Observations on Four Cases of Brooke–Spiegler Syndrome
Abstract
1. Introduction
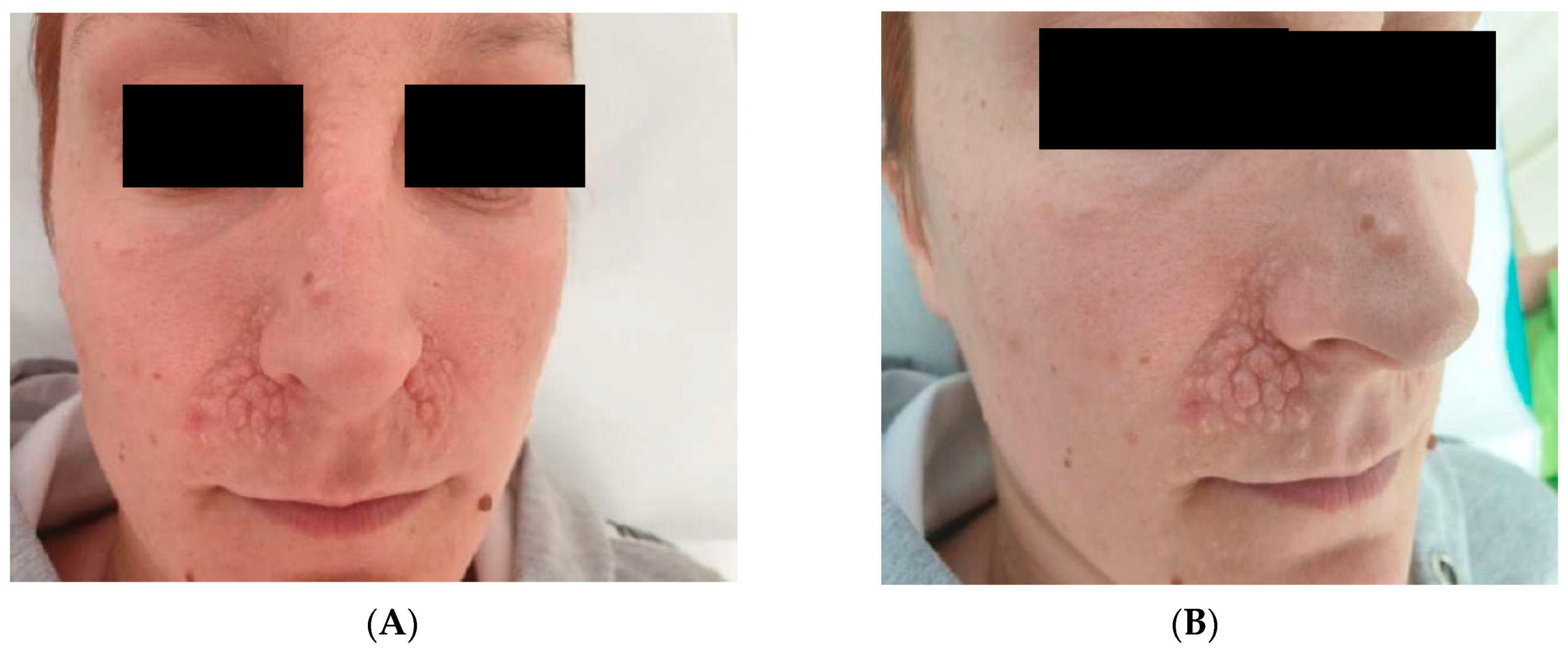
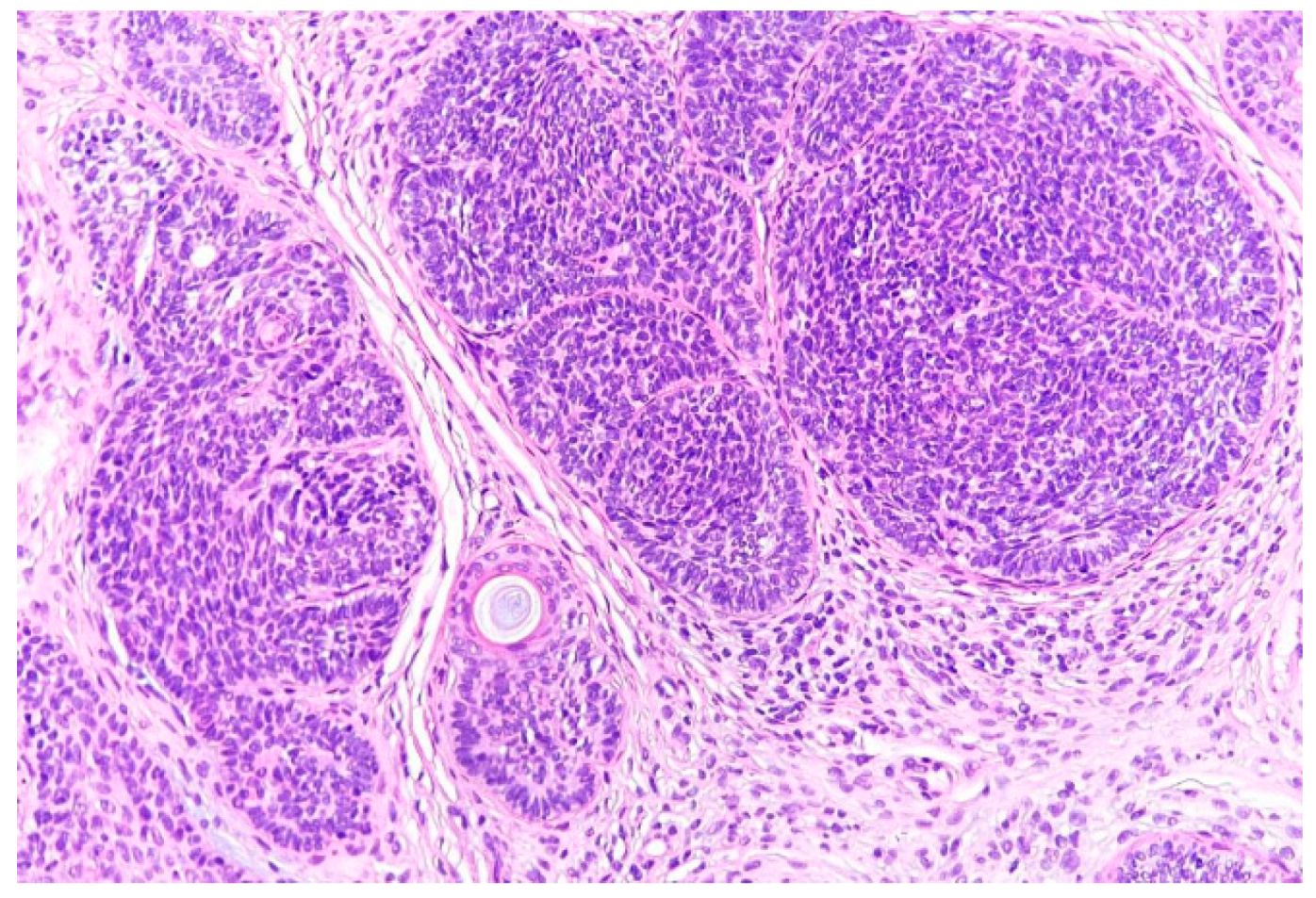
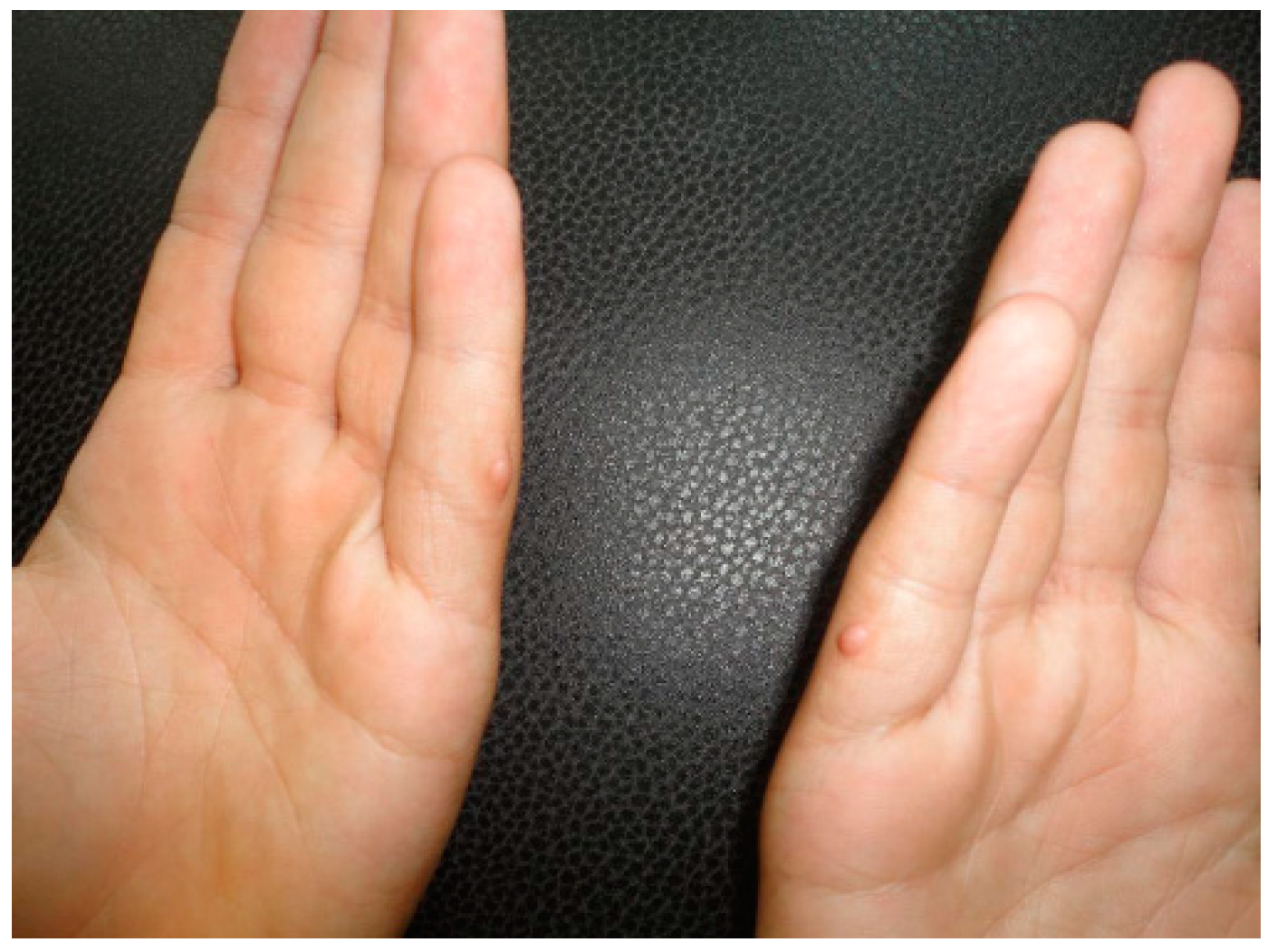
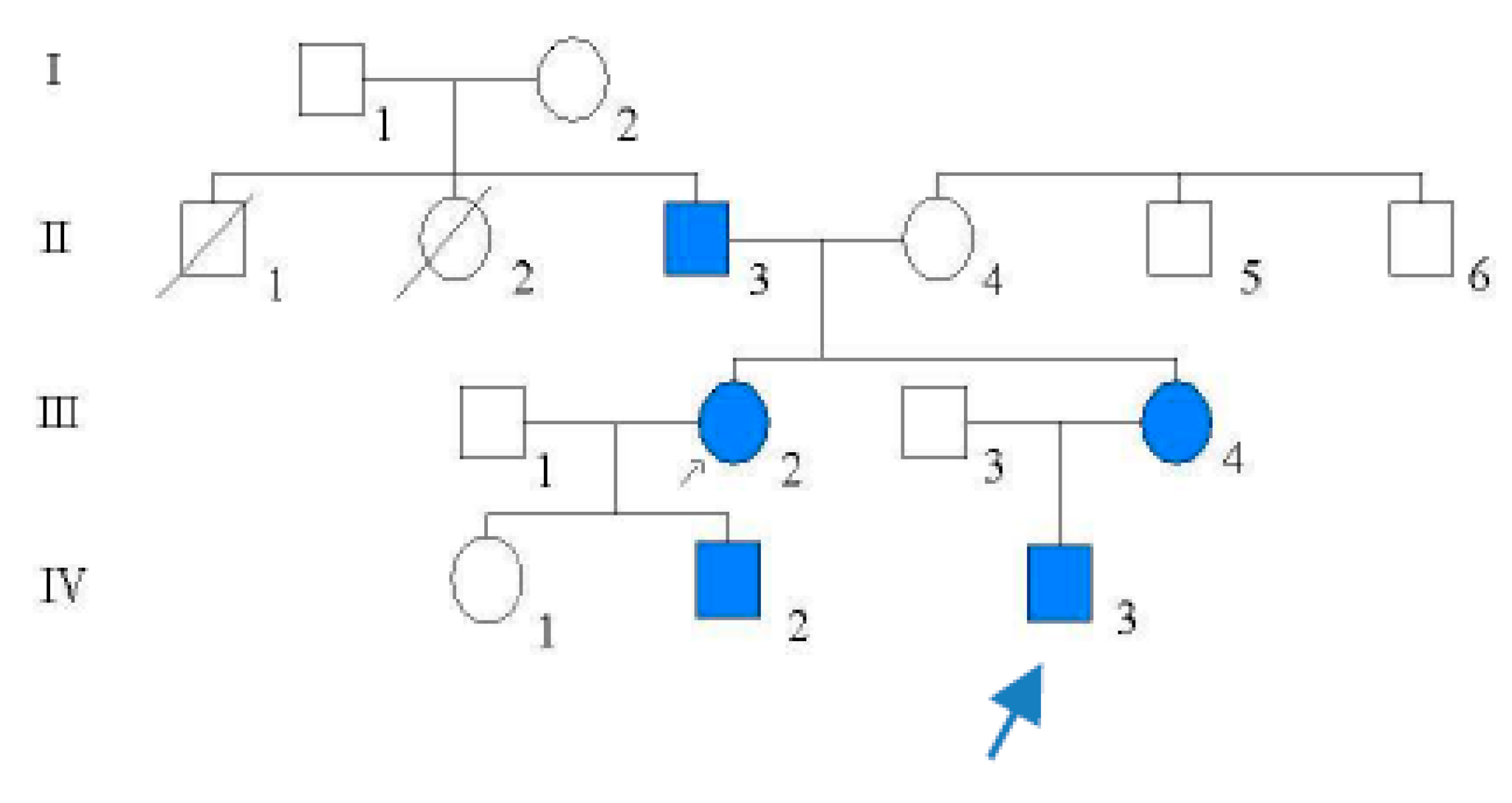
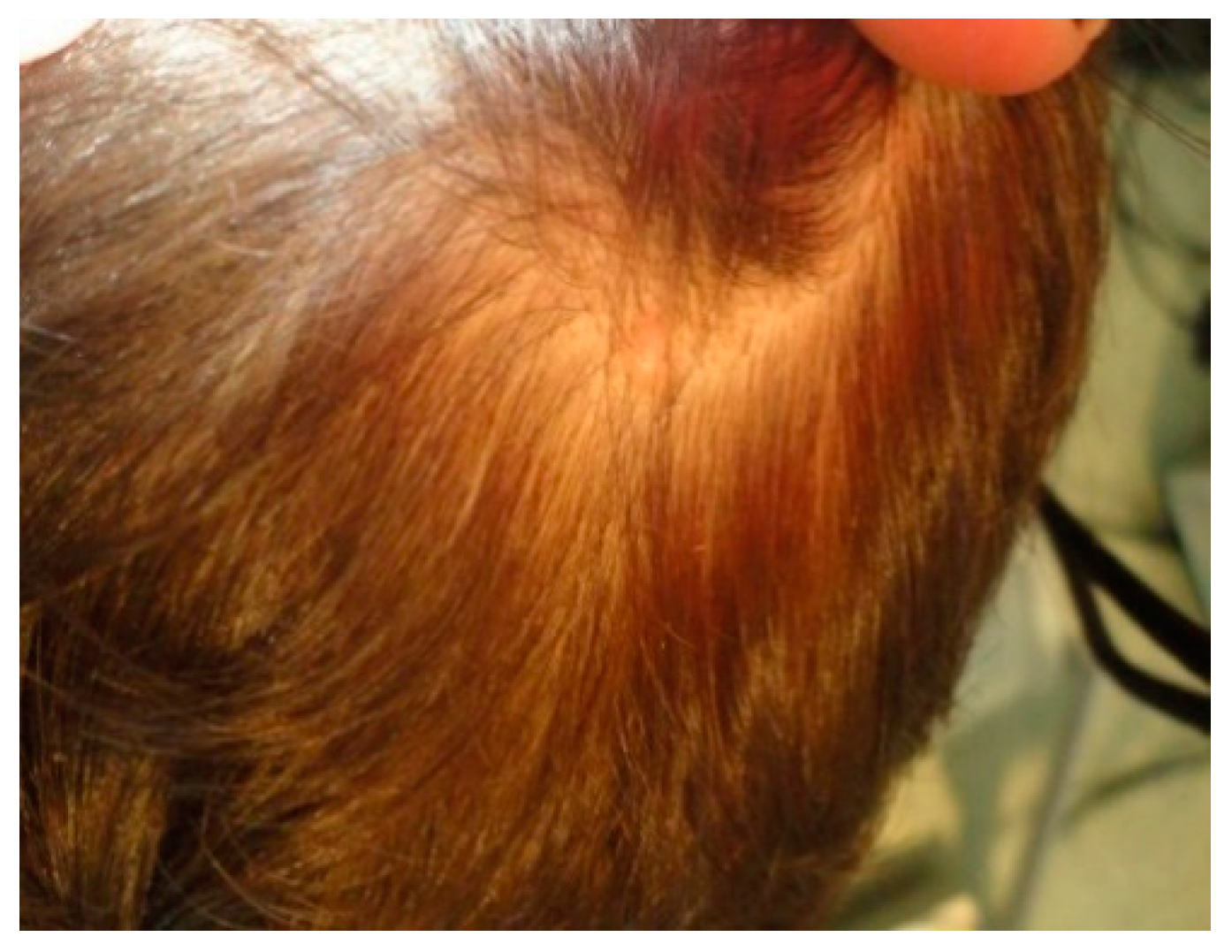
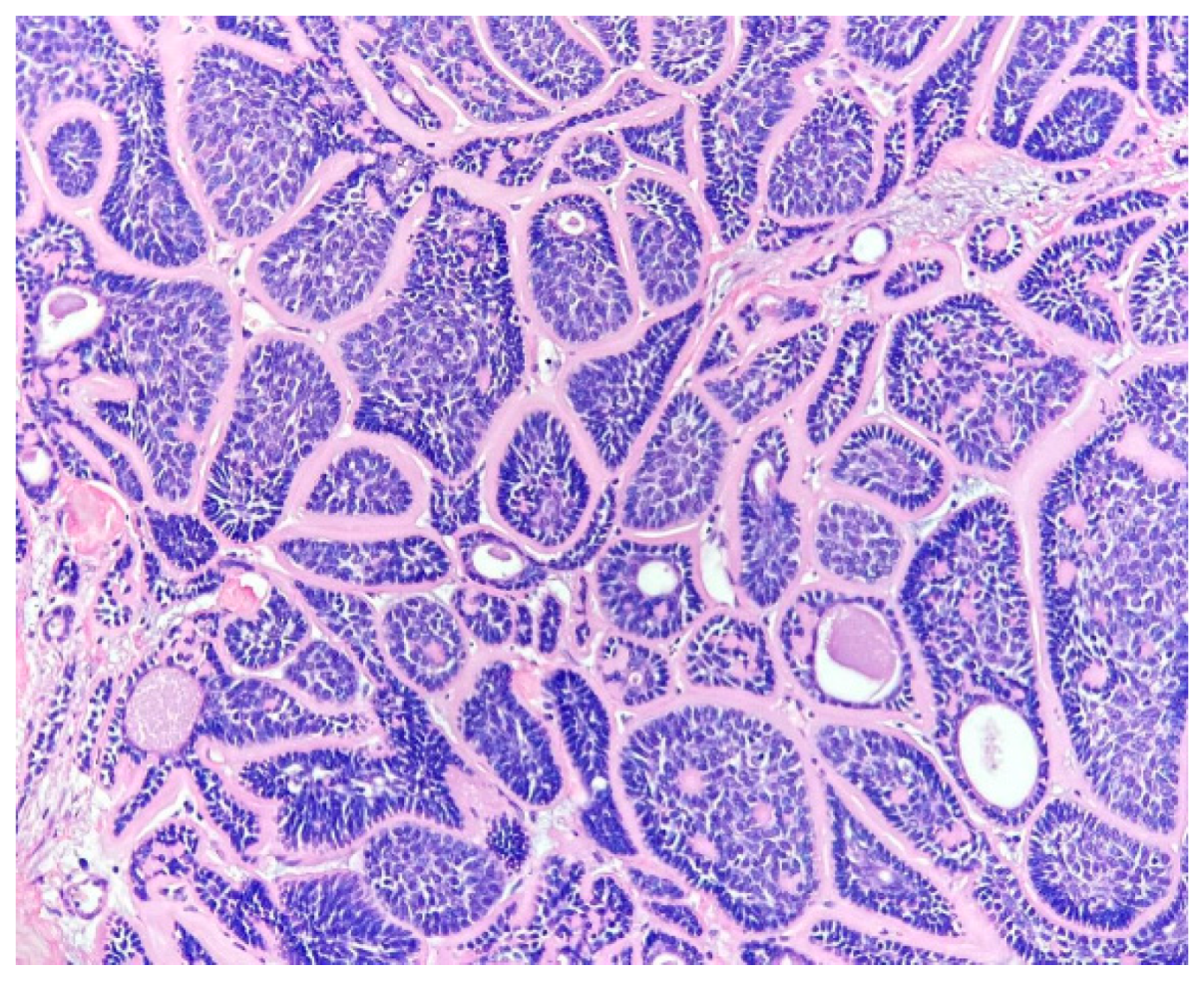
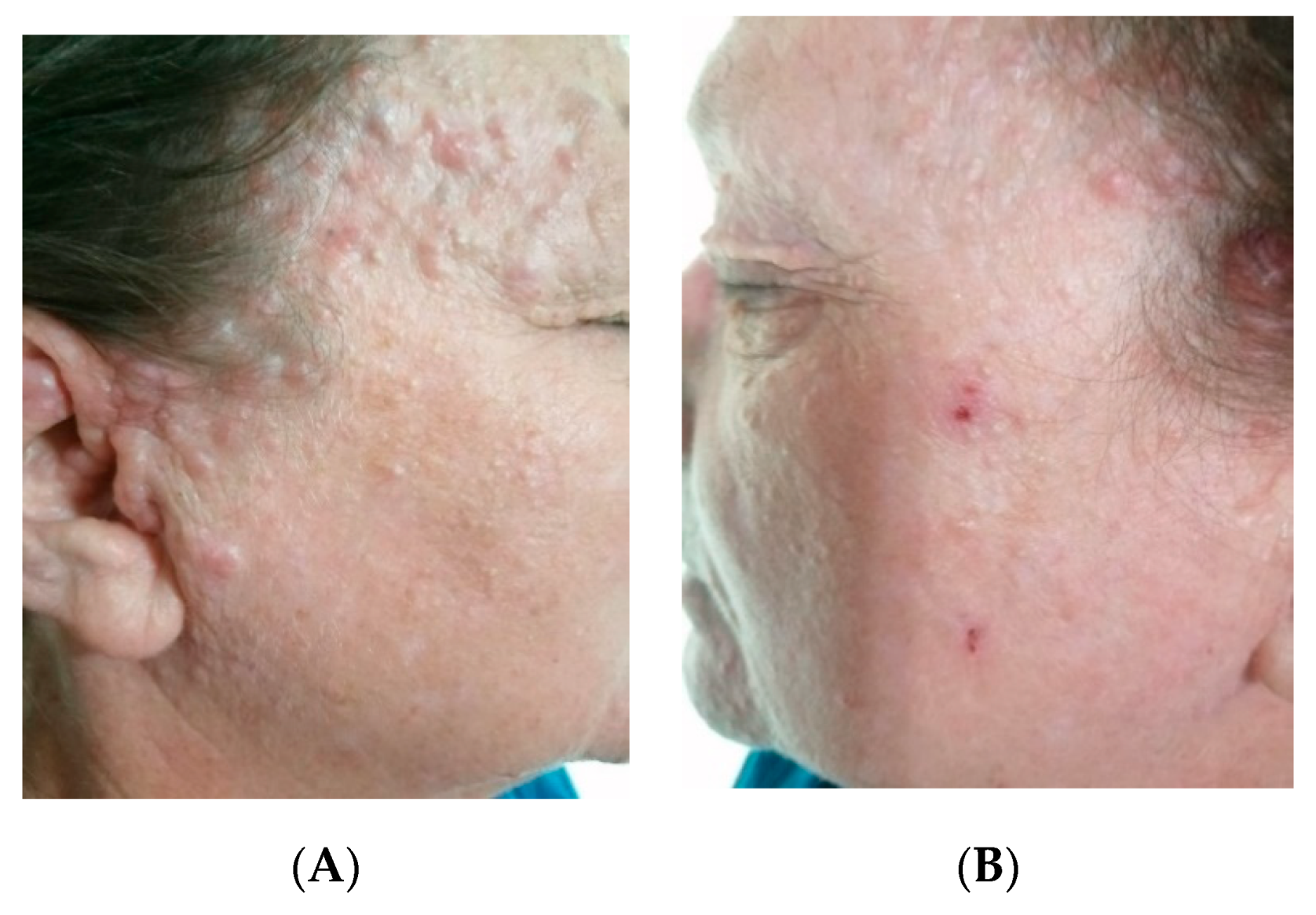
2. Case Presentation Section
3. Discussion
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Saggar, S.; Chernoff, K.A.; Lodha, S.; Horev, L.; Kohl, S.; Honjo, R.S.; Brandt, H.R.C.; Hartmann, K.; Celebi, J.T. CYLD mutations in familial skin appendage tumours. J. Med. Genet. 2008, 45, 298. [Google Scholar] [CrossRef]
- Bowen, S.; Gill, M.; Lee, D.A.; Fisher, G.; Geronemus, R.G.; Vazquez, M.E.; Celebi, J.T. Mutations in the CYLD gene in Brooke-Spiegler syndrome, familial cylindromatosis, and multiple familial trichoepithelioma: Lack of genotype-phenotype correlation. J. Investig. Dermatol. 2005, 124, 919. [Google Scholar] [CrossRef]
- Young, A.L.; Kellermayer, R.; Szigeti, R.; Teszas, A.; Azmi, S.; Celebi, J.T. CYLD mutations underlie Brooke-Spiegler, familial cylindromatosis, and multiple familial trichoepithelioma syndromes. Clin. Genet. 2006, 70, 246. [Google Scholar] [CrossRef] [PubMed]
- van den Ouweland, A.M.; Elfferich, P.; Lamping, R.; van de Graaf, R.; van Veghel-Plandsoen, M.M.; Franken, S.M.; Houweling, A.C. Identification of a large rearrangement in CYLD as a cause of familial cylindromatosis. Fam. Cancer 2011, 10, 127. [Google Scholar] [CrossRef] [PubMed]
- Puig, L.; Nadal, C.; Fernández-Figueras, M.T.; Alegre, M.; de Moragas, J.M. Brooke-Spiegler syndrome variant: Segregation of tumor types with mixed differentiation in two generations. Am. J. Dermatopathol. 1998, 20, 56–60. [Google Scholar] [CrossRef] [PubMed]
- Tantcheva-Poór, I.; Vanecek, T.; Lurati, M.C.; Rychly, B.; Kempf, W.; Michal, M.; Kazakov, D.V. Report of Three Novel Germline CYLD Mutations in Unrelated Patients with Brooke-Spiegler Syndrome, Including Classic Phenotype, Multiple Familial Trichoepitheliomas and Malignant Transformation. Dermatology 2016, 232, 30. [Google Scholar] [CrossRef] [PubMed]
- Grossmann, P.; Vanecek, T.; Steiner, P.; Kacerovska, D.; Spagnolo, D.V.; Cribier, B.; Rose, C.; Vazmitel, M.; Carlson, J.A.; Emberger, M.; et al. Novel and recurrent germline and somatic mutations in a cohort of 67 patients from 48 families with Brooke-Spiegler syndrome including the phenotypic variant of multiple familial trichoepitheliomas and correlation with the histopathologic findings in 379 biopsy specimens. Am. J. Dermatopathol. 2013, 35, 34–44. [Google Scholar]
- Sima, R.; Vanecek, T.; Kacerovska, D.; Trubac, P.; Cribier, B.; Rutten, A.; Vazmitel, M.; Spagnolo, D.V.; Litvik, R.; Vantuchova, Y.; et al. Brooke-Spiegler syndrome: Report of 10 patients from 8 families with novel germline mutations: Evidence of diverse somatic mutations in the same patient regardless of tumor type. Diagn. Mol. Pathol. 2010, 19, 83–91. [Google Scholar] [CrossRef]
- Kazakov, V.D. Brooke-Spiegler Syndrome and Phenotypic Variants: An Update. Head Neck Pathol. 2016, 10, 125–130. [Google Scholar] [CrossRef]
- Rathi, M.; Awasthi, S.; Budania, S.K.; Ahmad, F.; Dutta, S.; Kumar, A. Brooke-spiegler syndrome: A rare entity. Case Rep. Pathol. 2014, 2014, 231895. [Google Scholar] [CrossRef]
- Saunders, H.; Tucker, P.; Saurine, T.; Watkins, F. Pedigree of multiple benign adnexal tumours of Brooke–Spiegler type. Australas. J. Dermatol. 2003, 44, 144–148. [Google Scholar] [CrossRef] [PubMed]
- Hoang, L.; Black, M.M.; Robson, A. case of Brooke-Spiegler Syndrome. Australas. J. Dermatol. 2004, 45, 220–222. [Google Scholar]
- Ponti, G.; Pellacani, G.; Seidenari, S.; Pollio, A.; Muscatello, U.; Tomasi, A. Cancer-associated genodermatoses: Skin neoplasms as clues to hereditary tumor syndromes. Crit. Rev. Oncol. Hematol. 2013, 85, 239–256. [Google Scholar] [CrossRef]
- Weyers, W.; Nilles, M.; Eckert, F.; Schill, W.B. Spiradenomas in Brooke–Spiegler syndrome. Am. J. Dermatopathol. 1993, 15, 156–161. [Google Scholar] [CrossRef]
- Sellheyer, K. Spiradenoma and cylindroma originate from the hair follicle bulge and not from the eccrine sweat gland: An immunohistochemical study with CD200 and other stem cell markers. J. Cutan. Pathol. 2015, 42, 90–101. [Google Scholar] [CrossRef]
- Evans, C.D. Turban tumour. Br. J. Dermatol. 1954, 66, 434–443. [Google Scholar] [CrossRef]
- Kazakov, D.V.; Zelger, B.; Rütten, A.; Vazmitel, M.; Spagnolo, D.V.; Kacerovska, D.; Vanecek, T.; Grossmann, P.; Sima, R.; Grayson, W.; et al. Morphologic diversity of malignant neoplasms arising in preexisting spiradenoma, cylindroma, and spiradenocylindroma based on the study of 24 cases, sporadic or occurring in the setting of Brooke-Spiegler syndrome. Am. J. Surg. Pathol. 2009, 33, 705. [Google Scholar] [CrossRef]
- Weedon, D. Tumors of cutaneous appendages. In Weedon’s Skin Pathology, 3rd ed.; Churchill Livingstone Elsevier: London, UK, 2010; pp. 785–786. [Google Scholar]
- Calonje, J.E.; Brenn, T.; Lazar, A.; Billings, S. Mckee’s Pathology of the Skin, 5th ed.; Elsevier: Amsterdam, The Netherlands, 2019; pp. 1570–1573, 1657–1665. [Google Scholar]
- Kersting, D.W.; Helwig, E.B. Eccrine spiradenoma. AMA Arch. Dermatol. 1956, 73, 199–227. [Google Scholar] [CrossRef]
- Kanwaljeet, S.; Chatterjee, T. Eccrine spiradenoma: A rare adnexal tumor. Indian J. Cancer 2017, 54, 695–696. [Google Scholar] [CrossRef]
- Goette, D.K.; McConnell, M.A.; Fowler, V.R. Cylindroma and eccrinespiradenoma coexistent in the same lesion. Arch. Dermatol. 1982, 118, 723–724. [Google Scholar] [CrossRef]
- Poniecka, A.W.; Alexis, J.B. An immunohistochemical study of basal cell carcinoma and trichoepithelioma. Am. J. Dermatopathol. 1999, 21, 332–336. [Google Scholar] [CrossRef] [PubMed]
- Carsuzaa, F.; Carloz, E.; Lebeuf, M.; Grob, J.J.; Arnoux, D. Trichoépithéliomes multiples, cylindromes, grains de milium, dégénérescence carcinomateuse. Ann. Dermatol. Venereol. 1992, 119, 746–748. [Google Scholar]
- Rajan, N.; Trainer, A.H.; Burn, J.; Langtry, J.A.A. Familial Cylindromatosis and Brooke-Spiegler Syndrome: A Review of Current Therapeutic Approaches and the Surgical Challenges Posed by Two Affected Families. Dermatol. Surg. 2009, 5, 845–852. [Google Scholar] [CrossRef] [PubMed]
- Tarstedt, M.; Molin, L. Nd:YAG laser for effective treatment of multiple cylindroma of the scalp. J. Cosmet. Laser Ther. 2004, 6, 41–43. [Google Scholar] [CrossRef] [PubMed]
- Lo, J.S.; Snow, S.N.; Mohs, F.E. Cylindroma treated by Mohs micrographic surgery. J. Dermatol. Surg. Oncol. 1991, 17, 871–874. [Google Scholar] [CrossRef]
- Crain, R.C.; Helwig, E.B. Dermal cylindroma (dermal eccrine cylindroma). Am. J. Clin. Pathol. 1961, 35, 504–515. [Google Scholar] [CrossRef]
- Irwin, L.R.; Bainbridge, L.C.; Reid, C.A.; Piggot, T.A.; Brown, H.G. Dermal eccrine cylindroma (turban tumour). Br. J. Plast. Surg. 1990, 43, 702–705. [Google Scholar] [CrossRef]




© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leventer, M.; Coltoiu, C.; Zota, A.; Tebeica, T.; Lisievici, C.; Martinescu, A. Observations on Four Cases of Brooke–Spiegler Syndrome. Reports 2020, 3, 28. https://doi.org/10.3390/reports3040028
Leventer M, Coltoiu C, Zota A, Tebeica T, Lisievici C, Martinescu A. Observations on Four Cases of Brooke–Spiegler Syndrome. Reports. 2020; 3(4):28. https://doi.org/10.3390/reports3040028
Chicago/Turabian StyleLeventer, Mihaela, Casandra Coltoiu, Alexandra Zota, Tiberiu Tebeica, Carmen Lisievici, and Alina Martinescu. 2020. "Observations on Four Cases of Brooke–Spiegler Syndrome" Reports 3, no. 4: 28. https://doi.org/10.3390/reports3040028
APA StyleLeventer, M., Coltoiu, C., Zota, A., Tebeica, T., Lisievici, C., & Martinescu, A. (2020). Observations on Four Cases of Brooke–Spiegler Syndrome. Reports, 3(4), 28. https://doi.org/10.3390/reports3040028





