Abstract
Situs inversus totalis (SIT) is a congenital anomaly that involves the mirror rearrangement of the thoracic and abdominal internal organs. In this paper, we report a 56-year-old male patient with previously confirmed SIT, who was admitted to the hospital for the diagnosis and surgical treatment of non-small-cell lung cancer, located in the sixth right pulmonary segment. The patient underwent segmentectomy with mediastinal and hilar lymphadenectomy. Furthermore, we screened the PubMed and Embase databases for reports of the surgical treatment of patients with SIT and lung cancer. Articles describing inoperable and disseminated disease, as well as patients qualified for palliative treatment, were not included. Ultimately, we compared 21 articles (including the one described here). Data about the clinical condition, tumor characteristics, treatment, and histopathological examination were extracted and summarized.
1. Introduction
Situs inversus totalis (SIT) is a congenital anomaly that involves the mirror rearrangement of the thoracic and abdominal internal organs [1]. SIT is an uncommon abnormality, with its prevalence ranging from 1:6500 to 1:25,000 [2]. In contrast, lung cancer is one of the most common neoplastic diseases and is responsible for the highest cancer-related death rate [3]. Lung cancer in patients with SIT is extremely rare, mostly published in single case reports [4]. Moreover, the documentation of several such cases in one center is unique. The aim of this article is to report a third patient with SIT and lung cancer treated surgically in the authors’ center. Furthermore, there is an attempt to gather similar case reports published in the literature, and to describe diagnostic difficulties and management strategies for these patients.
2. Detailed Case Description
A 56-year-old man with previously confirmed SIT was admitted to the Thoracic Surgery and Transplantation Department in January 2014 due to a 2.5 cm tumor of unknown etiology in the right lung, detected in a chest X-ray. The patient did not present any clinical symptoms. The image of SIT was confirmed in a contrast-enhanced chest computed tomography (CT). In addition, CT confirmed a 28 × 22 mm tumor in the sixth right segment, with a 9 mm satellite tumor located slightly higher, with enlargement of the mediastinal lymph nodes (Figure 1). Positron emission tomography FDG-PET/CT and endobronchial ultrasound (EBUS) were inaccessible during hospitalization. The diagnosis procedure was extended with an ultrasound fine needle aspiration biopsy of the right lung tumor and left supraclavicular lymph node with a diameter of 6 mm. Lung tumor biopsy was ineffective and cancer cells were not observed in the supraclavicular lymph node biopsy specimen, although the high level of carcinoembryonic antigen CEA (95.3 ng/mL) suggested adenocarcinoma in stage N2. A bronchofiberoscopy showed the right side of the lobar opening segmental bronchi anatomy in a configuration typical of the left lung, and an analogous image on the left side, where the bronchial configuration of the lobar openings’ segmental bronchi anatomy corresponded to the right lung. Subsequently, the patient qualified for surgery via right thoracotomy. Intraoperatively, the correct anatomy of the left lung (bilobar lung) on the right side and the tumor in the sixth segment, corresponding to the chest CT, was found; however, the posterior part of interlobar fissure was undeveloped. The entire anatomy of the mediastinum also corresponded to the left side, including the nodal station of the aorto-pulmonary window. Intraoperative examination confirmed metastases to the nodes of groups 5 and 7 and the procedure was limited to the sixth segmentectomy with mediastinal and lung hilar lymphadenectomy. The surgical technique was based on reconstructing the posterior part of the interlobar fissure by scissor stapling and ligation of the artery and vein to segment VI, followed by the linear stapler resection of segment VI.
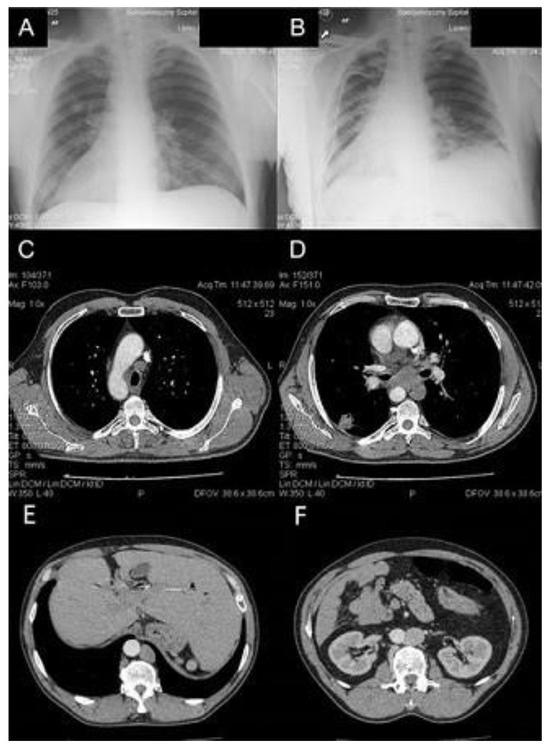
Figure 1.
(A,B) Pre- and postoperative chest X-rays of the patient with SIT and lung cancer. (C,D) Chest CT showing rearrangement of mediastinal vessels and 2.5 cm tumor in VI right segment with enlargement of lymph nodes 4R and 7. (E,F) Abdominal CT showing position of the liver on the left side and position of the aorta on the right side.
Finally, the diagnosis of adenocarcinoma G2 and partially (approximately 20%) adenocarcinoma micropapillary G3 was established in the T1bN2Mx/IIIA stage. The postoperative course was uneventful. The patient underwent adjuvant chemo- and radiotherapy and died after 12 months due to metastatic brain spread.
3. Discussion
Situs anomalies are associated with the abnormal positioning of internal organs. Situs ambiguous refers to the improper position of one or several organs within the chest or abdomen (situs inversus incomplete syndrome). In contrast, situs inversus totalis (SIT) is a mirror rearrangement of the normal state (situs solitus) [1]. It is considered that the first reports of situs anomalies in humans were described in 17th century [5] Many studies have investigated the underlying genetics of SIT and found that several mutations might contribute to the development of this abnormality, including CFAP45, NME7, and DNAH11, among many others [6,7,8,9]. Patients with SIT or other laterality abnormalities often have an additional condition, named primary ciliary dyskinesia (PCD), which is associated with bronchiectasis. Indeed, SIT, bronchiectasis, and chronic sinusitis have collectively been described as Kartagener syndrome [10]. The occurrence of situs inversus in PCD patients is approximately 40% to 50% [11,12]. Pulmonary resection in a patient with Kartagener syndrome due to symptomatic bronchiectasis has also been described [13]. Patients with Kartagener syndrome may develop end-stage respiratory failure, which requires lung transplantation. Vascular and bronchial asymmetry between a recipient with situs inversus and a donor represents a technical challenge [14].
To the best of our knowledge, there are only 20 cases in medical databases that refer to patients with SIT and lung cancer treated surgically, with the operative verification of an inverted lung anatomy. The found cases with their characteristics are presented in Table 1.

Table 1.
Characteristics of included patients. NR—not reported; VATS—video-assisted thoracoscopic surgery; RATS—robot-assisted thoracoscopic surgery.
In all the SIT and lung cancer operated cases, a mirror and typical anatomy were described, which supports the constant nature of the SIT anatomical rule, although there may be isolated changes in the number of segmental vessels, enlargement of the bronchial arteries with Kartagener syndrome cases, or massive infiltration requiring pneumonectomy [18,33]. This observation does not apply to situs inversus incomplete syndrome [35,36]. According to the mirror lung and mediastinum image, the largest challenge was the surgeon’s dexterity and reaction to the inverted anatomy. In our material, the layout of the operating team was typical. All maneuvers in the operational field were according to the rules for the opposing side. Segmental and main pulmonary vessels, lobar fissures, and bronchi based on a regular anatomy were supplied according to the technique used in the center (staplers, ligatures, electrocoagulation, etc.). Depending on the case, diagnostic procedures included bronchofiberoscopies, which visualized the reversed anatomy of the bronchial tree, and transbronchial and percutaneous transthoracic biopsies. Furthermore, surgery was often used for both diagnostic and curative purposes. Among the collected data, surgical procedures involved wedge resections (two patients), segmentectomies (five patients), lobectomies (twelve patients), bilobectomy (one patient), and pneumonectomy in two cases (one case had two operating methods). Open procedures (thoracotomy and median sternotomy) were performed in nine patients. A minimally invasive approach was used in the case of 12 patients, including one robotic-assisted procedure. Only eight studies reported a follow-up (6 months–2 years). The majority of cases were described in the eastern part of the world [15,18,19,21,22,24,25,26,28,29,30,31,33,34]. Surprisingly, the presence of as many as three such cases was observed in Szczecin, in Europe.
Lung cancer is one of the most common malignant diseases, but coexistence with SIT is not frequent. Coexisting lung cancer, SIT, and Kartagener syndrome is an even rarer observation [18,33]. The diagnosis of SIT is based on radiology. First, lung cancer and SIT cases are imaged only by X-ray [15]. Currently, radiological imaging based on X-ray, contrast-enhanced chest CT, and FDG-PET/CT is combined as 3D-CT, which allows the more accurate preoperative identification of the vascular and bronchial system [35]. The complex anatomy in SIT is a difficulty in the preoperative planning of thoracic procedures. Therefore, 3D-CT images were described in several included articles [28,29,33,34]. It is important to remember potential metastasis. PET/CT is an accurate method of determining such information, especially in non-small-cell lung cancer (NSCLC) patients, and a tissue biopsy should be performed even in uncommon metastasis locations [37].
The inverted but regular anatomy of SIT cases enabled the use of a typical surgical technique and even allowed the introduction of minimally invasive procedures. According to this observation, lobectomies and segmentectomies performed by the VATS technique have already been documented [38,39]. Robotic thoracic procedures are relatively novel and have gained much popularity recently. These procedures include early-stage lung cancer resections as well as complex procedures, such as sleeve resections [40,41]. Yang and colleagues recently published the first report of a lung cancer patient with SIT treated with robot-assisted lobectomy [28]. Furthermore, contemporary emphasis has been directed towards quantitative proteomics and its use in biomarker identification. MIC-A/B, FASLG, and HGF have gained prominence as indicators for the radical resection of NSCLC [42]. The combination of advanced surgical techniques with the development of biochemistry may be the future of lung cancer surgery.
4. Conclusions
To conclude, lung cancer may develop in SIT patients with a chance for surgery. Preoperative planning should be based on contrast-enhanced chest CT and FDG-PET/CT, combined with three-dimensional CT for the more accurate preoperative identification of the vascular and bronchial system. The CT mirror image has to be confirmed by bronchofiberoscopy. The analysis of the literature indicates that in cases of lung cancer with SIT, a normal, albeit inverted, lung anatomy can be counted on, which may be helpful in planning surgical treatment, especially in minimally invasive surgeries.
Author Contributions
Conceptualization, J.W. and T.G.; formal analysis, D.K. and K.K.; investigation, J.W., T.G., J.P., N.W. and M.E.W.; resources, J.W., T.G., J.P., N.W. and M.E.W.; writing—original draft preparation, J.W., T.G., J.P., N.W., D.K., K.K., M.M., S.B., P.B. and M.E.W.; writing—review and editing, J.W., T.G., J.P., N.W., D.K., K.K., M.M., S.B., P.B. and M.E.W.; visualization, J.W., T.G., J.P., N.W., D.K., K.K., M.M., S.B., P.B. and M.E.W.; supervision, J.W. and M.E.W. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was approved by IRB of the Pomeranian Medical University (KB.006.93.2023).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available in this article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Applegate, K.E.; Goske, M.J.; Pierce, G.; Murphy, D. Situs revisited: Imaging of the heterotaxy syndrome. Radiographics 1999, 19, 837–852, discussion 853–834. [Google Scholar] [CrossRef] [PubMed]
- Eitler, K.; Bibok, A.; Telkes, G. Situs Inversus Totalis: A Clinical Review. Int. J. Gen. Med. 2022, 15, 2437–2449. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics, 2022. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef]
- Wójcik, J.; Grodzki, T.; Bielewicz, M.; Wojtyś, M.; Kubisa, B.; Pieróg, J.; Wójcik, N. Lung cancer in situs inversus totalis (SIT)—Literature review. Adv. Med. Sci. 2013, 58, 1–8. [Google Scholar] [CrossRef]
- Blegen, H.M. Surgery in Situs Inversus. Ann. Surg. 1949, 129, 244–259. [Google Scholar] [CrossRef] [PubMed]
- Dougherty, G.W.; Mizuno, K.; Nöthe-Menchen, T.; Ikawa, Y.; Boldt, K.; Ta-Shma, A.; Aprea, I.; Minegishi, K.; Pang, Y.P.; Pennekamp, P.; et al. CFAP45 deficiency causes situs abnormalities and asthenospermia by disrupting an axonemal adenine nucleotide homeostasis module. Nat. Commun. 2020, 11, 5520. [Google Scholar] [CrossRef]
- Reish, O.; Aspit, L.; Zouella, A.; Roth, Y.; Polak-Charcon, S.; Baboushkin, T.; Benyamini, L.; Scheetz, T.E.; Mussaffi, H.; Sheffield, V.C.; et al. A Homozygous Nme7 Mutation Is Associated with Situs Inversus Totalis. Hum. Mutat. 2016, 37, 727–731. [Google Scholar] [CrossRef]
- Bartoloni, L.; Blouin, J.L.; Pan, Y.; Gehrig, C.; Maiti, A.K.; Scamuffa, N.; Rossier, C.; Jorissen, M.; Armengot, M.; Meeks, M.; et al. Mutations in the DNAH11 (axonemal heavy chain dynein type 11) gene cause one form of situs inversus totalis and most likely primary ciliary dyskinesia. Proc. Natl. Acad. Sci. USA 2002, 99, 10282–10286. [Google Scholar] [CrossRef]
- Deng, H.; Xia, H.; Deng, S. Genetic basis of human left-right asymmetry disorders. Expert. Rev. Mol. Med. 2015, 16, e19. [Google Scholar] [CrossRef]
- Leigh, M.W.; Pittman, J.E.; Carson, J.L.; Ferkol, T.W.; Dell, S.D.; Davis, S.D.; Knowles, M.R.; Zariwala, M.A. Clinical and genetic aspects of primary ciliary dyskinesia/Kartagener syndrome. Genet. Med. 2009, 11, 473–487. [Google Scholar] [CrossRef]
- Noone, P.G.; Leigh, M.W.; Sannuti, A.; Minnix, S.L.; Carson, J.L.; Hazucha, M.; Zariwala, M.A.; Knowles, M.R. Primary ciliary dyskinesia: Diagnostic and phenotypic features. Am. J. Respir. Crit. Care Med. 2004, 169, 459–467. [Google Scholar] [CrossRef] [PubMed]
- Barber, A.T.; Shapiro, A.J.; Davis, S.D.; Ferkol, T.W.; Atkinson, J.J.; Sagel, S.D.; Dell, S.D.; Olivier, K.N.; Milla, C.E.; Rosenfeld, M.; et al. Laterality Defects in Primary Ciliary Dyskinesia: Relationship to Ultrastructural Defect or Genotype. Ann. Am. Thorac. Soc. 2023, 20, 397–405. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.; Cao, Z.; Zhao, X.; Ye, Q. Left middle lobectomy for bronchiectasis in a patient with Kartagener syndrome: A case report. J. Cardiothorac. Surg. 2016, 11, 37. [Google Scholar] [CrossRef]
- Gauthier, J.M.; Takahashi, T.; Bierhals, A.J.; Brody, S.L.; Hachem, R.R.; Witt, C.A.; Byers, D.E.; Yusen, R.D.; Trulock, E.P.; Aguilar, P.R.; et al. Technical Considerations for Lung Transplantation in Kartagener’s Syndrome. Ann. Thorac. Surg. 2019, 107, e337–e339. [Google Scholar] [CrossRef] [PubMed]
- Kodama, K.; Doi, O.; Tatsuta, M. Situs inversus totalis and lung cancer. Chest 1990, 97, 1274–1275. [Google Scholar] [CrossRef] [PubMed]
- Subotich, D.; Mandarich, D.; Katchar, V.; Bulajich, B.; Drndarski, B. Lung resection for primary bronchial carcinoma in a patient with complete situs inversus. Clin. Anat. 2006, 19, 358–362. [Google Scholar] [CrossRef]
- Bielewicz, M.; Wojtyś, M.; Witkowska, D.; Alchimowicz, J.; Wójcik, J.; Grodzki, T. Non-small cell lung cancer in patient with visceral total inversion. Pneumonol. Alergol. Pol. 2009, 77, 200–204. [Google Scholar] [CrossRef]
- Inoue, Y.; Suga, A.; Sekido, Y.; Yamada, S.; Iwazaki, M. A case of surgically resected lung cancer in a patient with Kartagener’s syndrome. Tokai J. Exp. Clin. Med. 2011, 36, 21–24. [Google Scholar]
- Shimizu, J.; Arano, Y.; Adachi, I.; Morishita, M.; Fuwa, B.; Saitoh, M.; Minato, H. Adenosquamous carcinoma of the lung in a patient with complete situs inversus. Ann. Thorac. Cardiovasc. Surg. 2011, 17, 178–181. [Google Scholar] [CrossRef][Green Version]
- Wójcik, J.; Kubisa, B.; Pieróg, J.; Bielewicz, M.; Wójcik, N.; Kaseja, K.; Grodzki, T. Lung Cancer in Situs Inversus Totalis (SIT)—A Case Report. Kardiochir. Torakochir. Pol. 2012, 2, 219–221. [Google Scholar]
- Yoshida, M.; Hino, H.; Machida, H.; Hatakeyama, N.; Okano, Y.; Iwahara, Y.; Shinohara, T.; Oogushi, F. Video-assisted thoracic surgery lobectomy for lung cancer in a patient with complete situs inversus. Gen. Thorac. Cardiovasc. Surg. 2013, 61, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Lin, F.; Yang, M.; Guo, C.; Liu, L. Lung cancer mimicking aortic dissecting aneurysm in a patient with situs inversus totalis. Thorac. Cancer 2016, 7, 254–256. [Google Scholar] [CrossRef] [PubMed]
- Grapatsas, K.; Piyis, A.; Neofotistos, K.; Tsilogianni, Z.; Zarogoulidis, P.; Paliouras, D.; Gogakos, A.; Barbetakis, N.; Organtzis, J.; Kioumis, I.; et al. A patient with situs inversus totalis and lung cancer-a rare combination. Ann. Transl. Med. 2016, 4, 450. [Google Scholar] [CrossRef] [PubMed]
- Juma, A.N.; Wang, Y.Q.; Chen, Y.; Peng, X.; Zhou, Y.; Zhuang, W. Lobectomy for lung cancer by video-assisted thoracic surgery in situs inversus. Asian Cardiovasc. Thorac. Ann. 2017, 25, 219–221. [Google Scholar] [CrossRef] [PubMed]
- Ye, M.; Shen, J.; Kong, M.; Lin, J.; Li, X.; Chen, B. Video-assisted thoracoscopic surgery right upper lobectomy in a situs inversus totalis patient. J. Thorac. Dis. 2017, 9, E1018–E1020. [Google Scholar] [CrossRef]
- Matsui, T.; Mizuno, K.; Yamada, T. Video-assisted thoracoscopic bisegmentectomies for double primary lung cancers in a patient with situs inversus totalis. Gen. Thorac. Cardiovasc. Surg. 2018, 66, 671–674. [Google Scholar] [CrossRef]
- Gonzalez-Rivas, D.; Soultanis, K.; Zheng, H.; Zhu, Y. Situs inversus uniportal video-assisted thoracoscopic right anatomic segmentectomy S1–S2 and S6. J. Thorac. Dis. 2018, 10, E383–E386. [Google Scholar] [CrossRef]
- Kanayama, M.; Inoue, M.; Yoshida, J.; Tanaka, F. Thoracoscopic Lung Lobectomy for a Lung Cancer Patient with Situs Inversus Totalis. J. UOEH 2018, 40, 237–241. [Google Scholar] [CrossRef][Green Version]
- Wu, Y.J.; Bao, Y.; Wang, Y.L. Thoracoscopic segmentectomy assisted by three-dimensional computed tomography bronchography and angiography for lung cancer in a patient living with situs inversus totalis: A case report. World J. Clin. Cases 2019, 7, 3844–3850. [Google Scholar] [CrossRef]
- Zhu, T.; Chen, Z.H.; Tang, S.; Yang, X.J.; Fang, S.; Deng, H.J. Primary pulmonary lymphoepithelioma-like carcinoma combined with situs inversus totalis. Chin. Med. J. 2019, 132, 223–226. [Google Scholar] [CrossRef]
- Chen, L.J.; Qiu, X.; Sun, H.; Xu, P.F.; Yin, F.M.; Xu, L.J. Two types of lung cancer with situs inversus totalis: A case report and review of the literature. J. Int. Med. Res. 2020, 48, 300060520944107. [Google Scholar] [CrossRef]
- Celik, A.; Sayan, M. Videothoracoscopic Left Upper Lobectomy for Lung Cancer in a Case of Situs Inversus Totalis. Cureus 2021, 13, e16217. [Google Scholar] [CrossRef] [PubMed]
- Zhou, D.; Tian, Y.; Lu, Y.; Yang, X. Anatomical variants of pulmonary segments and uni-portal thoracoscopic segmentectomy for lung cancer in a patient with Kartagener syndrome: A case report. Gen. Thorac. Cardiovasc. Surg. 2021, 69, 1432–1437. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.; Jin, W.; Fan, X.; Zheng, L.; Wang, H.; Wang, Q. Robotic-assisted pulmonary lobectomy with lung cancer in a patient with situs inversus totalis. J. Cardiothorac. Surg. 2022, 17, 221. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Xu, D.; Cheng, B.; Tang, L.; Chen, Z.; Du, L. A Case Report of Pulmonary Artery Sling and Situs Inversus Incompletes. Medicine 2021, 100, e24021. [Google Scholar] [CrossRef]
- Del Prete, A.; Cavaliere, C.; Di Pietto, F.; De Ritis, R. Situs Inversus with Levocardia, Infrahepatic Interruption of the Inferior Vena Cava, and Azygos Continuation: A Case Report. Surg. Radiol. Anat. 2015, 38, 369–371. [Google Scholar] [CrossRef]
- Cha, H.K.; Lim, J.H.; Ryu, W.K.; Kim, L.; Ryu, J.-S. Solitary Uncommon Metastasis in Non-Small Cell Lung Cancer. Reports 2023, 6, 8. [Google Scholar] [CrossRef]
- Sihoe, A.D.L. Video-assisted thoracoscopic surgery as the gold standard for lung cancer surgery. Respirology 2020, 25 (Suppl. 2), 49–60. [Google Scholar] [CrossRef]
- Hireche, K.; Lounes, Y.; Bacri, C.; Solovei, L.; Marty-Ané, C.; Canaud, L.; Alric, P. VATS versus Open Lobectomy Following Induction Therapy for Stage III NSCLC: A Propensity Score-Matched Analysis. Cancers 2023, 15, 414. [Google Scholar] [CrossRef]
- Manfredini, B.; Zirafa, C.C.; Romano, G.; Bagalà, E.; Cariello, C.; Davini, F.; Melfi, F. Intraoperative Catastrophes during Robotic Lung Resection: A Single-Center Experience and Review of the Literature. Life 2023, 13, 215. [Google Scholar] [CrossRef]
- Rocha Júnior, E.; Terra, R.M. Robotic lung resection: A narrative review of the current role on primary lung cancer treatment. J. Thorac. Dis. 2022, 14, 5039–5055. [Google Scholar] [CrossRef] [PubMed]
- Bodén, E.; Andreasson, J.; Hirdman, G.; Malmsjö, M.; Lindstedt, S. Quantitative Proteomics Indicate Radical Removal of Non-Small Cell Lung Cancer and Predict Outcome. Biomedicines 2022, 10, 2738. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).