An Unusual Case of Vomiting Caused by Myeloid Sarcoma
Abstract
:1. Introduction
- AML with recurrent genetic abnormalities
- AML with myelodysplasia-related features
- Therapy-related AML and MDS
- AML, not otherwise specified
- Myeloid sarcoma
- Myeloid proliferations related to Down syndrome
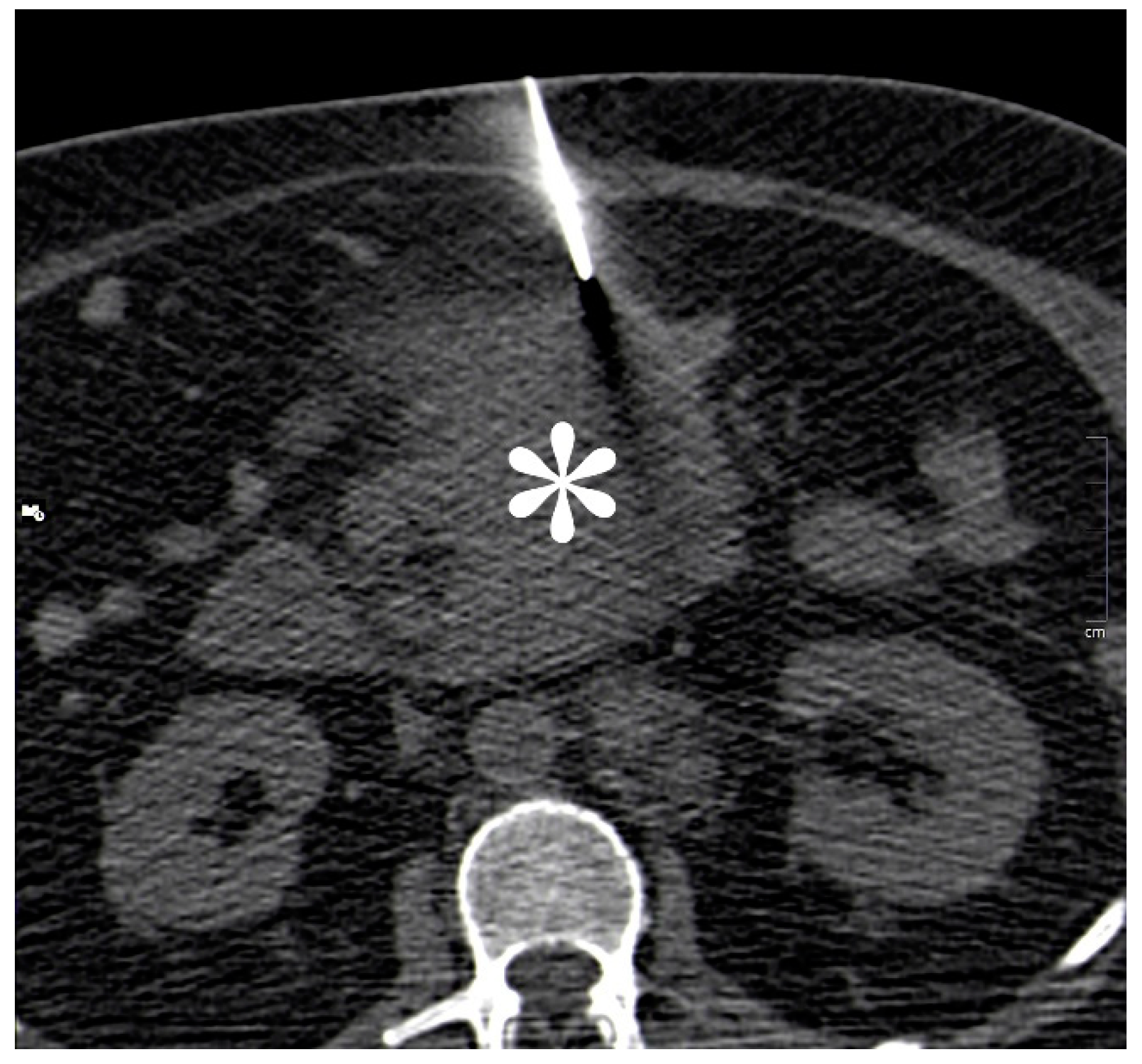
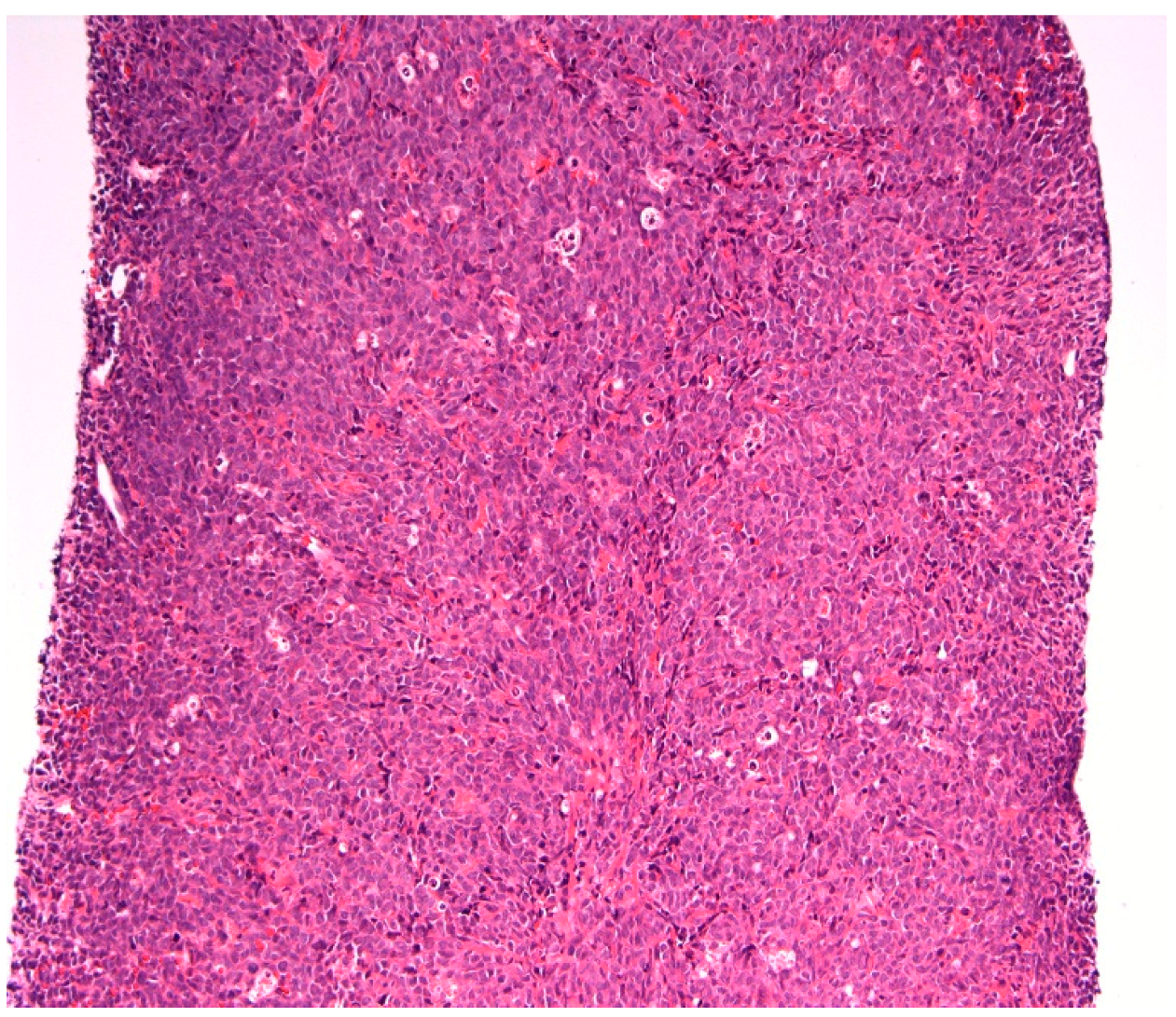
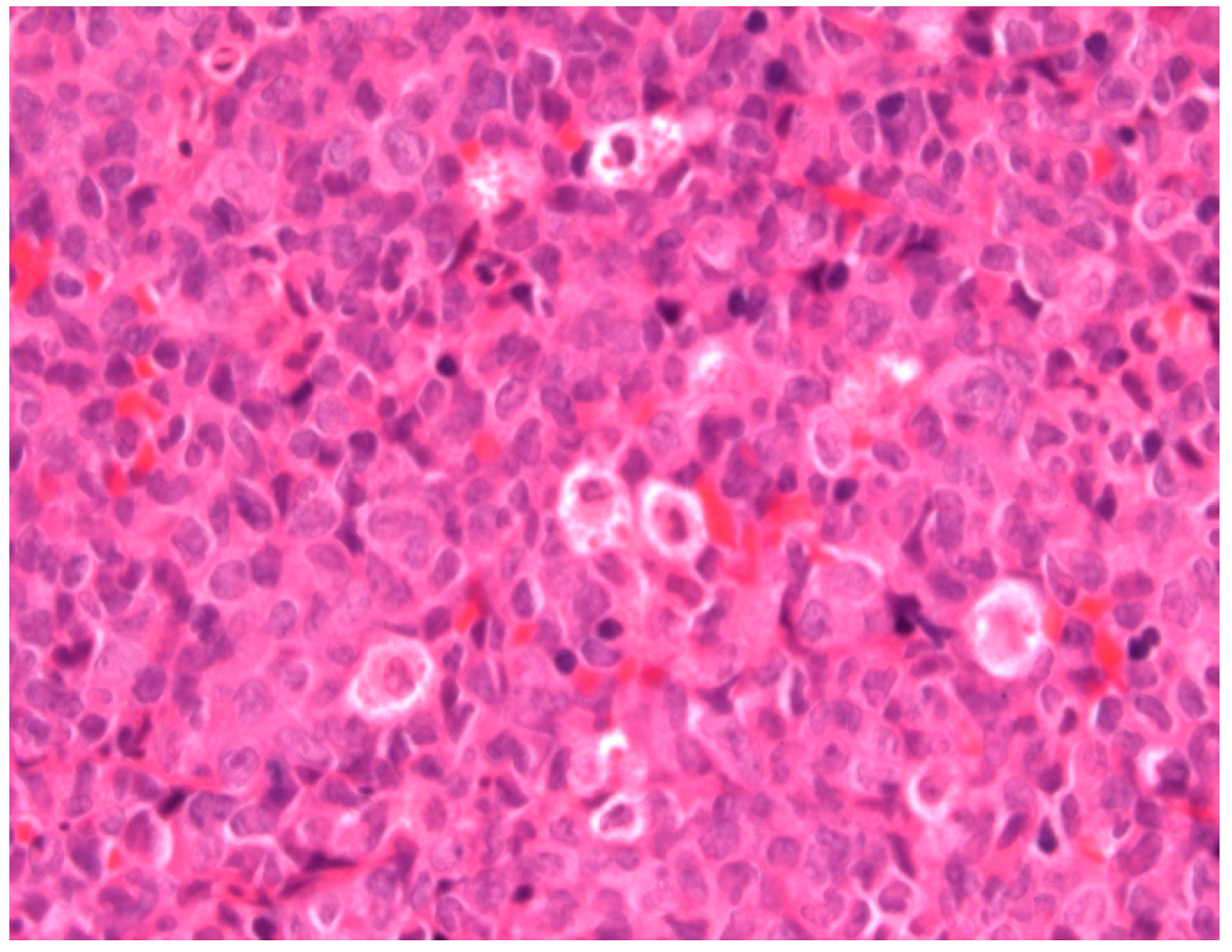
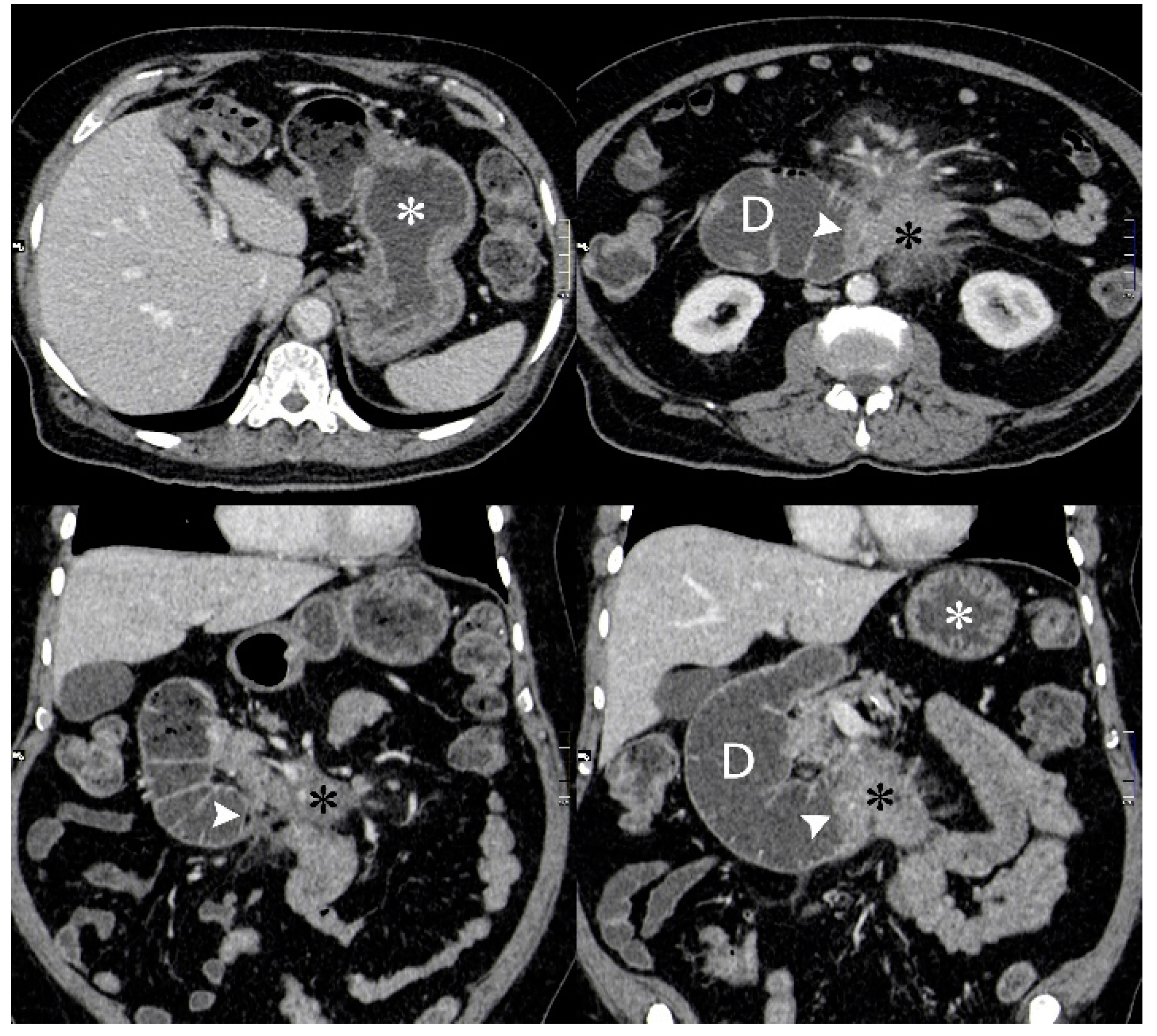
2. Case Report
3. Discussion
4. Conclusions
Funding
Acknowledgments
Conflicts of Interest
References
- Byrd, J.C.; Edenfield, W.J.; Shields, D.J.; Dawson, N.A. Extramedullary myeloid cell tumors in acute nonlymphocytic leukemia: A clinical review. J. Clin. Oncol. 1995, 13, 1800–1816. [Google Scholar] [CrossRef] [PubMed]
- Vardiman, J.W.; Thiele, J.; Arber, D.A.; Brunning, R.D.; Borowitz, M.J.; Porwit, A.; Harris, N.L.; Le Beau, M.M.; Hellström-Lindberg, E.; Tefferi, A.; et al. The 2008 revision of the World Health Organization (WHO) classification of myeloid neoplasms and acute leukemia: Rationale and important changes. Blood 2009, 114, 937–951. [Google Scholar] [CrossRef] [PubMed]
- Benjazia, E.; Khalifa, M.; Benabdelkader, A.; Laatiri, A.; Braham, A.; Letaief, A.; Bahri, F. Granulocytic sarcoma of the rectum: Report of one case that presented with rectal bleeding. World J. Gastrointest. Pathophysiol. 2010, 1, 144–146. [Google Scholar] [CrossRef] [PubMed]
- Swedlow, S.H.; Campo, E.; Harris, N.L.; Jaffe, E.S.; Pileri, S.A.; Stein, H.; Thiele, J.; Vardiman, J.W. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues, 4th ed.; IARC Press: Lyon, France, 2008. [Google Scholar]
- Choi, E.K.; Ha, H.K.; Park, S.H. Granulocytic Sarcoma of Bowel: CT Findings. Radiology 2007, 243, 3. [Google Scholar] [CrossRef] [PubMed]
- Girelli, C.M.; Carsenzuola, V.; Latargia, M.; Aguzzi, A.; Serio, G. Small-bowel myeloid sarcoma: Report of a case with atypical presentation. Int. J. Surg. Case Rep. 2014, 5, 613–616. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miliauskas, J.R.; Crowley, K.S. Granulocytic sarcoma (chloroma) of the small intestine with associated megakaryocytes. Pathology 1985, 17, 661–662. [Google Scholar] [CrossRef]
- John, S.; Ahmad, H.A.; Dunna, T.; Kern, W.; Holter, J.; Cherry, M. Unusual presentation of bladder myeloid sarcoma causing acute renal failure: Case report and review of the literature. Clin. Adv. Haematol. Oncol. 2013, 11, 388–392. [Google Scholar]
- Pileri, S.A.; Ascani, S.; Cox, M.C.; Campidelli, C.; Bacci, F.; Piccioli, M.; Piccaluga, P.P.; Agostinelli, C.; Asioli, S.; Novero, D.; et al. Myeloid sarcoma: Clinic-pathologic, phenotypic and cytogenetic analysis of 92 adult patients. Leukemia 2007, 21, 340–350. [Google Scholar] [CrossRef] [PubMed]
- Bakst, R.L.; Tallman, M.S.; Douer, D.; Yahalom, J. How I treat extramedullary acute myeloid leukemia. Blood 2011, 118, 3785–3793. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Menon, S.; Trudgill, N. How commonly is upper gastrointestinal cancer missed at endoscopy? A meta-analysis. Endosc. Int. Open 2014, 2, E46–E50. [Google Scholar] [CrossRef] [PubMed]



| Full Blood Count | Patient’s Results | Normal Range |
|---|---|---|
| Haemoglobin (Hb) | 146 g/L | 130–180 g/L |
| White Cell Count (WCC) | 92.8 × 109/L | 4.0 × 109/L–11.0 × 109/L |
| Platelets (Plts) | 60 × 109/L | 150× 109/L–450 × 109/L |
| Mean Corpuscular Volume (MCV) | 84/2 FL | 76.0–100.0 FL |
| Neutrophils | 21.6 × 109/L | 2.0 × 109/L–7.5 × 109/L |
| Lymphocytes | 10.6 × 109/L | 1.5 × 109/L–4.0 × 109/L |
| Monocytes | 25.3 × 109/L | 0.2 × 109/L–0.8 × 109/L |
| Eosinophils | 0.3 × 109/L | 0.0 × 109/L–0.4 × 109/L |
| Basophils | 4.0 × 109/L | 0.0 × 109/L–0.4 × 109/L |
| Renal Profile | ||
| Sodium | 136 mmol/L | 133–146 moml/L |
| Potassium | 3.3 mmol/L | 3.5–5.3 mmol/L |
| Urea | 12.7 mmol/L | 2.5–7.8 mmol/L |
| Creatinine | 111 mmol/L | 58–110 mmol/L |
| Liver Profile | ||
| Total Bilirubin | 10 umol/L | 0–21 umol/L |
| ALT | 21 IU/L | 3–53 IU/L |
| ALP | 109 IU/L | 30–130 IU/L |
| Albumin | 37 g/L | 35–50 g/L |
| Bone Profile | ||
| Calcium | 2.30 mmol/L | 2.20–2.60 mmol/L |
| Adjusted Calcium | 2.38 mmol/L | 2.20–2.60 mmol/L |
| Total Protein | 64 g/L | 60–80 g/L |
| Globulin | 27 g/L | 18–36 g/L |
| CRP | 53 mg/L | 0–10 mg/L |
| Lactate Dehydrogenase | 6104 IU/L | 313–619 IU/L |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Goodoory, V.C.; Triantafyllopoulou, D.; Gkikas, I.; Alani, F.; Bin, A.A.; Mellor, S.; Adiyodi, J.; Sahasrabudhe, N.; Saxton, M.; Cowburn, H. An Unusual Case of Vomiting Caused by Myeloid Sarcoma. Reports 2019, 2, 2. https://doi.org/10.3390/reports2010002
Goodoory VC, Triantafyllopoulou D, Gkikas I, Alani F, Bin AA, Mellor S, Adiyodi J, Sahasrabudhe N, Saxton M, Cowburn H. An Unusual Case of Vomiting Caused by Myeloid Sarcoma. Reports. 2019; 2(1):2. https://doi.org/10.3390/reports2010002
Chicago/Turabian StyleGoodoory, Vivek Chand, Diana Triantafyllopoulou, Ioannis Gkikas, Fouad Alani, Ayub Ali Bin, Stuart Mellor, Jagdish Adiyodi, Neil Sahasrabudhe, Matthew Saxton, and Hazel Cowburn. 2019. "An Unusual Case of Vomiting Caused by Myeloid Sarcoma" Reports 2, no. 1: 2. https://doi.org/10.3390/reports2010002
APA StyleGoodoory, V. C., Triantafyllopoulou, D., Gkikas, I., Alani, F., Bin, A. A., Mellor, S., Adiyodi, J., Sahasrabudhe, N., Saxton, M., & Cowburn, H. (2019). An Unusual Case of Vomiting Caused by Myeloid Sarcoma. Reports, 2(1), 2. https://doi.org/10.3390/reports2010002





