Tear Liquid for Predictive Diagnosis of Alzheimer’s Disease
Abstract
:1. Introduction
2. Materials and Methods
2.1. Methods
2.2. Materials
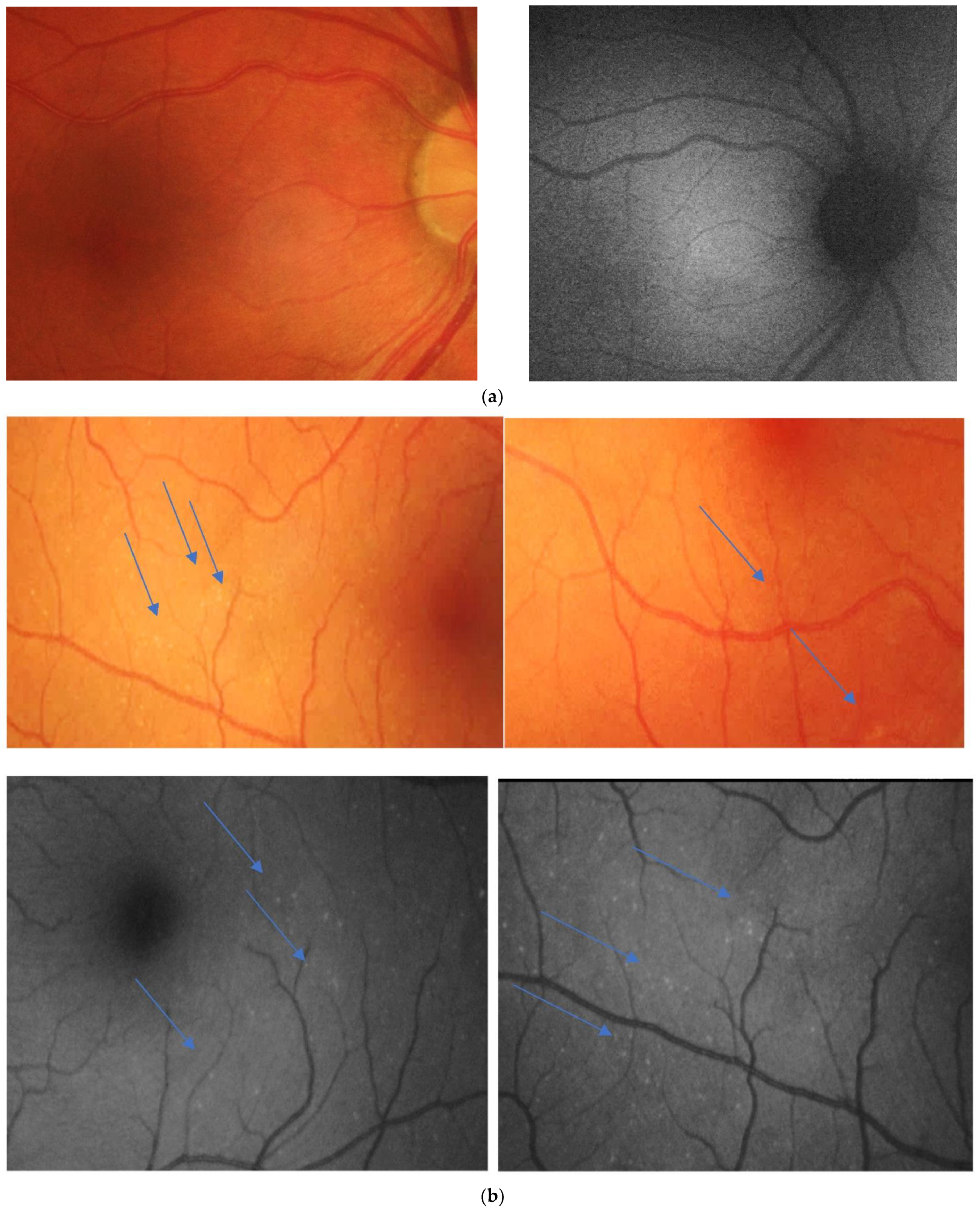
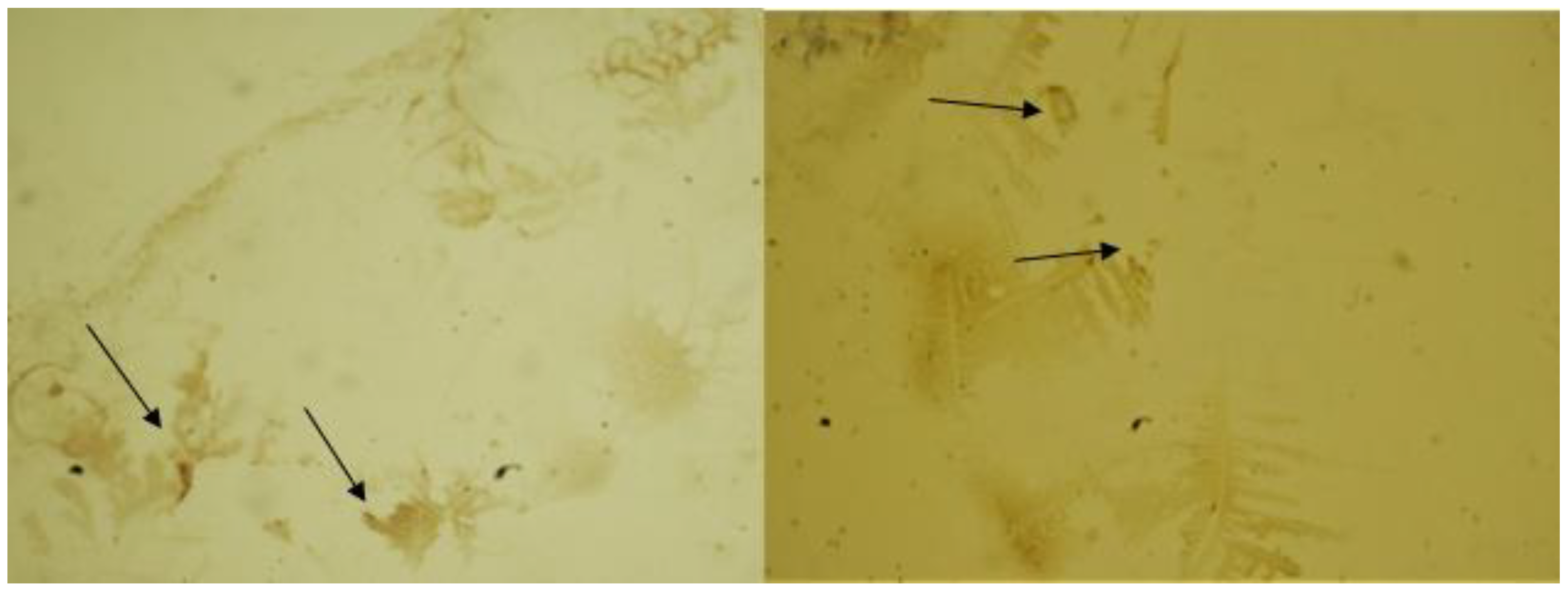
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Ethics Approval
References
- Hagan, S.; Martin, E.; Enríquez-De-Salamanca, A. Tear fluid biomarkers in ocular and systemic disease: Potential use for predictive, preventive and personalised medicine. EPMA J. 2016, 7, 15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Börger, M.; Funke, S.; Bähr, M.; Grus, F.; Lingor, P. Biomarker sources for Parkinson’s disease: Time to shed tears? Basal Ganglia 2015, 5, 63–69. [Google Scholar] [CrossRef]
- Rusciano, G.; Zito, G.; Pesce, G.; Del Prete, S.; Cennamo, G.; Sasso, A. Assessment of conjunctival microvilli abnormality by micro-Raman analysis—By G. Rusciano et al. J. Biophotonics 2016, 9, 551–559. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van Setten, G.; Nilsson, L.; Hahne, S.; Jhonston, A.; Kvanta, A.; Gandy, S.; Naslund, J.; Nordstedt, C. b-amyloid protein precursor expression in lacrimal glands and tears fluid. Investig. Opthalmol. Vis. Sci. 1996, 37, 13. [Google Scholar]
- Yu, X.; Hayden, E.Y.; Xia, M.; Liang, O.; Cheah, L.; Teplow, D.B.; Xie, Y.-H. Surface enhanced Raman spectroscopy distinguishes amyloid Β-protein isoforms and conformational states. Protein Sci. 2018, 27, 1427–1438. [Google Scholar] [CrossRef] [PubMed]
- Lue, L.-F.; Kuo, Y.-M.; Roher, A.E.; Brachova, L.; Shen, Y.; Sue, L.; Beach, T.; Kurth, J.H.; Rydel, R.E.; Rogers, J. Soluble Amyloid β Peptide Concentration as a Predictor of Synaptic Change in Alzheimer’s Disease. Am. J. Pathol. 1999, 155, 853–862. [Google Scholar] [CrossRef]
- McLean, C.A.; Cherny, R.A.; Fraser, F.W.; Fuller, S.J.; Smith, M.J.; Beyreuther, K.; Bush, A.I.; Masters, C.L. Soluble pool of Abeta amyloid as a determinant of severity of neurodegeneration in Alzheimer’s disease. Ann. Neurol. 1999, 46, 860–866. [Google Scholar]
- Colligris, P.; De Lara, M.J.P.; Colligris, B.; Pintor, J. Ocular Manifestations of Alzheimer’s and Other Neurodegenerative Diseases: The Prospect of the Eye as a Tool for the Early Diagnosis of Alzheimer’s Disease. J. Ophthalmol. 2018, 2018, 8538573. [Google Scholar] [CrossRef] [PubMed]
- Roda, M.; Ciavarella, C.; Giannaccare, G.; Versura, P. Biomarkers in Tears and Ocular Surface: A Window for Neurodegenerative Diseases. Eye Contact Lens 2020, 46, S129–S134. [Google Scholar] [CrossRef] [PubMed]
- Camerlingo, C.; Lisitskiy, M.; Lepore, M.; Portaccio, M.; Montorio, D.; Del Prete, S.; Cennamo, G. Characterization of Human Tear Fluid by Means of Surface-Enhanced Raman Spectroscopy. Sensors 2019, 19, 1177. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hart, N.; Koronyo, Y.; Black, K.L.; Koronyo-Hamaoui, M. Ocular indicators of Alzheimer’s: Exploring disease in the retina. Acta Neuropathol. 2016, 132, 767–787. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kalló, G.; Emri, M.; Varga, Z.; Ujhelyi, B.; Tőzsér, J.; Csutak, A.; Csősz, É. Changes in the Chemical Barrier Composition of Tears in Alzheimer’s Disease Reveal Potential Tear Diagnostic Biomarkers. PLoS ONE 2016, 11, e0158000. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sundelöf, J.; Giedraitis, V.; Irizarry, M.C.; Sundström, J.; Ingelsson, E.; Rönnemaa, E.; Ärnlöv, J.; Gunnarsson, M.D.; Hyman, B.T.; Basun, H.; et al. Plasma β Amyloid and the Risk of Alzheimer Disease and Dementia in Elderly Men. Arch. Neurol. 2008, 65, 256–263. [Google Scholar] [CrossRef] [PubMed] [Green Version]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Del Prete, S.; Marasco, D.; Sabetta, R.; Del Prete, A.; Marino, F.Z.; Franco, R.; Troisi, S.; Troisi, M.; Cennamo, G. Tear Liquid for Predictive Diagnosis of Alzheimer’s Disease. Reports 2021, 4, 26. https://doi.org/10.3390/reports4030026
Del Prete S, Marasco D, Sabetta R, Del Prete A, Marino FZ, Franco R, Troisi S, Troisi M, Cennamo G. Tear Liquid for Predictive Diagnosis of Alzheimer’s Disease. Reports. 2021; 4(3):26. https://doi.org/10.3390/reports4030026
Chicago/Turabian StyleDel Prete, Salvatore, Daniela Marasco, Rosalaura Sabetta, Antonio Del Prete, Federica Zito Marino, Renato Franco, Salvatore Troisi, Mario Troisi, and Gilda Cennamo. 2021. "Tear Liquid for Predictive Diagnosis of Alzheimer’s Disease" Reports 4, no. 3: 26. https://doi.org/10.3390/reports4030026
APA StyleDel Prete, S., Marasco, D., Sabetta, R., Del Prete, A., Marino, F. Z., Franco, R., Troisi, S., Troisi, M., & Cennamo, G. (2021). Tear Liquid for Predictive Diagnosis of Alzheimer’s Disease. Reports, 4(3), 26. https://doi.org/10.3390/reports4030026







