Muscle Activation in Older Females after a Community-Based Resistance Training Program: A Pilot Study
Abstract
:1. Introduction
2. Methods
2.1. Inclusion and Exclusion Criteria
2.2. Study Design
2.3. Exercise Training
2.4. The sEMG Protocol
2.5. Statistical Analysis
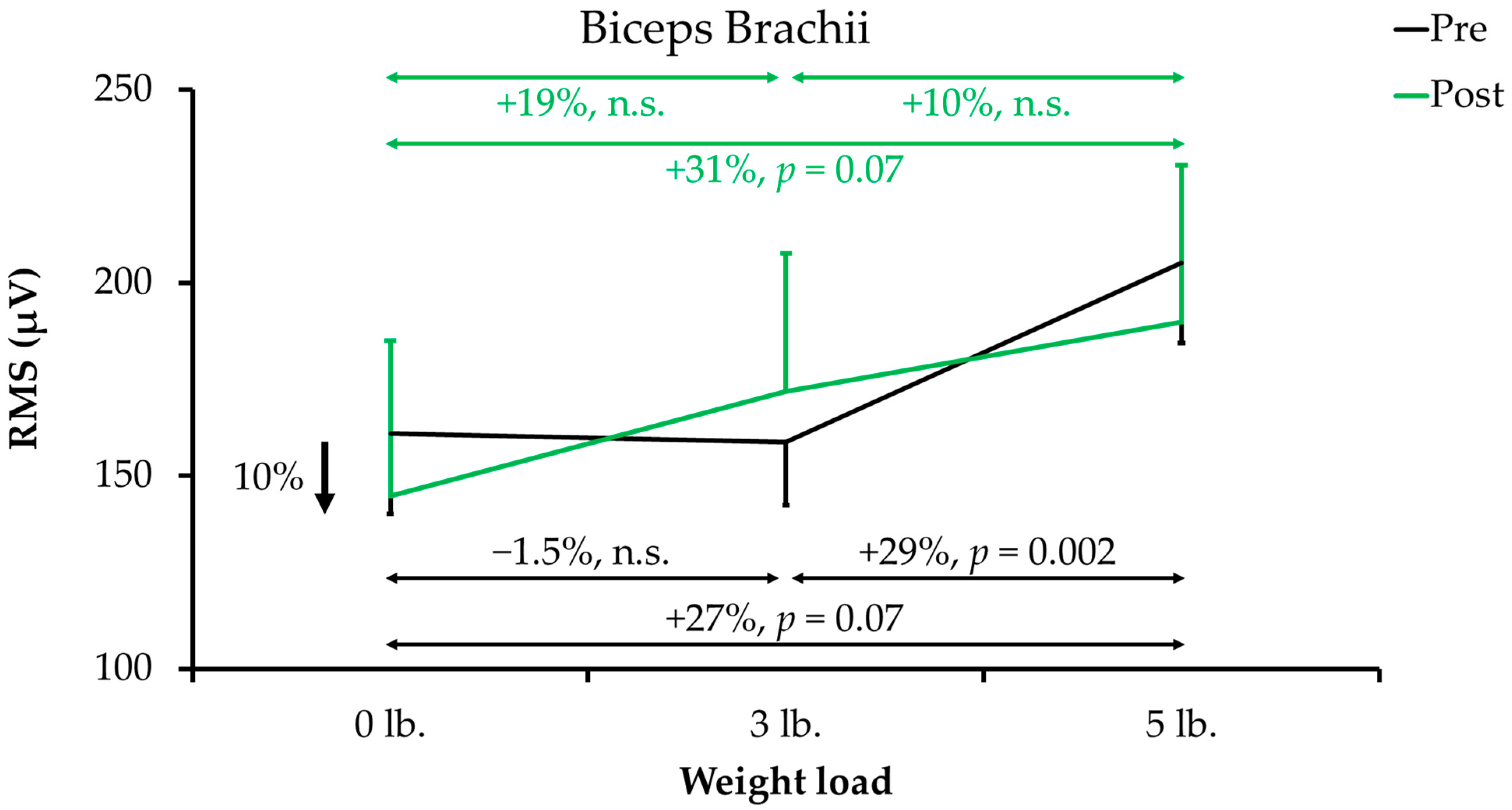
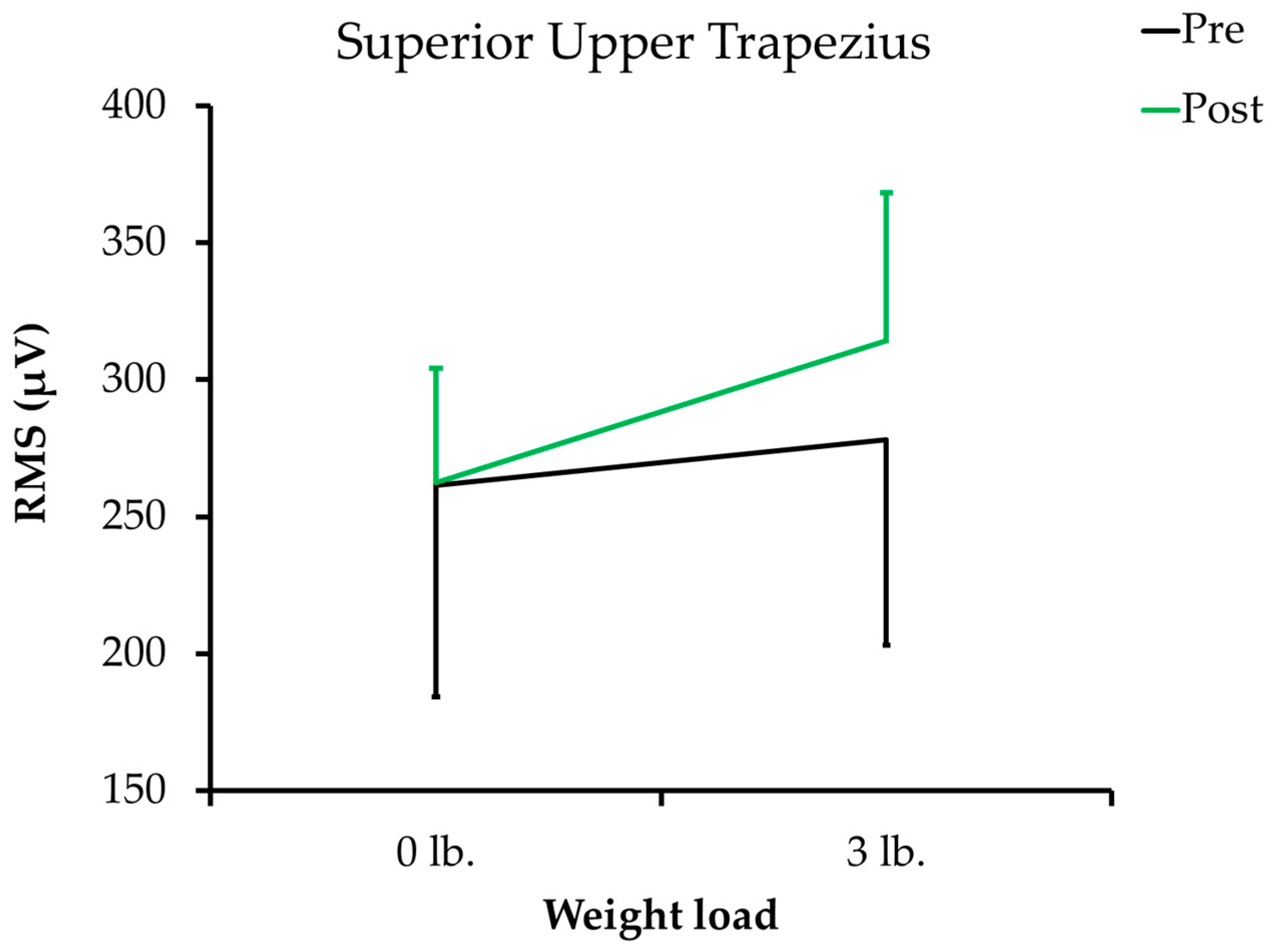
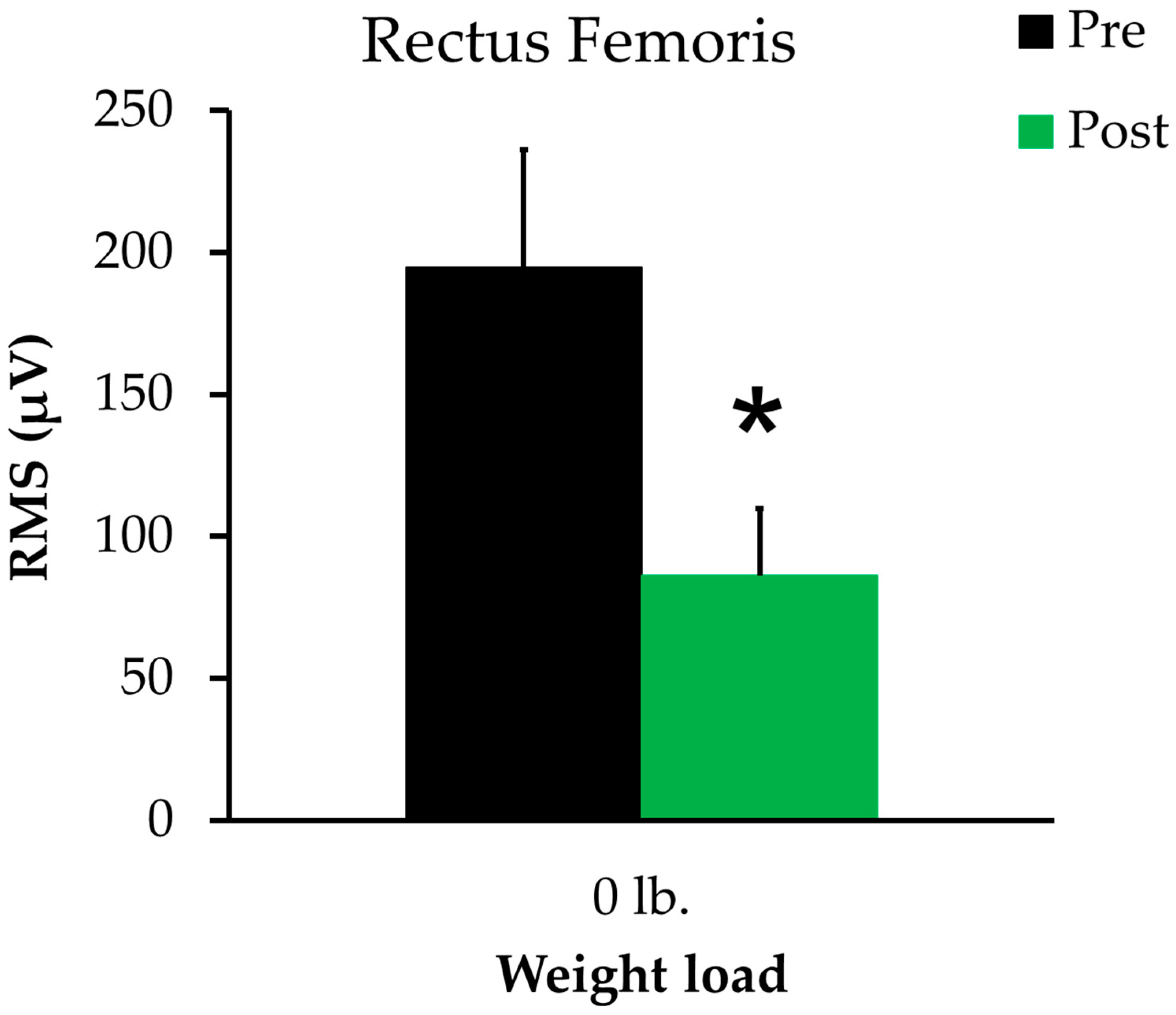
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yamada, H.; Okada, M.; Oda, T.; Nemoto, S.; Shiozaki, T.; Kizuka, T.; Kuno, S.; Masuda, T. Effects of aging on EMG variables during fatiguing isometric contractions. J. Hum. Ergol. 2000, 29, 7–14. [Google Scholar]
- Cecílio, F.A.; Regalo, S.C.H.; Palinkas, M.; Issa, J.P.M.; Siéssere, S.; Hallak, J.E.C.; Machado-De-Sousa, J.P.; Semprini, M. Ageing and surface EMG activity patterns of masticatory muscles. J. Oral Rehabil. 2010, 37, 248–255. [Google Scholar] [CrossRef] [PubMed]
- Moreland, J.D.; Richardson, J.A.; Goldsmith, C.H.; Clase, C.M. Muscle Weakness and Falls in Older Adults: A Systematic Review and Meta-Analysis. J. Am. Geriatr. Soc. 2004, 52, 1121–1129. [Google Scholar] [CrossRef] [PubMed]
- McLean, R.R.; Shardell, M.D.; Alley, D.E.; Cawthon, P.M.; Fragala, M.S.; Harris, T.B.; Kenny, A.M.; Peters, K.W.; Ferrucci, L.; Guralnik, J.M.; et al. Criteria for Clinically Relevant Weakness and Low Lean Mass and Their Longitudinal Association with Incident Mobility Impairment and Mortality: The Foundation for the National Institutes of Health (FNIH) Sarcopenia Project. J. Gerontol. Ser. A 2014, 69, 576–583. [Google Scholar] [CrossRef]
- Morse, C.I.; Thom, J.; Mian, O.; Birch, K.; Narici, M.V. Gastrocnemius specific force is increased in elderly males following a 12-month physical training programme. Graefe’s Arch. Clin. Exp. Ophthalmol. 2006, 100, 563–570. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, Y.; Ueyasu, Y.; Yamashita, Y.; Akagi, R. Effects of 4 Weeks of Explosive-type Strength Training for the Plantar Flexors on the Rate of Torque Development and Postural Stability in Elderly Individuals. Int. J. Sports Med. 2016, 37, 470–475. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reichert, T.; Bagatini, N.C.; Simmer, N.M.; Meinerz, A.P.; Barroso, B.M.; Prado, A.K.G.; Delevatti, R.; Costa, R.R.; Kanitz, A.C.; Kruel, L.F.M. Effects of Different Models of Water-Based Resistance Training on Muscular Function of Older Women. Res. Q. Exerc. Sport 2019, 90, 46–53. [Google Scholar] [CrossRef] [PubMed]
- Emerson, N.S.; Stout, J.R.; Fukuda, D.H.; Robinson, E.H.; Iv; Scanlon, T.C.; Beyer, K.S.; Fragala, M.S.; Hoffman, J.R. Resistance training improves capacity to delay neuromuscular fatigue in older adults. Arch. Gerontol. Geriatr. 2015, 61, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Cadore, E.L.; Pinto, R.S.; Pinto, S.S.; Alberton, C.L.; Correa, C.S.; Tartaruga, M.P.; Silva, E.M.; Almeida, A.P.V.; Trindade, G.T.; Kruel, L.F.M. Effects of Strength, Endurance, and Concurrent Training on Aerobic Power and Dynamic Neuromuscular Economy in Elderly Men. J. Strength Cond. Res. 2011, 25, 758–766. [Google Scholar] [CrossRef] [PubMed]
- Ploutz, L.L.; Tesch, P.A.; Biro, R.L.; Dudley, G.A. Effect of resistance training on muscle use during exercise. J. Appl. Physiol. 1994, 76, 1675–1681. [Google Scholar] [CrossRef]
- Crowe, E.M.; Ball, S.D. Effectiveness of Advanced Stay Strong, Stay Healthy in Community Settings. Gerontol. Geriatr. Med. 2015, 1, 2333721415596462. [Google Scholar] [CrossRef]
- Ball, S.; Gammon, R.; Kelly, P.J.; Cheng, A.-L.; Chertoff, K.; Kaume, L.; Abreu, E.L.; Brotto, M. Outcomes of Stay Strong, Stay Healthy in Community Settings. J. Aging Health 2013, 25, 1388–1397. [Google Scholar] [CrossRef] [PubMed]
- Baker, B.S.; Weitzel, K.J.; Royse, L.; Miller, K.; Guess, T.M.; Ball, S.D.; Duren, D.L. Efficacy of an 8-Week Resistance Training Program in Older Adults: A Randomized Controlled Trial. J. Aging Phys. Act. 2021, 29, 121–129. [Google Scholar] [CrossRef]
- Syed-Abdul, M.M.; Peterson, E.C.; Mills-Gray, S.L.; Parks, E.J.; Ball, S.D. Stay Strong, Stay Healthy. Med. Sci. Sports Exerc. 2016, 48, 125. [Google Scholar] [CrossRef]
- Syed-Abdul, M.M.; Mills-Gray, S.L.; Parks, E.J.; Ball, S.D. Acute effects of incremental resistance training on muscle function in older adults. FASEB J. 2017, 31 (Suppl. 1), 1020.11. [Google Scholar]
- Syed-Abdul, M.M.; McLellan, C.L.; Parks, E.J.; Ball, S.D. Effects of incremental resistance training program on quality of life in older adults. Int. J. Exerc. Sci. 2017, 11, 44. [Google Scholar]
- Syed-Abdul, M.M.; McClellan, C.L.; Parks, E.J.; Ball, S.D. Effects of a resistance training community programme in older adults. Ageing Soc. 2021, 1–16. [Google Scholar] [CrossRef]
- PHAC and CSEP, Physical Activity Readiness Questionnaire (PAR-Q). In Public Health Agency of Canada and the Canadian Society for Exercise Physiology. 2002. Available online: https://geriatrictoolkit.missouri.edu/his/Par-Q.pdf (accessed on 14 October 2021).
- Warren, G.L.; Hermann, K.M.; Ingalls, C.P.; Masselli, M.R.; Armstrong, R.B. Decreased EMG median frequency during a second bout of eccentric contractions. Med. Sci. Sports Exerc. 2000, 32, 820–829. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, S.S.M.; Miara, M.D.B.; Arnold, A.S.; Biewener, A.A.; Wakeling, J.M. Recruitment of faster motor units is associated with greater rates of fascicle strain and rapid changes in muscle force during locomotion. J. Exp. Biol. 2013, 216, 198–207. [Google Scholar] [CrossRef] [Green Version]
- Syed-Abdul, M.M.; Soni, D.S.; Miller, W.M.; Johnson, R.J.; Barnes, J.T.; Pujol, T.J.; Wagganer, J.D. Traditional Versus Suspended Push-up Muscle Activation in Athletes and Sedentary Women. J. Strength Cond. Res. 2018, 32, 1816–1820. [Google Scholar] [CrossRef]
- Fiebert, I.M.; Spielholz, N.I.; Applegate, E.; Fox, C.; Jaro, J.; Joel, L.; Raper, L. Comparison of EMG activity of medial and lateral hamstrings during isometric contractions at various cuff weight loads. Knee 2001, 8, 145–150. [Google Scholar] [CrossRef]
- Lane, C.L.; Hardwick, D.; Janus, T.P.; Chen, H.; Lu, Y.; Mayer, J.M. Comparison of the firefighter candidate physical ability test to weight lifting exercises using electromyography. Work 2019, 62, 459–467. [Google Scholar] [CrossRef]
- Daniels, R.J.; Cook, S.B. Effect of instructions on EMG during the bench press in trained and untrained males. Hum. Mov. Sci. 2017, 55, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Dicus, J.R.; Holmstrup, M.E.; Shuler, K.T.; Rice, T.T.; Raybuck, S.D.; Siddons, C.A. Stability of Resistance Training Implement alters EMG Activity during the Overhead Press. Int. J. Exerc. Sci. 2018, 11, 708–716. [Google Scholar] [PubMed]
- Vigotsky, A.D.; Halperin, I.; Lehman, G.J.; Trajano, G.; Vieira, T.M. Interpreting Signal Amplitudes in Surface Electromyography Studies in Sport and Rehabilitation Sciences. Front. Physiol. 2018, 8, 985. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oliveira, A.D.S.C.; Gonçalves, M. EMG amplitude and frequency parameters of muscular activity: Effect of resistance training based on electromyographic fatigue threshold. J. Electromyogr. Kinesiol. 2009, 19, 295–303. [Google Scholar] [CrossRef]
- Horlings, C.G.; Van Engelen, B.G.; Allum, J.H.; Bloem, B.R. A weak balance: The contribution of muscle weakness to postural instability and falls. Nat. Clin. Pract. Neurol. 2008, 4, 504–515. [Google Scholar] [CrossRef] [PubMed]
| Upper-Body Exercises | Lower-Body Exercises |
|---|---|
|
|
| Exercise Class # | Sets of Reps | Weights | Single-Leg Exercises |
|---|---|---|---|
| 1 | 1 set of 5 repetitions (1 × 5) | No weights | Alternate legs each repetition (R,L,R,L,R,L,R,L,R,L) |
| 2 | 2 × 5 | No weights | Alternate legs each rep |
| 3 | 2 × 6 | No weights | Alternate legs each rep |
| 4 | 2 × 6 | Add weights | Alternate legs each rep |
| 5 | 2 × 8 | With weights | Alternate legs each rep |
| 6 | 2 × 10 | With weights | Alternate legs each rep |
| 7 | 2 × 10 | With weights | Alternate legs each rep |
| 8 | 2 × 10 | With weights | Alternate legs each set (1 × 10 R; 1 × 10 L, repeat) |
| 9 | 2 × 10 | With weights | Alternate legs each set |
| 10 | 2 × 10 | With weights | Alternate legs each set |
| 11 | 2 × 10 | With weights | No alternating (2 × 10 R; 2 × 10 L) |
| 12 | 2 × 10 | With weights | No alternating |
| 13 | 2 × 10 | 1–2 adaptations with weights | No alternating |
| 14 | 2 × 10 | Same adaptations with weights | No alternating |
| 15 | 2 × 10 | 1–2 new adaptations with weights | No alternating |
| 16 | 2 × 10 | Same adaptations with weights | No alternating |
| Anthropometrics (n = 7) | Baseline a | Change | p-Value | ||||
|---|---|---|---|---|---|---|---|
| Age (years) | 61.1 | ± | 1.5 | ||||
| Height (meters) | 1.66 | ± | 0.03 | ||||
| Weight (kg) | 83.5 | ± | 6.6 | −1.8 | ± | 0.5 | 0.008 |
| Body mass index (kg/m2) | 30.2 | ± | 2.0 | −1.8 | ± | 0.5 | 0.013 |
| Body fat b | |||||||
| Total body fat (kg) | 33.9 | ± | 3.6 | −0.81 | ± | 0.36 | 0.063 |
| Total body fat (%) | 40.2 | ± | 1.5 | −0.09 | ± | 0.04 | 0.075 |
| Body lean mass c | |||||||
| Total lean (kg) | 46.8 | ± | 2.6 | −0.46 | ± | 0.20 | 0.058 |
| Total lean (%) | 57.0 | ± | 1.4 | −0.60 | ± | 0.29 | 0.310 |
| Trunk lean (%) | 29.2 | ± | 1.0 | −0.17 | ± | 0.38 | 0.757 |
| Left arm lean (%) | 2.4 | ± | 0.1 | −0.01 | ± | 0.03 | 0.961 |
| Right arm lean (%) | 2.8 | ± | 0.1 | −0.08 | ± | 0.05 | 0.184 |
| Left leg lean (%) | 9.5 | ± | 0.2 | −0.17 | ± | 0.19 | 0.360 |
| Right leg lean (%) | 9.7 | ± | 0.3 | −0.07 | ± | 0.20 | 0.821 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Syed-Abdul, M.M.; Ball, S.D. Muscle Activation in Older Females after a Community-Based Resistance Training Program: A Pilot Study. Reports 2021, 4, 38. https://doi.org/10.3390/reports4040038
Syed-Abdul MM, Ball SD. Muscle Activation in Older Females after a Community-Based Resistance Training Program: A Pilot Study. Reports. 2021; 4(4):38. https://doi.org/10.3390/reports4040038
Chicago/Turabian StyleSyed-Abdul, Majid Mufaqam, and Stephen D. Ball. 2021. "Muscle Activation in Older Females after a Community-Based Resistance Training Program: A Pilot Study" Reports 4, no. 4: 38. https://doi.org/10.3390/reports4040038
APA StyleSyed-Abdul, M. M., & Ball, S. D. (2021). Muscle Activation in Older Females after a Community-Based Resistance Training Program: A Pilot Study. Reports, 4(4), 38. https://doi.org/10.3390/reports4040038






