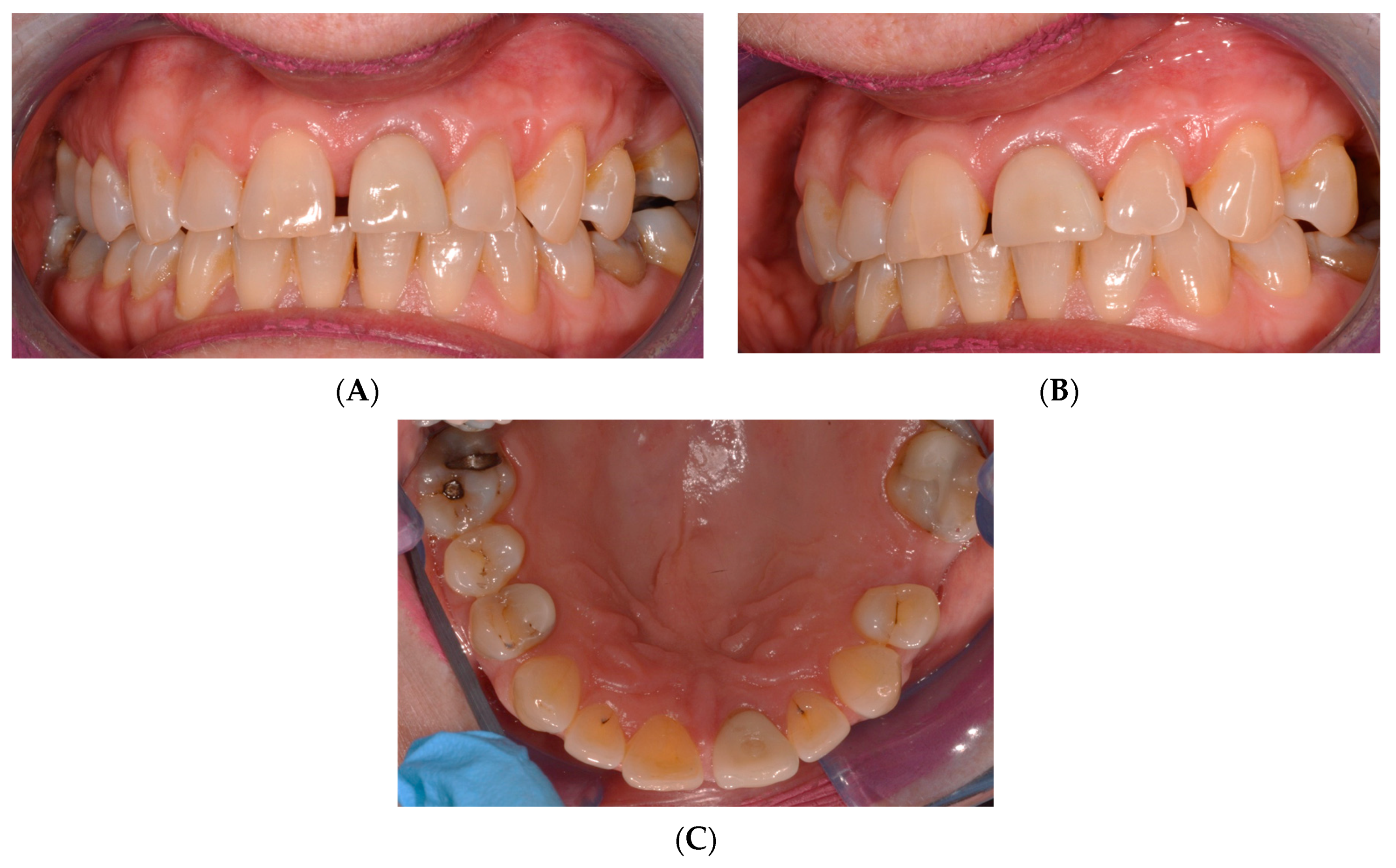
2.4. Healing of the Defect and Follow Up
3. Discussion
4. Clinical Applications
- Utilize Leukocyte-Platelet-Rich Fibrin (L’PRF) in Periapical Surgery:
- ∙
- When periapical surgery is indicated, consider using L’PRF as a biocompatible material to promote healing and bone regeneration.
- ∙
- Prepare L’PRF from the patient’s own blood to minimize the risk of rejection and infection.
- Manage Periapical Cysts with Combined Endodontic and Surgical Approaches:
- ∙
- Treat persistent periapical lesions with a combination of a root canal treatment and periapical surgery for effective management.
- ∙
- Employ modern materials like MTA for obturation and use L’PRF during apical surgery to enhance healing.
- Monitor Healing Progress with Clinical and Radiographic Follow-ups:
- ∙
- Schedule regular follow-up appointments post surgery to monitor the healing process through clinical examination and radiographs.
- ∙
- Consider annual follow-ups for up to 3 to 4 years to ensure complete healing and adhere to post-apical-surgery guidelines.
- Emphasize the Patient’s Quality of Life Post Surgery:
- ∙
- Educate the patient about the potential for improved quality of life following the use of L’PRF in periapical surgeries.
- ∙
- Inform patients that while their immediate postoperative quality of life may not significantly differ with L’PRF, its long-term benefits for bone healing are promising.
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Herrera, D.; Retamal-Valdes, B.; Alonso, B.; Feres, M. Acute periodontal lesions (periodontal abscesses and necrotizing periodontal diseases) and endo-periodontal lesions. J. Clin. Periodontol. 2018, 45, S78–S94. [Google Scholar] [CrossRef]
- Jalali, P.; Tahmasbi, M.; Augsburger, R.A.; Khalilkhani, N.K.; Daghighi, K. Dynamics of bone loss in cases with acute or chronic apical abscess. J. Endod. 2019, 45, 1114–1118. [Google Scholar] [CrossRef]
- Lieblich, S.E. Current concepts of periapical surgery. Oral Maxillofac. Surg. Clin. 2015, 27, 383–392. [Google Scholar] [CrossRef]
- Chieruzzi, M.; Rallini, M.; Pagano, S.; Eramo, S.; D’Errico, P.; Torre, L.; Kenny, J.M. Mechanical effect of static loading on endodontically treated teeth restored with fiber-reinforced posts. J. Biomed. Mater. Res. B Appl. Biomater. 2014, 102, 384–394. [Google Scholar] [CrossRef]
- Karan, N.B.; Aricioğlu, B. Assessment of bone healing after mineral trioxide aggregate and platelet-rich fibrin application in periapical lesions using cone-beam computed tomographic imaging. Clin. Oral Investig. 2020, 24, 1065–1072. [Google Scholar] [CrossRef]
- Abusrewil, S.M.; McLean, W.; Scott, J.A. The use of Bioceramics as root-end filling materials in periradicular surgery: A literature review. Saudi Dent. J. 2018, 30, 273–282. [Google Scholar] [CrossRef]
- Dragonas, P.; Katsaros, T.; Avila-Ortiz, G.; Chambrone, L.; Schiavo, J.H.; Palaiologou, A. Effects of leukocyte–platelet-rich fibrin (L-PRF) in different intraoral bone grafting procedures: A systematic review. Int. J. Oral Maxillofac. Surg. 2019, 48, 250–262. [Google Scholar] [CrossRef]
- Meschi, N.; Fieuws, S.; Vanhoenacker, A.; Strijbos, O.; Van der Veken, D.; Politis, C.; Lambrechts, P. Root-end surgery with leucocyte-and platelet-rich fibrin and an occlusive membrane: A randomized controlled clinical trial on patients’ quality of life. Clin. Oral Investig. 2018, 22, 2401–2411. [Google Scholar] [CrossRef]
- Meschi, N.; Vanhoenacker, A.; Strijbos, O.; Camargo dos Santos, B.; Rubbers, E.; Peeters, V.; Curvers, F.; Van Mierlo, M.; Geukens, A.; Fieuws, S. Multi-modular bone healing assessment in a randomized controlled clinical trial of root-end surgery with the use of leukocyte-and platelet-rich fibrin and an occlusive membrane. Clin. Oral Investig. 2020, 24, 4439–4453. [Google Scholar] [CrossRef]
- Dhiman, M.; Kumar, S.; Duhan, J.; Sangwan, P.; Tewari, S. Effect of platelet-rich fibrin on healing of apicomarginal defects: A randomized controlled trial. J. Endod. 2015, 41, 985–991. [Google Scholar] [CrossRef]
- Kavitha, M.; Krishnaveni, R.; Swathi, A.; Abubacker, M. Evaluation of Healing by Cone Beam Computed Tomography (CBCT) using Platelet-Rich Plasma (PRP)+ β-Tricalcium Phosphate (β-TCP) and Platelet Rich Fibrin (PRF)+ β-Tricalcium Phosphate (β-TCP) in Periapical Lesions: Case Report. Niger. J. Clin. Pract. 2020, 23, 1026–1029. [Google Scholar]
- Monga, P.; Grover, R.; Mahajan, P.; Keshav, V.; Singh, N.; Singh, G. A comparative clinical study to evaluate the healing of large periapical lesions using platelet-rich fibrin and hydroxyapatite. Endodontology 2016, 28, 27–31. [Google Scholar] [CrossRef]
- Singh, R.; Ismail, P.M.S.; Kambli, V.; Kumar, R.; Singh, K.D.; Kochhar, A.S.; Babaji, P. Evaluation of Hydroxyapatite Granules, CERAMENT™, and Platelet-rich Fibrin in the Management of Endodontic Apical Surgery. J. Contemp. Dent. Pract. 2020, 21, 555. [Google Scholar] [CrossRef]
- Soto-Peñaloza, D.; Peñarrocha-Diago, M.; Cervera-Ballester, J.; Peñarrocha-Diago, M.; Tarazona-Alvarez, B.; Peñarrocha-Oltra, D. Pain and quality of life after endodontic surgery with or without advanced platelet-rich fibrin membrane application: A randomized clinical trial. Clin. Oral Investig. 2020, 24, 1727–1738. [Google Scholar] [CrossRef]
- Thanikasalam, M.; Ahamed, S.; Narayana, S.S.; Bhavani, S.; Rajaraman, G. Evaluation of healing after periapical surgery using platelet-rich fibrin and nanocrystalline hydroxyapatite with collagen in combination with platelet-rich fibrin. Endodontology 2018, 30, 25–31. [Google Scholar]
- Tiwari, U.O.; Chandra, R.; Tripathi, S.; Jain, J.; Jaiswal, S.; Tiwari, R.K. Comparative analysis of platelet-rich fibrin, platelet-rich fibrin with hydroxyapatite and platelet-rich fibrin with alendronate in bone regeneration: A cone-beam computed tomography analysis. J. Conserv. Dent. JCD 2020, 23, 348. [Google Scholar]
- Moiseiwitsch, J.R.D.; Trope, M. Nonsurgical root canal therapy treatment with apparent indications for root-end surgery. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 1998, 86, 335–340. [Google Scholar] [CrossRef]
- Velvart, P. Papilla base incision: A new approach to recession-free healing of the interdental papilla after endodontic surgery. Int. Endod. J. 2002, 35, 453–460. [Google Scholar] [CrossRef]
- Abusteit, O.E.; Hosney, S.; ElSheshtawy, A.S.; Zapata, R.O. Outcome of Endodontic Treatment through Existing Full Coverage Restorations: An Endodontic Practice Case Series. J. Endod. 2022, 48, 388–395. [Google Scholar] [CrossRef]
- Torabinejad, M.; Nosrat, A.; Verma, P.; Udochukwu, O. Regenerative endodontic treatment or mineral trioxide aggregate apical plug in teeth with necrotic pulps and open apices: A systematic review and meta-analysis. J. Endod. 2017, 43, 1806–1820. [Google Scholar] [CrossRef]
- Velvart, P.; Ebner-Zimmermann, U.; Ebner, J. Comparison of long-term papilla healing following sulcular full thickness flap and papilla base flap in endodontic surgery. Int. Endod. J. 2004, 37, 687–693. [Google Scholar] [CrossRef] [PubMed]
- Whitman, D.H.; Berry, R.L.; Green, D.M. Platelet gel: An autologous alternative to fibrin glue with applications in oral and maxillofacial surgery. J. Oral Maxillofac. Surg. 1997, 55, 1294–1299. [Google Scholar] [CrossRef]
- Marx, R.E.; Carlson, E.R.; Eichstaedt, R.M.; Schimmele, S.R.; Strauss, J.E.; Georgeff, K.R. Platelet-rich plasma: Growth factor enhancement for bone grafts. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 1998, 85, 638–646. [Google Scholar] [CrossRef]
- Miron, R.J.; Zucchelli, G.; Pikos, M.A.; Salama, M.; Lee, S.; Guillemette, V.; Fujioka-Kobayashi, M.; Bishara, M.; Zhang, Y.; Wang, H.-L. Use of platelet-rich fibrin in regenerative dentistry: A systematic review. Clin. Oral Investig. 2017, 21, 1913–1927. [Google Scholar] [CrossRef]
- Lektemur Alpan, A.; Torumtay Cin, G. PRF improves wound healing and postoperative discomfort after harvesting subepithelial connective tissue graft from palate: A randomized controlled trial. Clin. Oral Investig. 2020, 24, 425–436. [Google Scholar] [CrossRef] [PubMed]
- Harrison, J.W.; Jurosky, K.A. Wound healing in the tissues of the periodontium following periradicular surgery. II. Dissectional Wound. J. Endod. 1991, 17, 544–552. [Google Scholar] [PubMed]
- Velvart, P.; Peters, C.I.; Peters, O.A. Soft tissue management: Suturing and wound closure. Endod. Top. 2005, 11, 179–195. [Google Scholar] [CrossRef]
- Chong, B.; Rhodes, J. Endodontic surgery. Br. Dent. J. 2014, 216, 281–290. [Google Scholar] [CrossRef]
- Luebke, R. Surgical endodontics. Dent. Clin. N. Am. 1974, 18, 379–391. [Google Scholar] [CrossRef]
- Lalonde, E.R.; Luebke, R.G. The frequency and distribution of periapical cysts and granulomas: An evaluation of 800 specimens. Oral Surg. Oral Med. Oral Pathol. 1968, 25, 861–868. [Google Scholar] [CrossRef]
- Alqutaibi, A.Y.; Aboalrejal, A. Zygomatic implants are a reliable treatment option for patients with atrophic maxilla. J. Evid. Based Dent. Pract. 2017, 17, 402–404. [Google Scholar] [CrossRef] [PubMed]
- Alqutaibi, A.Y.; Alnazzawi, A.A.; Algabri, R.; Aboalrejal, A.N.; AbdElaziz, M.H. Clinical performance of single implant-supported ceramic and metal-ceramic crowns: A systematic review and meta-analysis of randomized clinical trials. J. Prosthet. Dent. 2021, 126, 369–376. [Google Scholar] [CrossRef] [PubMed]
- Moustafa Ali, R.M.; Alqutaibi, A.Y.; El-Din Gomaa, A.S.; Abdallah, M.F. Effect of Submerged vs Nonsubmerged Implant Placement Protocols on Implant Failure and Marginal Bone Loss: A Systematic Review and Meta-Analysis. Int. J. Prosthodont. 2018, 31, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Alqutaibi, A.Y.; Radi, I.A.-E. No clear evidence regarding the effect of osteoporosis on dental implant failure. J. Evid. Based Dent. Pract. 2016, 16, 124–126. [Google Scholar] [CrossRef] [PubMed]
- Abdalla, R.I.B.; Alqutaibi, A.Y.; Kaddah, A. Does the adjunctive use of platelet-rich plasma to bone graft during sinus augmentation reduce implant failure and complication? Systematic review and meta-analysis. Quintessence Int. 2018, 4, 139. [Google Scholar]
- Sinsareekul, C.; Saengthong-Aram, P.; Limpuangthip, N. Survival, complications, and patient-reported outcomes of endodontically treated teeth versus dental implant-supported prostheses: A systematic review. J. Prosthet. Dent. 2024. [Google Scholar] [CrossRef]
- Grande, F.; Pozzan, M.C.; Marconato, R.; Mollica, F.; Catapano, S. Evaluation of load distribution in a mandibular model with four implants depending on the number of prosthetic screws used for OT-bridge system: A finite element analysis (FEA). Materials 2022, 15, 7963. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Qurban, H.A.; Hamadallah, H.H.; Madkhaly, M.A.; Hakeem, M.M.; Alqutaibi, A.Y. Leukocyte-Platelet-Rich Fibrin in Bone Regeneration after Periapical Surgery: A 30-Month Follow-Up Clinical Report. Reports 2024, 7, 32. https://doi.org/10.3390/reports7020032
Qurban HA, Hamadallah HH, Madkhaly MA, Hakeem MM, Alqutaibi AY. Leukocyte-Platelet-Rich Fibrin in Bone Regeneration after Periapical Surgery: A 30-Month Follow-Up Clinical Report. Reports. 2024; 7(2):32. https://doi.org/10.3390/reports7020032
Chicago/Turabian StyleQurban, Hatim A., Hatem Hazzaa Hamadallah, Mohammad A. Madkhaly, Muhannad M. Hakeem, and Ahmed Yaseen Alqutaibi. 2024. "Leukocyte-Platelet-Rich Fibrin in Bone Regeneration after Periapical Surgery: A 30-Month Follow-Up Clinical Report" Reports 7, no. 2: 32. https://doi.org/10.3390/reports7020032
APA StyleQurban, H. A., Hamadallah, H. H., Madkhaly, M. A., Hakeem, M. M., & Alqutaibi, A. Y. (2024). Leukocyte-Platelet-Rich Fibrin in Bone Regeneration after Periapical Surgery: A 30-Month Follow-Up Clinical Report. Reports, 7(2), 32. https://doi.org/10.3390/reports7020032






