Abstract
We present the case of an eighty-two-year-old man who presented with testicular pain, diarrhoea, fresh rectal bleeding, and weight loss. A clear history was not obtained because of presumed chronic confusion secondary to age related vascular dementia. He was subsequently diagnosed with Fournier’s gangrene and a retrospective obtainment of his collateral history revealed a completely normal pre-morbid cognitive level of function. Thus, his confusion was secondary to an atypical cause of sepsis and he was managed with surgical debridement. We highlight the value of urgent computed tomography (CT) scanning as well as the use of screening tools for assessing cognitive function, particularly in surgical specialties, as well as the importance of obtaining a collateral history and discussing means for better collaborative efforts amongst surgeons and physicians in managing the “confused patient”.
1. Introduction
Fournier’s gangrene is an infection normally characterised by the mixture of aerobic and anaerobic microorganisms resulting in necrosis of fascia layers around the perineal skin and genital areas [1]. It is a progressive process and can be fatal if not treated promptly [2]. Early clinical identification and surgical intervention are essential to managing these patients. Fournier’s gangrene has a very high mortality rate, up to 45% in some case series [3,4].
Perforated rectal cancer is a known cause of Fournier’s gangrene, however, its incidence is unknown [5]. We present a case of a patient who had immediate symptoms of Fournier’s gangrene with a history suggestive of rectal cancer symptoms. We discuss how his treatment was nearly delayed because his confusion was initially wrongly attributed to a dementia-process, and the value of early computer tomography (CT) scanning to both aid the diagnosis as well as for preoperative planning.
2. Case Presentation Section
An eighty-two-year-old man presented to the surgical assessment unit with a ten-day history of scrotal pain. He also reported a history of change in bowel habit to diarrhoea, as well as haematochezia, urinary incontinence during defaecation, and one stone weight loss over the preceding four-months. His initial surgical review noted the patient to be a poor historian and confused. His confusion was thought to be chronic and age-related, and because of this, components of the history were dismissed.
Clinical examination revealed evidence of sepsis with a pyrexia (38 °C), tachycardia (122 bpm), and tachypnoea (22 bpm), but he remained normotensive (135/62 mmHg). His abdomen was soft and non-tender, but he had a large scrotal swelling with skin changes on the left side and the testicle was noted to feel firm and craggy. Rectal examination also revealed a firm mass. Cognition testing was not completed.
Blood tests revealed a white blood cell count of: 21.1 × 109/L (3.5–9.5 × 109/L), Neutrophils: 18.3 (1.7–6.5 × 109/L), and C-reactive protein: 278 mg/L (0–5 mg/L). He was started on Piperacillin/Tazobactam (Tazocin) and Clindamycin pending further review.
A later senior review allowed for a collateral history to be obtained from the patient’s son who confirmed that the patient was indeed an excellent communicator and any confused behaviour noted during the admission was grossly atypical behaviour for him.
An urgent computed tomography scan was requested, revealing a possible rectal cancer with bilateral hydrocoeles (Figure 1). Urgent debridement of the scrotal tissue for Fournier’s gangrene was undertaken. Rectal biopsies revealed a villous adenoma with a high-grade dysplasia. The scrotal biopsies showed surface ulceration of the skin with a pronounced acute inflammatory infiltrate with abscess formation and infarction in the underlying dermis which extended to involve the subcutaneous tissues and adherent underlying testicular tissue and tracts along the epididymis in keeping with Fournier’s gangrene. Causative organisms were Staphylococcus aureus and Escherichia coli.
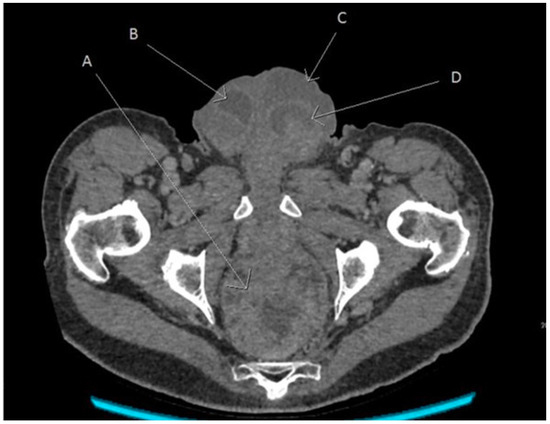
Figure 1.
Angled axial reconstruction computed tomography image of abdomen and pelvis showing the rectal tumour, scrotal collection, and bilateral hydrocoeles. A—Rectal tumour, B—Right hydrocele, C—Left scrotal collection, and D—Left hydrocele.
Subsequently, a defunctioning colostomy was performed with further debridement of his Fournier’s gangrene and mesh grafting.
His cognitive function returned to baseline following surgical management of his sepsis. The multi-disciplinary review suggested a course of palliative chemotherapy which he received and from which he is currently recovering. Consent was gained directly from the patient. As per BMJ guidance no additional ethical approval was required.
3. Discussion
This case represents an interesting presentation of the relatively rare condition of Fournier’s gangrene, the treatment for which is urgent surgical debridement.
Attention to the history was essential, not only to the complaint of scrotal pain, but also the patient’s preceding symptoms of changes in bowel habits and rectal bleeding supported a diagnosis of rectal malignancy. The combination of symptoms was thereby suggestive of local invasion resulting in Fournier’s gangrene, as demonstrated in other reported cases [6]. Cross-sectional imaging is thus imperative in such scenarios to exclude other causes of local sepsis, such as pelvic abscess, and to allow for preoperative assessment whilst not delaying surgical debridement. The CT scan allowed for better decision making as to whether to defunction the patient during initial surgical debridement.
This case also demonstrates an important point to be learnt from in that surgeons can often focus on the pathology without paying as much respect to the history, particularly the collateral history. Thus, as shown here, the patient was initially labelled as being confused without investigating the timings and mechanisms underlying this. Cognitive assessment, an essential tool in the clerking armamentarium, was not undertaken here, and had it been performed, would have triggered an earlier investigation and management of the patients’ confusion [1].
There is national guidance with respect to screening for delirium but there needs to be cross-specialty engagement for it to be truly effective, as when undertaken, it can yield highly successful outcomes [7,8]. The senior review included a collateral history and indicated that the patient’s presentation of confusion was not due to dementia, but due to sepsis and that this had delayed management slightly.
A Pubmed search for “collateral history” and “General surgery” and “Elderly”/”Older”/”Ageing” received no results. The importance of this in the management of this patient was imperative and yet there is very little published on the topic.
Whilst older patients are associated with poorer post-operative morbidity and mortality, these risks are often directly linked to both comorbidity as well as timing of intervention [9]. Thus, early attention to the history, including a careful cognitive assessment, and collateral account can save time later in the patient journey resulting in better overall outcomes.
We believe this case highlights the need for urgent CT scanning if available as well as a more holistic surgical approach aimed at achieving such processes, in addition to a more coordinated surgical-physician approach to managing confused older patients.
4. Conclusions
A Fournier’s gangrene requires urgent debridement. Symptoms of rectal cancer should raise suspicious of perforation leading to Fournier’s gangrene. Cross-sectional imaging can aid surgical planning in a case like this to assist deciding whether the patient should be defunctioned immediately or during the ensuing debridement operations.
Confusion in an elderly patient should be screened as this may be sepsis induced. Even in an apparently confused patient, there may be sufficient information that can be extracted from the history to achieve a diagnosis or working list of differentials. It is imperative to also obtain a collateral history in such situations to support initial clinical suspicions. Perhaps this point is best made by the famous quote from the nineteenth century physician, Sir William Osler, who said “Listen to your patient, for he is telling you the diagnosis.”
Author Contributions
J.G.: Developing, proofing the manuscript and editing the images. H.N.H.: Developing and proofing the manuscript. P.S.: Proofing the manuscript and concept development.
Funding
This research received no external funding.
Acknowledgments
The authors would like to thank James Hampton Consultant Radiologist for annotating and sourcing the images.
Conflicts of Interest
The authors declare no conflict of interest.
References
- George, J.; Raja, A.; Hei, C.; Li, D.; Joshi, H. Fournier’s gangrene: Diagnosis and management aided by repeated clinical examination and ultrasound. BMJ Case Rep. 2017. [Google Scholar] [CrossRef] [PubMed]
- Smith, G.L.; Bunker, C.B.; Dinneen, M.D. Fournier’s gangrene. Br. J. Urol. 1998, 81, 347–355. [Google Scholar] [CrossRef] [PubMed]
- Oguz, A.; Gümüş, M.; Turkoglu, A.; Bozdağ, Z.; Ülger, B.V.; Agaçayak, E.; Böyük, A. Fournier’s Gangrene: A Summary of 10 Years of Clinical Experience. Int. Surg. 2015, 100, 934–941. [Google Scholar] [CrossRef] [PubMed]
- Hejase, M.J.; Simonin, J.E.; Bihrle, R.; Coogan, C.L. Genital Fournier’s gangrene: Experience with 38 patients. Urology 1996, 47, 734–739. [Google Scholar] [CrossRef]
- Bruketa, T.; Majerovic, M.; Augustin, G. Rectal cancer and Fournier’s gangrene—Current knowledge and therapeutic options. World J. Gastroenterol. 2015, 21, 9002–9020. [Google Scholar] [CrossRef] [PubMed]
- Yoshino, Y.; Funahashi, K.; Okada, R.; Miura, Y.; Suzuki, T.; Koda, T.; Yoshida, K.; Koike, J.; Shiokawa, H.; Ushigome, M.; et al. Severe Fournier’s gangrene in a patient with rectal cancer: Case report and literature review. World J. Surg. Oncol. 2016, 14, 234. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Excellence. Delirium: Prevention, Diagnosis and Management; Guidance and Guidelines; NICE: London, UK, 2010. [Google Scholar]
- McNaughton-Garratt, H.; Safran, A.; Ahsan, M. Audit of the implementation of a dementia CQUIN diagnostic screening tool: A district general hospital experience. Age Ageing 2014, 43, i9. [Google Scholar] [CrossRef]
- Hamel, M.B.; Henderson, W.G.; Khuri, S.F.; Daley, J. Surgical Outcomes for Patients Aged 80 and Older: Morbidity and Mortality from Major Noncardiac Surgery. J. Am. Geriatr. Soc. 2005, 53, 424–429. [Google Scholar] [CrossRef] [PubMed]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).