Abstract
Motion sickness is known under several names in different domains, such as seasickness, carsickness, cybersickness, and simulator sickness. As we will argue, these can all be considered manifestations of one common underlying mechanism. In recent years, it has received renewed interest, largely due to the advent of automated vehicles and developments in virtual reality, in particular using head-mounted displays. Currently, the most widely accepted standard to predict motion sickness is ISO 2631-1 (1997), which is based on studies on seasickness and has limited applicability to these newer domains. Therefore, this paper argues for extending the ISO standard to cover all forms of motion sickness, to incorporate factors affecting motion sickness, and to consider various degrees of severity of motion sickness rather than just emesis. This requires a dedicated standard, separate from other effects of whole-body vibration as described in the current ISO 2631-1. To that end, we first provide a sketch of the historical origins of the ISO 2631-1 standard regarding motion sickness and discuss the evidence for a common mechanism underlying various forms of motion sickness. After discussing some methodological issues concerning the measurement of motion sickness, we outline the main knowledge gaps that require further research.
1. Introduction
Motion sickness is a syndrome of adverse effects caused by exposure to motion stimuli (inertial, visual, or in combination). Recently, research into motion sickness has received increased interest due to developments in automated driving and virtual reality, as well as augmented, mixed, and extended reality, but for the current purpose further summarized under the term VR. As such, it is imperative to achieve consensus among researchers on the methodology to be used in these studies and on models that describe or predict motion sickness for applications in various domains. The current ISO standard (ISO 2631-1, 1997 [1]) includes motion sickness among various effects of oscillatory motion on humans and is largely based on research concerning seasickness; therefore, it has a limited applicability to other forms of motion sickness. In this paper, we argue that this standard needs to be further extended and developed into a separate standard on motion sickness, including a consensus on how to measure and predict motion sickness in its various forms. We also outline the most important gaps in our current understanding of motion sickness that need to be addressed in order to establish this new standard. We start our paper by looking back at the origin of the current standard and by briefly discussing the mechanisms that are thought to cause motion sickness. This paper does not aim to explain motion sickness per se and for this the reader is referred to some of the excellent reviews already existing in the literature, e.g., [2,3,4,5]. The paper does not aim to be complete either. Although, for example, it does not deal with countermeasures, an extended standard will be of value in the design and validation thereof.
1.1. Origin and Historical Background of the ISO 2631-1 Standard
The ISO 2631-1 standard on motion sickness traces its roots back to World War II, in which seasickness was found to be a serious threat to soldier performance after ship-based transport of troops, which subsequently led to basic research programs to better understand and predict the phenomenon. A series of laboratory studies were performed by, for example [6,7,8,9,10,11,12,13,14,15,16]. Among the most cited sea trials are those by [17,18,19,20]. Studies like these resulted in the ISO 2631-1 [1] and the British Standard 6841 [21]. Given their origin, these standards were limited to vertical motion which was shown to be the dominant factor with respect to seasickness aboard relatively large ships. In these ships, the combination of tangential acceleration due to pitch and heave caused by swell typically shows relatively high power exactly in the frequency range that appeared to elicit most sickness [14].
1.2. Predictive Model of Seasickness
ISO 2631-1 includes a mathematical description of the percentage of people that are expected to reach emesis (i.e., vomit) during a certain interval of motion exposure, also referred to as the Motion Sickness Incidence (MSI). It is based on the so-called Motion Sickness Dose Value (MSDV), which is the integration over time of the frequency-weighted instantaneous vertical acceleration:
where aw is the frequency-weighted acceleration (in m/s2) and T the motion exposure duration (in seconds). MSDV is accordingly expressed in units of m/s3/2. According to the ISO prediction,
where Km = 1/3 for a mixed population of males and females. The standard also provides a weighting function that is used to calculate the frequency-weighted acceleration in order to arrive at the MSDV. It uses a similar approach to predict effects of whole-body vibration on health, perception, and comfort.
MSDVz = { ∫0T [aw(t)]2dt}½
MSI = Km⋅MSDVz
1.3. Limitations of the Current Standard
As already mentioned above, a major limitation of the ISO 2631-1 standard on motion sickness concerns its application to vertical (ship) motion only. However, horizontal car motion, for example, due to accelerating, braking, and cornering, generally does show more power in the frequency range of human sensitivity to sickness than vertical car accelerations do [22]. The latter typically show most power at frequencies above 1 Hz which, according to the ISO 2631-1 standard, are hardly provocative. Although carsickness has been an issue since the invention of the automobile, it started to receive increasing attention since the early 2000s with the introduction of vehicle automation, which is expected to increase the incidence of carsickness. The reason for this is the fact that vehicle automation renders all occupants into passengers, who, compared to drivers, are known to be more susceptible to carsickness [23,24,25,26]. In addition, vehicle automation enables passengers to engage in a wide variety of in-vehicle activities, such as reading or screen use, which are also known to increase the likelihood of carsickness [25,26] (see further below). Given that 60–70% of all passengers do suffer from carsickness at some moment [26,27], and that currently only about 30% of all car occupants are passengers, this will turn carsickness from a minority (approx. 60–70% × 30% ≈ 20% suffering currently) into a majority problem (60–70% × 100% suffering in automated vehicles) [28]. Hence, this poses the question of whether ISO 2631-1, being defined for vertical motion only, is a valid tool to also predict carsickness.
Moreover, ISO 2631-1 only considers emesis, with all other symptoms typically preceding that (see further below) not taken into account, even though these do contribute to the general appraisal of comfort [29]. Hence, this further raises questions as to the validity of ISO 2631-1 not only for predicting carsickness, but for all other forms of motion sickness as well.
A third major limitation concerns the effect of vision. At the time the ISO 2631-1 standard was formulated, the effect of vision, though known, was not incorporated in the standard. This may be partly explained by observations that people in whom the organs of balance are not functioning appear to be almost, if not completely, insensitive to motion sickness [30,31,32], while blind people do suffer [33]. However, the effect of vision in motion sickness became critical when simulators started to be used for training purposes in the 1960s [34,35,36], and even more so with the introduction of Virtual Reality (VR) and VR goggles, in particular from about 2000 onwards (e.g., [3,37,38]. Simulator sickness can have a severe impact, as illustrated by findings according to which dropout rates in training due to sickness of 50% are no exception (e.g., [39]), and have in some instances even been found to increase above 90% [40]. It goes without saying that ISO 2631-1 does not take into account simulator sickness, cybersickness, or even just visually induced motion sickness (VIMS) at all.
2. Underlying Mechanism of Motion Sickness
Although multiple theories have been suggested to explain motion sickness (e.g., [2,3,4,5], we here focus on the two most cited theories.
2.1. Theories
Although far from complete, scientific consensus is growing regarding the underlying mechanism of motion sickness. Motion sickness is generally assumed to be caused by a conflict between integrated sensory information about self-motion and a prediction or expectation thereof created by the brain based on previous experiences and on a copy of motor commands controlling the actual self-motion [41,42,43,44,45,46]. Although they are still in a developing phase, mathematical elaborations of this mechanism have already shown promising results in predicting several observations [47,48,49,50,51,52].
Another theory focuses on the role of postural instability explaining motion sickness [53,54]. Apart from the explicit statement that postural instability is a necessary and sufficient condition for getting sick, this theory otherwise seems to be largely compatible with the neural mismatch theory (see also [55]). Taken together, this suggests the possibility of understanding, describing, and predicting motion sickness not only based on inertial motion, but on visual motion as well, and draws together all forms of motion sickness as shown in Figure 1.
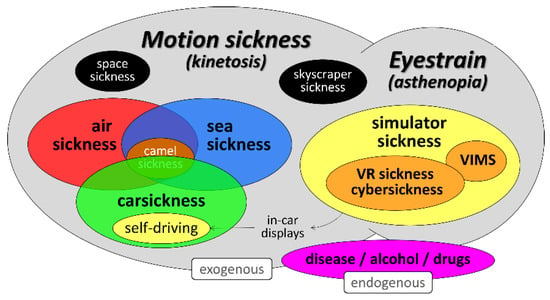
Figure 1.
Motion sickness taxonomy reflecting the conditions in which motion sickness and eye strain can occur. Note that the symptoms of motion sickness are not only caused be external (exogenous), physical, and/or visual motion, but may also be brought about in the absence of these stressors in the case of defects within the vestibular system, causing (endogenous) motion illusions. Adapted from [56].
2.2. Sickness versus Eyestrain
One detail regarding Figure 1 concerns the interaction between motion sickness and eyestrain. As stated above, consensus is growing on the importance of a vestibular–expectation conflict to understand and predict motion sickness. In virtual environments, the vestibular–expectation conflict is often caused by a difference in visually and vestibularly perceived self-motion, and is typically referred to as a visual–vestibular conflict. At the same time, visual conflicts often occur in virtual environments, which lead to eyestrain and may even exist when viewing still images. A factor of interest in these visual conflicts is the accommodation–(con)vergence conflict. In real life, looking at objects located at different distances is accompanied by coupled changes in vergence (the angle between the visual axes of both eyes) and in accommodation (changes in the focal length of the ocular lenses by changing curvature). In artificial stereoscopy, such as in VR goggles, this relationship is disturbed (e.g., see [57]). A perception of depth is then created by presenting different images to both eyes, all taken from a slightly different perspective, causing the eyes to converge or diverge. At the same time, however, in all commercially available apparatus these virtual images are projected at a fixed distance, not only on a display and viewed through additional lenses within a head-mounted device, but also on a projection screen using projectors. The latter requires the eye lenses to remain focused at a fixed distance, while the eyes should be free to converge and diverge. This causes a conflict for the brain that expresses itself by means of “tired eyes”, headaches, and blurred vision, typical symptoms for eyestrain [58]. There hence seem to be two different conflicts at issue in explaining motion sickness on the one hand and eyestrain on the other hand. The fact that eyestrain is considered a symptom of motion sickness too (see, e.g., below about the SSQ) can be understood by assuming that if our brain is in conflict about accommodation and convergence cues, this can also affect our depth perception, thus potentially causing a visual–vestibular conflict [56]. This topic has hardly been studied and should be considered for further clarification.
3. Methodological Considerations
In studying the causes of motion sickness, various methodological issues need to be considered. In this section, we focus on how to measure motion sickness itself and on the importance of taking the large variability in motion sickness susceptibility into account. The various factors that play a role in causing and modulating motion sickness will be described in the next section on the gaps in our current understanding of motion sickness.
3.1. Measuring Motion Sickness
The ISO 2631-1 standard only considers emesis as a measure of motion sickness. It predicts the proportion of people that is expected to reach emesis due to exposure to vertical motion with a known frequency characteristic for up to 6 h, referred to as the Motion Sickness Incidence (MSI) as defined by [12]. This outcome measure is useful for seasickness, wherein people are typically exposed to motion during long periods of time without the ability to change or escape the motion stimulus. Consequently, seasickness often leads to emesis at some point in time. However, it ignores the great variety in signs and symptoms that can occur in motion sickness. These symptoms include epigastric awareness or discomfort, drowsiness, lethargy, dizziness, (cold) sweating, flushing, pallor, increased salivation, burping, flatulence, headache, and blurred vision, symptoms which typically precede nausea and emesis [2,27,59,60,61]. The MSI is also less useful for measuring motion sickness that occurs with other types of motion, for instance in cars. Carsickness is less likely to lead to emesis than seasickness, because trips are typically shorter and drivers can adjust their driving behavior in response to passenger complaints, or pause driving altogether. Consequently, only counting the instances of emesis is likely to underestimate the prevalence of carsickness. Similar arguments hold for other forms of motion sickness, such as simulator sickness, cybersickness, or VIMS. With respect to the frequency weighting as applied by ISO 2631-1, it may, for example, be assumed that the weighting function representative for human sensitivity to sickness will show more power at lower and higher frequencies when also covering these symptoms as compared to the current weighting which is valid for emesis only.
Given its variability in signs and symptoms, motion sickness has been termed a multidimensional construct [2,62,63,64]. Therefore, several rating scales have been suggested to measure the occurrence and severity of motion sickness on multiple dimensions. One of the earliest, the Pensacola Diagnostic Index (PDI), determines one single composite score for motion sickness, based on the subjective evaluation by participants of several dimensions covering the symptoms mentioned above [65]. In a similar vein, [66] introduced the Simulator Sickness Questionnaire (SSQ), which rates simulator sickness on three main dimensions: nausea, oculomotor, and disorientation, which can be combined in a single total score. These dimensions were labeled based on a factor analysis of specific symptoms pointing to the assumed dominant factors describing these symptoms. Although nausea seems to be specifically related to motion sickness and the other two dimensions seem to be more related to visual factors, this mapping is not necessarily straightforward and does require further research. Accommodation–convergence conflicts, for example, can be assumed to contribute heavily to the ocular symptoms (see above), but may affect depth of perception as well, hence also causing a visual–vestibular conflict. [67] identified four different dimensions that underlie various descriptions of motion sickness symptoms and termed these gastrointestinal, central, peripheral, and sopite-related dimensions of motion sickness. The latter is typically related to drowsiness and lethargy [68,69]. This analysis formed the basis for their 16-item Motion Sickness Assessment Questionnaire (MSAQ), which also allows for the determination of one total motion sickness score.
Although these multidimensional scales allow for a comprehensive measurement of subjective motion sickness symptoms, administering them takes time and may interfere with a task deployed during the sickening motion exposure in field or sea trials as well as in lab trials. In addition, the combination of categories and degrees of severity in, for instance, the PDI puts a considerable memory load on participants, as well as requiring clear instructions with respect to how to rate symptom severity. Therefore, these multidimensional scales are less suited for fast and repeated ratings of motion sickness during motion exposure and seem more appropriate for evaluating the motion sickness endpoint after motion exposure ends.
As an alternative, single-item illness ratings have been proposed (e.g., [70]). Some of these, such as the 11-point Misery Scale (MISC), originally proposed by [71] and further developed by [59,61], and the 7-point rating scale by [22] combine a fixed ordering of symptoms and severity into a single rating scale. These are based on the observation that symptoms of motion sickness usually progress in a fixed order over time, with nausea, retching, and emesis most often following the other symptoms [61,72]. Other scales, such as the 21-point Fast Motion Sickness Scale (FMS) proposed by [73], only reflect changes in discomfort or unpleasantness caused by motion sickness, without referring to specific symptoms. [61] recently showed that symptomatology as rated by the MISC does accumulate monotonously over time (at least when habituation is not at issue), while the FMS does not. As a consequence, they also observed that unpleasantness, not only as rated by the FMS but in other ways as well, increases with symptomatology, except at the onset of nausea when unpleasantness shortly decreases. This suggests that, although nausea typically follows after other symptoms such as headache, it is considered less unpleasant than (severe) headache. This also implies that unpleasantness can be predicted by symptomatology, but symptomatology cannot be predicted from unpleasantness. A practical consequence is that unpleasantness has less predictive value for the moment of emesis than does symptomatology. Altogether, this strongly speaks in favor of extending ISO 2631-1 by including the entire range of symptoms associated with motion sickness, instead of considering emesis only. In addition, consensus to use one common rating scale would allow for a better comparability of the results of different studies than is currently the case.
A disadvantage of rating symptomatology may be the fact that it requires a subjective response to a predefined question. For that reason, there have been several efforts to measure motion sickness by means of physiological correlates, such as changes in heart rate, skin conductance and temperature, respiratory rate and the occurrence of sighing or yawning, gastrointestinal activity, pupil and eye movements, as well as in various blood markers [74,75,76,77,78,79]. Having a measure of motion sickness based on these physiological changes would allow for the continuous monitoring of motion sickness, ideally in an inobtrusive way. A usable and valid measure should exhibit both high sensitivity, ability to detect motion sickness when it occurs, and high specificity, not detecting motion sickness when it is not present. However, to the best of our knowledge, no general measure based on either a single physiological marker or a metric based on a combination of multiple markers has been found which exhibits both good sensitivity and specificity to motion sickness. Though some measures have been found to correlate moderately well with subjective motion sickness ratings, autonomic arousal responses to motion sickness vary widely between persons and situations, limiting their sensitivity [80,81,82]. At the same time, these autonomic responses do not only occur with motion sickness, but with numerous other stressors unrelated to motion (e.g., high ambient temperature, cognitive load, emotional stress), limiting their specificity (e.g., see [72,83]). Possibly, new approaches obtaining facial characteristics from video and thermographic images may improve sensitivity and specificity (e.g., [78,84]).
3.2. Motion Sickness Susceptibility
While a functioning vestibular system appears to be a prerequisite for motion sickness to occur [27,85,86], people vary widely in their susceptibility or predisposition to motion sickness [2,87,88]. Susceptibility to motion sickness likely has an important genetic component [89,90,91]. Two factors that are commonly cited in the literature to contribute to differences in motion sickness susceptibility are gender and age.
3.2.1. Gender
A recent meta-analysis showed that females are significantly more likely to report having suffered from motion sickness in the past than males, as well as to rate motion sickness as more severe when exposed to motion sickness-inducing stimuli in experiments [92]. Yet, the difference between males and females was found to be larger for reports of past motion sickness than for present severity ratings. This is in agreement with numerous older studies not contained in the meta-analysis by [92], which also reported a higher incidence of emesis and higher illness ratings by women for seasickness (e.g., [17,19,29,93], as well as studies on carsickness [26]. Although it has been argued that at least part of the susceptibility differences between males and females may be attributed to differences in body awareness and/or willingness to report symptoms of motion sickness, this has also been doubted [5]. However, the fact that women not only report more subjective symptoms of motion sickness, but also include vomiting in said symptoms more often than males do [19] suggests that this cannot be the entire explanation (see also [94]). Self-selection in study participation is also unlikely to explain the difference [95]. Hormonal causes have been suggested for the increased susceptibility in women [96], supported by the finding that motion sickness susceptibility fluctuates with women’s menstrual cycle [96,97], and is increased around the time of menopause [98]. However, to date, there is no complete explanation for the gender difference in motion sickness susceptibility [92].
3.2.2. Age
Susceptibility to motion sickness has been reported to peak in prepuberty and decrease thereafter [99,100], though this peak may occur later for males than for females [29]. Infants and young children very rarely suffer from motion sickness in the first years of life [100]. The international survey on carsickness by [26], confirmed that the decrease in motion sickness susceptibility in post-puberty continues with increasing age for adults (from 18 to over 50 years), and a similar decrease has been reported for seasickness [29,101]. Interestingly, susceptibility to visually induced motion sickness (VIMS) and cybersickness appears to show the opposite trend, being higher for older persons [92]. Though the age dependency for VIMS and cybersickness is not as well established as for other types of motion sickness (see [102]), the difference between the two may be due to differences in exposure frequency and, consequently, habituation [92]. Moreover, in cybersickness other factors often play a role in addition to physically induced motion sickness, such as visualization latencies and visual conflicts (e.g., [103,104]).
3.2.3. Measuring Susceptibility
Motion sickness susceptibility is typically measured by taking someone’s history of motion sickness. The appropriately named Motion Sickness Susceptibility Questionnaire is the most commonly used method. Originally proposed by [27], it has been adapted and simplified by [88,105]. It quantifies the occurrence and frequency of motion sickness with different types of transportation, moving playground toys, and funfair rides, both as a child and in the recent past, corrected for the amount of exposure to these stimuli. Population norms for the MSSQ have been updated by [106]. The older Pensacola Motion Sickness Questionnaire [107] is also used to quantify susceptibility. Unsurprisingly, motion sickness susceptibility scores generally correlate highly with motion sickness ratings when exposed to motion stimuli (e.g., [59,108,109]. However, susceptibility to one kind of motion sickness (e.g., cross-coupled motion) does not necessarily imply high susceptibility to other kinds (e.g., due to linear acceleration) [87]. In addition, frequent or prolonged exposure to a given motion stimulus reduces motion sickness susceptibility for that stimulus through habituation [101,110].
3.2.4. Impact of Susceptibility
Failing to take the variability in motion sickness susceptibility into account may reduce both the internal and external validity of experiments on motion sickness. Co-variation of experimental factors with susceptibility through inadequate participant sampling or assignment may modulate effect sizes or even reverse effects, as motion sickness as measured may correlate stronger with motion sickness susceptibility than with the experimental manipulation itself. In order to increase chances of inducing motion sickness, researchers may choose to select participants with higher-than-average susceptibility, based on their history of motion sickness. This, however, limits the possibilities to generalize the results to the population at large. Moreover, participants may self-select in choosing whether to participate in experiments in which they expect to feel sick. Although, somewhat surprisingly, [95] reported this not to be the case in their study, this remains a potential issue for generalizing the results of motion sickness experiments beyond the study sample. Besides potential problems with experimental validity when not taking motion sickness susceptibility of participants into account, it may also reduce the reliability of motion sickness predictions, using models such as those proposed in ISO 2631-1. While this standard mentions the possibility of using different values of parameter Km to reflect different susceptibility in males and females (see Equation (2)), it remains to be seen whether such a simple account still holds when considering the broad range of motion sickness symptoms, visual factors, and other non-linear phenomena not yet considered by ISO 2631-1.
4. Knowledge Gaps and Steps towards an Enhanced Motion Sickness Standard
Although the literature on seasickness has uncovered and quantified several factors in the causation of motion sickness, it is still largely unknown how these generalize to other forms of motion sickness or which other factors may play a role. This section discusses the most important gaps in our knowledge of motion sickness, which are not covered by the current ISO 2631-1 standard. In our opinion, these gaps need to be addressed in order to develop a new standard that encompasses the various forms of motion sickness and is able to quantitatively predict motion sickness for different forms of motion. Based on this, Section 5 will lastly elaborate on the main steps toward a new, enhanced standard for motion sickness.
4.1. Motion Axes and Interactions
4.1.1. Linear Accelerations
Motion sickness prediction according to ISO 2631-1 was originally developed to be applicable to motion in ships and other vessels. As such, it considers vertical (z) motion only. The model has not been validated for horizontal motion, both fore–aft (x) and lateral (y), which is of particular concern in road transport. Several studies have shown that horizontal motion is more nauseating than would be predicted based on vertical motion [111,112,113]. Furthermore, the frequency dependence of motion in the horizontal plane may be different from that of vertical motion as specified in ISO 2631-1 [114,115,116,117].
4.1.2. Angular Motions
In addition, rotational motion is not considered in the current standard. To date, research regarding rotational motion is limited, but, similarly to horizontal motion and as described above, it cannot be estimated by the current standard. The severity of rotational motion has been shown to differ for different axes [45,71], and exhibits a different frequency dependency [118]. This suggests that the mechanisms that mediate the motion sickness under pure roll oscillation may be different from horizontal oscillation [119].
4.1.3. Interactions
Motion axes interactions are also not currently considered. However, research suggests their possible occurrence. Significant interaction effects of combined vertical and angular motion have been reported, while each of these motions studied separately were hardly provocative [71]. Similarly, studies on the effect of lateral and roll oscillation have shown that low levels of sickness were reported with pure roll or lateral oscillation [117,120]. However, when combined, significantly higher levels of sickness were reported [121], possibly due to linear and angular Coriolis effects, where in particular angular or (vestibular) cross-coupled Coriolis effects can be extremely nauseating [122].
Whilst the studies mentioned above provide useful data for comparing motion sickness in different motion axes and their interactions, these data are neither complete nor conclusive. Further research is required to establish the suitable frequency weighting that could be applied to evaluate the motion sickness for respective motion axes and their interactions. This includes other questions such as whether the effects of different motion frequencies add up linearly or whether they interact with each other (as suggested by the work of [16], and to what extent is the frequency weighting independent from the acceleration magnitude. This may also relate to the observation according to which the application of a non-sickening high-frequency vibration to the head reduces the sickening effect of a low-frequency motion [123]. Furthermore, part of the reason that comparisons across studies are problematic is due to the different measures of motion sickness used as well as the differences in experimental protocols. Future standardization activities shall pertain to these issues.
4.2. Temporal Dynamics
As per the current Standard, the MSDV increases with the square root of time. This implies an unlimited increase, or accumulation, of the MSI over time, while MSI, by definition, is limited to 100%. For that reason, ISO limits the exposure duration for valid predictions to periods in the range of 20 min to about 6 h, with the prevalence of emesis varying up to about 70% [18]. Although the 70% and the upper time limit seems appropriate for reckoning carsickness, the lower time limit may not be.
Related to but different from accumulation are the phenomena of habituation, i.e., an observed decrease in sickness with longer motion exposure durations [124], recovery [59], and retention [27], the latter of accumulation and habituation. These temporal effects remain largely unexplored, while still being important when dealing with longer lasting durations and repeated exposures. A specific point of interest concerns the predictability of motion per se. [16], for example, exposed subjects to several combinations of sinusoidal vertical motion, and did observe “unexpectedly high” motion sickness in certain combinations, an observation that also relates to the possible non-linear addition of frequency effects referred to above already. Similarly, it has been observed that accelerations and braking maneuvers that are perfectly predictable are less sickening than equal maneuvers occurring randomly [125]. To date, there is a dearth of knowledge with regard to these temporal aspects of motion sickness. Furthermore, as people vary in their susceptibility to motion sickness, the time course of motion sickness likely also shows large interindividual differences, which has so far hardly been investigated as well.
4.3. Modulating Factors
While motion per se is the primary cause of motion sickness, modulating factors refer to the factors that are able to regulate, adjust, or adapt motion sickness that would not cause sickness in the absence of motion. Yet, such factors are currently not incorporated into the standard. Here, we briefly describe three of them, again without any claim to be complete: vision, anticipation, and body orientation/posture.
4.3.1. Vision
The Standard was derived from data obtained in studies using participants having no view of the outside world. Due to the fact that the organs of balance are essential for motion sickness and vision is not, vision can be considered a modulating factor. Indeed, vision is known to be an important modulating factor [99,126,127,128], with the exact nature of the relationship between vision and motion sickness, however, yet to be determined. Outstanding questions concern, among other things, the relative importance of instantaneous visual information available to estimate body motion (direct visual–vestibular conflict) and the ability to anticipate future motion on the basis of the visual information [127,129,130]. In addition, frame information, that is, visual information to indicate horizontality and verticality [131], may also play a role, in particular in the absence of an outside view, or when using mere artificial imageries in VR or simulators [132].
A point of concern with respect to simulator sickness in moving base simulators relates in particular to the perceived coherence of visual and inertial motion, where generally (considerably) less platform motion is required than the visual imagery would require [132,133]. This topic too deserves more scrutiny, in particular with respect to motion sickness.
4.3.2. Anticipation and Expectation
The beneficial effect of vision has been attributed, at least partly, to the ability to anticipate the future motion trajectory [23,129]). To date, however, the true potential of such cues in reducing motion sickness is yet to be determined and requires further research into the relative effectiveness as a function of sensory modality, timing, and information detailing [130]. A particular point of concern is the effect of anticipatory cues requiring higher-order cognitive processing, such as the view on a curve ahead, different from the instantaneous effect of and visual cues about self-motion leading to vection and perceived self-tilt [46]. Another point of interest related to anticipation concerns the effect of a priori expectation. An equal small motion experienced aboard a ship that is expected to move may be not sickening, while it can be sickening when experienced on top of a high building that is not expected to move [134].
4.3.3. Body Orientation and Reclination
Body orientation relative to the direction of travel as well as reclination angles have been shown to affect motion sickness levels [128,135]. To date, only a few studies have explored these topics and indicate the need to better understand the role of passenger orientation and motion sickness. A specific point of interest, making matters likely even more complex, relate to dynamic seating, which may for example be an issue shortly before a transfer of control in intermediate levels of automation.
5. Discussion and Conclusions
An international standard for motion sickness promotes a common agreed-upon research methodology, allowing for better comparisons of results from different research labs. It should also provide a validated prediction model, making it possible to easily estimate and compare the effectiveness of different countermeasures. ISO 2631-1 provided a solid first step towards a general international standard on motion sickness. However, as we have argued above, it does not suffice anymore in this day and age, nearly four decades after the standard was first published.
First, it is primarily based on research on seasickness and therefore not necessarily applicable to other forms of motion sickness, such as cybersickness and simulator sickness, which include a visual component, or carsickness, which is largely caused by horizontal as opposed to vertical motion. Second, ISO 2631-1 only considers emesis as an outcome measure of motion sickness, ignoring the range of other symptoms and effects that are highly relevant in many contexts in which motion sickness may occur, thus also requiring guidelines on measurement. Third and lastly, it does not include some of the important factors that are now known to contribute or modulate motion sickness, such as susceptibility to and history of motion sickness, visual factors, anticipation, and body orientation.
Although we limited this paper to these factors, other factors not mentioned here may concern the effects of odors, ambient temperature, (pseudo) Coriolis and Purkinje effects, off-vertical axis rotations, G-transitions relevant for space travel and parabolic flight, and probably many more factors. In that respect, we did not intend to be complete, we rather intended to provide reasons for which the current ISO standard does not comply anymore with a desire for a standard that also covers motion sickness in conditions different from those at sea with a view on the interior only.
Moreover, the current ISO 2631-1 standard includes motion sickness as the last effect on humans caused by whole body vibration, only after the effects on health, comfort, and perception. Although this is in accordance with the ISO approach based on frequency weighting, with different weightings accounting for the different effects, it is not applicable when considering the specific effects of vision, anticipation, individual, and modulating factors typical for physically and visually induced motion sickness.
When adding the growing societal impact of motion sickness in transportation and VR, we therefore propose to remove motion sickness from the current ISO 2631-1 standard and develop a new dedicated and enhanced international standard on motion sickness in all of its manifestations. In order to provide a scientific basis and agreed-upon methodology for measurement and prediction, additional research is part of the process and the text box (Box 1) below provides some major issues. Given its incompleteness, this paper, lastly, aims at starting a discussion about the development of such a new standard, rather than presenting a blueprint thereof.
Box 1. Main research topics providing a scientific basis for a new standard on motion sickness
- Contribution of inertial acceleration amplitude and frequency along vertical and horizontal axes, including potential interactions;
- Contribution of visual (image) factors (a simple statement that may even be more complex than determining the contribution of the inertial factors);
- Prediction of sickness including the pre-emesis symptoms;
- Integration of various forms of motion sickness into one single prediction model;
- Time course of motion sickness (accumulation, habituation, recovery, retention);
- Inclusion of individual differences;
- Standardization of methodology for motion sickness research (sickness rating scales, motion stimuli, and individual difference and susceptibility ratings);
- Contribution of moderating factors besides vision, such as posture/orientation, anticipation/predictability, temperature, odors, etc.
Author Contributions
All authors contributed equally to this paper. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- ISO 2631-1; Mechanical Vibration and Shock—Evaluation of Human Exposure to Whole-Body Vibration—Part 1: General Requirements. International Organization for Standardization: Geneva, Switzerland, 1997.
- Lackner, J.R. Motion sickness: More than nausea and vomiting. Exp. Brain Res. 2014, 232, 2493–2510. [Google Scholar] [CrossRef] [PubMed]
- Bertolini, G.; Straumann, D. Moving in a Moving World: A Review on Vestibular Motion Sickness. Front. Neurol. 2016, 7, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Proietti, P.; Allsop, J.; Bloch, M.; Bos, J.E.; Burov, O.; Clement, D.; French, J.; Kirollos, R.; Lawson, B.D.; Leoncini, P.; et al. Guidelines for Mitigating Cybersickness in Virtual Reality Systems; Technical Report NATO Science and Technology Organisation, Human Factors and Medicine & Modeling and Simulation Group Specialist Team 323 2021 NATO STO-TR-HFM-MSG-323; NATO: Brussels, Belgium, 2021. [Google Scholar]
- Keshavarz, B.; Golding, J.F. Motion sickness: Current concepts and management. Curr. Opin. Neurol. 2022, 35, 107–112. [Google Scholar] [CrossRef] [PubMed]
- Alexander, S.J.; Cotzin, M.; Hill, C.J., Jr.; Ricciuti, E.A.; Wendt, G.R. Weslean University studies of motion sickness: I. The effects of variation of time intervals between accelerations upon sickness rates. J. Psychol. 1945, 19, 49–62. [Google Scholar] [CrossRef]
- Alexander, S.J.; Cotzin, M.; Hill, C.J., Jr.; Ricciuti, E.A.; Wendt, G.R. Weslean University studies of motion sickness: II. A second approach to the problem of the effects of the variation of time intervals between accelerations upon sickness rates. J. Psychol. 1945, 19, 63–68. [Google Scholar] [CrossRef]
- Alexander, S.J.; Cotzin, M.; Hill, C.J., Jr.; Ricciuti, E.A.; Wendt, G.R. Weslean University studies of motion sickness: III. The effects of various accelerations upon sickness rates. J. Psychol. 1945, 20, 3–8. [Google Scholar] [CrossRef]
- Alexander, S.J.; Cotzin, M.; Hill, C.J., Jr.; Ricciuti, E.A.; Wendt, G.R. Weslean University studies of motion sickness: IV. The effects of waves containing two acceleration levels upon sickness. J. Psychol. 1945, 20, 9–18. [Google Scholar] [CrossRef]
- Alexander, S.J.; Cotzin, M.; Hill, C.J., Jr.; Ricciuti, E.A.; Wendt, G.R. Weslean University studies of motion sickness: V. Incidence of sickness at various hours of the day. J. Psychol. 1945, 20, 19–24. [Google Scholar] [CrossRef]
- Alexander, S.J.; Cotzin, M.; Hill, C.J., Jr.; Ricciuti, E.A.; Wendt, G.R. Weslean University studies of motion sickness: VI. Prediction of sickness on a vertical acceleration by means of a motion sickness history questionnaire. J. Psychol. 1945, 20, 25–30. [Google Scholar] [CrossRef]
- Alexander, S.J.; Cotzin, M.; Hill, C.J., Jr.; Ricciuti, E.A.; Wendt, G.R. Weslean University studies of motion sickness: VII. The effects of sickness upon performance. J. Psychol. 1945, 20, 31–39. [Google Scholar] [CrossRef]
- Alexander, S.J.; Cotzin, M.; Klee, M.; Wendt, G.R. Studies of motion sickness. XVI. The effects upon sickness rates of waves of various frequencies but identical acceleration. J. Exp. Psychol. 1947, 37, 440–448. [Google Scholar] [CrossRef]
- O’Hanlon, J.F.; McCauley, M.E. Motion sickness incidence as a function of the frequency and acceleration of vertical sinusoidal motion. Aerosp. Med. 1974, 45, 366–369. [Google Scholar]
- McCauley, M.E.; Royal, J.W.; Wylie, C.D.; O’Hanlon, J.F.; Mackie, R.R. Motion Sickness Incidence: Exploratory Studies of Habituation, Pitch and Roll, and the Refinement of a Mathematical Model; Technical Report; Human Factors Research, Inc.: Goleta, CA, USA, 1976; Volume 1733–2, pp. 1–61. [Google Scholar]
- Guignard, J.C.; McCauley, M.E. Motion sickness incidence induced by complex periodic waveforms. Aviat. Space Environ. Med. 1982, 53, 554–563. [Google Scholar] [CrossRef]
- Lawther, A.; Griffin, M.J. The motion of a ship at sea and the consequent motion sickness amongst passengers. Ergonomics 1986, 29, 535–552. [Google Scholar] [CrossRef]
- Lawther, A.; Griffin, M.J. Prediction of the incidence of motion sickness from the magnitude, frequency and duration of vertical oscillation. J. Acoust. Soc. Am. 1987, 82, 957–966. [Google Scholar] [CrossRef]
- Lawther, A.; Griffin, M.J. A survey of the occurrence of motion sickness amongst passengers at sea. Aviat. Space Environ. Med. 1988, 59, 399–406. [Google Scholar]
- Lawther, A.; Griffin, M.J. Motion sickness and motion characteristics of vessels at sea. Ergonomics 1988, 31, 1373–1394. [Google Scholar] [CrossRef]
- BS 6841; Guide to Measurement and Evaluation of Human Exposure to Whole-Body Mechanical Vibration and Repeated Shock. British Standards Institution: London, UK, 2020.
- Griffin, M.J.; Newman, M.M. An experimental study of low-frequency motion in cars. Proc. Inst. Mech. Eng. Part D J. Automob. Eng. 2004, 218, 1231–1238. [Google Scholar] [CrossRef]
- Rolnick, A.; Lubow, R.E. Why is the driver rarely motion sick? The role of controllability in motion sickness. Ergonomics 1991, 34, 867–879. [Google Scholar] [CrossRef]
- Diels, C. Will autonomous vehicles make us sick? In Contemporary Ergonomics and Human Factors; Sharples, S.M., Shorrock, S., Eds.; Taylor & Francis: Abingdon, UK, 2014; pp. 301–307. [Google Scholar]
- Diels, C.; Bos, J.E. Self-driving carsickness. Appl. Ergon. Part B 2016, 53, 374–382. [Google Scholar] [CrossRef]
- Schmidt, E.A.; Kuiper, O.X.; Wolter, S.; Diels, C.; Bos, J.E. An international survey on the incidence and modulating factors of carsickness. Transp. Res. Part F Traffic Psychol. Behav. 2020, 71, 76–87. [Google Scholar] [CrossRef]
- Reason, J.T.; Brand, J.J. Motion Sickness; Academic Press: London, UK, 1975. [Google Scholar]
- Bos, J.E. Motion sickness, simulator sickness, and automated vehicles. In Proceedings of the Driving Simulation and Virtual Reality Conference Europe, Antibes, France, 5–7 September 2018. [Google Scholar]
- Bos, J.E.; Damala, D.; Lewis, C.; Ganguly, A.; Turan, O. Susceptibility to seasickness. Ergonomics 2007, 50, 890–901. [Google Scholar] [CrossRef] [PubMed]
- Irwin, J.A. The pathology of seasickness. Lancet 1881, 2, 907–909. [Google Scholar] [CrossRef]
- James, W. The sense of dizziness in deaf-mutes. Am. J. Otol. 1882, 4, 239–254. [Google Scholar]
- Kennedy, R.S.; Graybiel, A.; McDonough, R.C.; Beckwith, F.D. Symptomatology under storm conditions in the North Atlantic in control subjects and in persons with bilateral labyrinthine defects. Acta Otolaryngol. 1968, 66, 533–540. [Google Scholar] [CrossRef] [PubMed]
- Graybiel, A. Susceptibility to acute motion sickness in blind persons. Aerosp. Med. 1970, 41, 650–653. [Google Scholar]
- Hettinger, L.J.; Kennedy, R.S.; Berbaum, K.S. Tracing the etiology of simulator sickness. Simul. Ser. 1987, 18, 105–108. [Google Scholar]
- Gower, D.W.; Lilienthal, M.G.; Kennedy, R.S.; Fowlkes, J.E. Simulator sickness in U.S. Army and Navy fixed- and rotary-wing flight simulators. In Proceedings of the AGARD Medical Panel Symposium on Motion Cues in Flight Simulation and Simulator Induced Sickness, Brussels, Belgium, 28 September–2 October 1987. [Google Scholar]
- Kennedy, R.S.; Lilienthal, M.G.; Berbaum, K.S.; Baltzley, D.R.; McCauley, M.E. Simulator sickness in U.S. Navy flight simulators. Aviat. Space Environ. Med. 1989, 60, 10–16. [Google Scholar]
- Stanney, K.; Lawson, B.D.; Rokers, B.; Dennison, M.; Fidopiastis, C.; Stoffregen, T.; Weech, S.; Fulvio, J.M. Identifying causes of and solutions for cybersickness in immersive technology: Reformulation of a research and development agenda. Int. J. Hum. Comput. Interact. 2020, 36, 1783–1803. [Google Scholar] [CrossRef]
- Caserman, P.; Garcia-Agundez, A.; Gamez Zerban, A.; Goebel, S. Cybersickness in current-generation virtual reality head-mounted displays: Systematic review and outlook. Virtual Real. 2021, 25, 1153–1170. [Google Scholar] [CrossRef]
- Reed, N.; Diels, C.; Parkes, A.M. Simulator sickness management: Enhanced familiarisation and screening processes. In Proceedings of the 1st International Symposium of Visually Induced Motion Sickness, Hong Kong, China, 10–11 December 2007; pp. 156–162. [Google Scholar]
- Cordes, C.; Heutink, J.; Brookhuis, K.A.; Brouwer, W.H.; Melis-Dankers, B.J.M. Driving slow motorised vehicles with visual impairment—A simulator study. Cogent Psychol. 2018, 5, 1485473. [Google Scholar] [CrossRef]
- Von Holst, E.; Mittelstaedt, H. Das Reafferenzprinzip. Naturwissenschaften 1950, 37, 464–476. [Google Scholar] [CrossRef]
- Reason, J.T. Motion sickness adaptation: A neural mismatch model. J. R. Soc. Med. 1978, 71, 819–829. [Google Scholar] [CrossRef]
- Oman, C.M. A heuristic mathematical model for the dynamics of sensory conflict and motion sickness. Acta Otolaryngol. Suppl. 1982, 392, 1–44. [Google Scholar] [CrossRef]
- Oman, C.M. Sensory conflict in motion sickness: An observer theory approach. In Pictorial Communication in Virtual and Real Environments, 2nd ed.; Ellis, S.R., Kaiser, M.K., Grunwald, A.J., Eds.; Taylor & Francis: London, UK, 1993; pp. 362–376. [Google Scholar]
- Bles, W.; Bos, J.E.; De Graaf, B.; Groen, E.; Wertheim, A.H. Motion sickness: Only one provocative conflict? Brain Res. Bull. 1998, 47, 481–487. [Google Scholar] [CrossRef]
- Bos, J.E.; Bles, W.; Groen, E.L. A theory on visually induced motion sickness. Displays 2008, 29, 47–57. [Google Scholar] [CrossRef]
- Bos, J.E.; Bles, W. Modelling motion sickness and subjective vertical mismatch detailed for vertical motions. Brain Res. Bull. 1998, 47, 537–542. [Google Scholar] [CrossRef]
- Kamiji, N.; Kurata, Y.; Wada, T.; Doi, S. Modeling and validation of carsickness mechanism. In Proceedings of the Annual International Conference on Instrumentation, Control and Information Technology, Takamatsu, Japan, 17–20 September 2007; pp. 1138–1143. [Google Scholar]
- Ukita, R.; Okafuji, Y.; Wada, T. A simulation study on lane-change control of automated vehicles to reduce motion sickness based on a computational model. In Proceedings of the IEEE International Conference on Systems, Man, and Cybernetics, Melbourne, Australia, 17–20 October 2020. [Google Scholar]
- Wada, T. Computational model of motion sickness describing the effects of learning exogenous motion dynamics. Front. Syst. Neurosci. 2021, 15, 634604. [Google Scholar] [CrossRef]
- Wada, T.; Fujisawa, S.; Doi, S. Analysis of driver’s head tilt using a mathematical model of motion sickness. Int. J. Ind. Ergon. 2018, 63, 89–97. [Google Scholar] [CrossRef]
- Wada, T.; Kawano, J.; Okafuji, Y.; Takamatsu, A.; Mitsuhiro, M. A computational model of motion sickness considering visual and vestibular information. In Proceedings of the IEEE International Conference on Systems, Man, and Cybernetics, Melbourne, Australia, 17–20 October 2020. [Google Scholar]
- Riccio, G.E.; Stoffregen, T.A. An ecological theory of motion sickness and postural instability. Ecol. Psychol. 1991, 3, 195–240. [Google Scholar] [CrossRef]
- Stoffregen, T.A.; Riccio, G.E. An ecological critique of the sensory conflict theory of motion sickness. Ecol. Psychol. 1991, 3, 159–194. [Google Scholar] [CrossRef]
- Bos, J.E. Nuancing the relationship between motion sickness and postural stability. Displays 2011, 32, 189–193. [Google Scholar] [CrossRef]
- Bos, J.E.; Lawson, B.D.; Allsop, J.; Rigato, P.; Secci, S. Chapter 2: Introduction. In Guidelines for Mitigating Cybersickness in Virtual Reality Systems; NATO STO, Report of the Human Factors and Medicine Panel/Modelling and Simulation Group 2021a, Activity number 323, NATO STO-TR-HFM-MSG-323; Proietti, P., Ed.; NATO: Brussels, Belgium, 2021. [Google Scholar]
- Rushton, S.K.; Riddell, P.M. Developing visual systems and exposure to virtual reality and stereo displays: Some concerns and speculations about the demands on accommodation and vergence. Appl. Ergon. 1999, 30, 69–78. [Google Scholar] [CrossRef]
- Lambooij, M.; Fortuin, M.; Heynderickx, I.; IJsselsteijn, W. Visual Discomfort and Visual Fatigue of Stereoscopic Displays: A Review. J. Imaging Sci. Technol. 2009, 53, 30201-1. [Google Scholar] [CrossRef]
- Bos, J.E.; MacKinnon, S.N.; Patterson, A. Motion Sickness Symptoms in a Ship Motion Simulator: Effects of Inside, Outside, and No View. Aviat. Space Environ. Med. 2005, 76, 1111–1118. [Google Scholar] [PubMed]
- Lawson, B.D. Motion Sickness Symptomatology and Origins. In Handbook of Virtual Environments: Design, Implementation, and Applications, 2nd ed.; Hale, K.S., Stanney, K.M., Eds.; CRC Press: Boca Raton, FL, USA, 2014; pp. 531–600. [Google Scholar]
- Reuten, A.J.C.; Nooij, S.A.E.; Bos, J.E.; Smeets, J.B.J. How feelings of unpleasantness develop during the progression of motion sickness symptoms. Exp. Brain Res. 2021, 239, 3615–3624. [Google Scholar] [CrossRef]
- Muth, E.R.; Stern, R.M.; Thayer, J.F.; Koch, K.L. Assessment of the multiple dimensions of nausea: The Nauea Profile (NP). J. Psychosom. Res. 1996, 40, 511–520. [Google Scholar] [CrossRef]
- Balaban, C.D.; Yates, B.J. What is nausea? A historical analysis of changing views. Auton. Neurosci. Basic Clin. 2017, 202, 5–17. [Google Scholar] [CrossRef]
- Cha, Y.H.; Golding, J.F.; Keshavarz, B.; Furman, J.; Kim, J.S.; Lopez-Escamez, J.A.; Magnusson, M.; Yates, B.J.; Lawson, B.D. Motion sickness diagnostic criteria: Consensus document of the classification committee of the Barany Society. J. Vestib. Res. 2021, 31, 327–344. [Google Scholar] [CrossRef]
- Graybiel, A.; Wood, C.D.; Miller, E.F.; Dewy, B.; Cramer, D.B. Diagnostic criteria for grading the severity of acute motion sickness. Aerosp. Med. 1968, 39, 453–455. [Google Scholar]
- Kennedy, R.S.; Lane, N.E.; Berbaum, K.S.; Lilienthal, M.G. Simulator Sickness Questionnaire: An enhanced method for quantifying simulator sickness. Int. J. Aviat. Psychol. 1993, 3, 203–220. [Google Scholar] [CrossRef]
- Gianaros, P.J.; Muth, E.R.; Mordkoff, J.T.; Levine, M.E.; Stern, R.M. A Questionnaire for the Assessment of the Multiple Dimensions of Motion Sickness. Aviat. Space Environ. Med. 2001, 72, 115–119. [Google Scholar] [PubMed]
- Graybiel, A.; Knepton, J. Sopite syndrome: A sometimes sole manifestation of motion sickness. Aviat. Space Environ. Med. 1976, 47, 873–882. [Google Scholar] [PubMed]
- Matsangas, P.; McCauley, M.E. Sopite syndrome: A revised definition. Aviat. Space Environ. Med. 2014, 85, 672–673. [Google Scholar] [CrossRef] [PubMed]
- Lawson, B.D. Motion sickness scaling. In Handbook of Virtual Environments: Design, Implementation and Applications, 2nd ed.; Hale, K.S., Stanney, K.M., Eds.; CRC Press: Boca Raton, FL, USA, 2014; pp. 601–623. [Google Scholar]
- Wertheim, A.H.; Bos, J.E.; Bles, W. Contributions of roll and pitch to sea sickness. Brain Res. Bull. 1998, 47, 517–524. [Google Scholar] [CrossRef]
- Shupak, A.; Gordon, C.R. Motion Sickness: Advances in Pathogenesis, Prediction, Prevention, and Treatment. Aviat. Space Environ. Med. 2006, 77, 1213–1223. [Google Scholar]
- Keshavarz, B.; Hecht, H. Validating an Efficient Method to Quantify Motion Sickness. Hum. Factors J. Hum. Factors Ergon. Soc. 2011, 53, 415–426. [Google Scholar] [CrossRef]
- Kennedy, R.S.; Frank, L.H. Review of motion sickness with special reference to simulator sickness. Transp. Res. Rec. 1985, 1059, 75–79. [Google Scholar]
- Gavgani, A.M.; Nesbitt, K.V.; Blackmore, K.L.; Nalivaiko, E. Profiling subjective symptoms and autonomic changes associated with cybersickness. Auton. Neurosci. 2017, 203, 41–50. [Google Scholar] [CrossRef]
- Romano, F.; Caramia, N.; Straumann, D.; Nalivaiko, E.; Bertolini, G. Cross-coupling vestibular stimulation: Motion sickness and the vestibulo-sympathetic reflex. J. Neurol. 2017, 264 (Suppl. S1), 96–103. [Google Scholar] [CrossRef]
- Irmak, T.; Pool, D.M.; Happee, R. Objective and subjective responses to motion sickness: The group and the individual. Exp. Brain Res. 2021, 239, 515–531. [Google Scholar] [CrossRef]
- Keshavarz, B.; Peck, K.; Rezaei, S.; Taati, B. Detecting and predicting visually induced motion sickness with physiological measures in combination with machine learning techniques. Int. J. Psychophysiol. 2022, 176, 14–26. [Google Scholar] [CrossRef]
- Li, C.; Zhang, Z.; Liu, Y.; Zhang, T.; Zhang, X.; Wang, H.; Wang, X. Multi-Dimensional and Objective Assessment of Motion Sickness Susceptibility Based on Machine Learning. Front. Neurol. 2022, 13, 824670. [Google Scholar] [CrossRef]
- Stout, C.S.; Toscano, W.B.; Cowings, P.S. Reliability of Autonomic Responses and Malaise across Multiple Motion Sickness Stimulation Tests; NASA-TM-108787; NASA Ames Research Center: Mountain View, CA, USA, 1993. [Google Scholar]
- Dahlman, J.; Sjörs, A.; Lindström, J.; Ledin, T.; Falkmer, T. Performance and Autonomic Responses during Motion Sickness. Hum. Factors J. Hum. Factors Ergon. Soc. 2009, 51, 56–66. [Google Scholar] [CrossRef]
- Smyth, J.; Birrell, S.; Woodman, R.; Jennings, P. Exploring the utility of EDA and skin temperature as individual physiological correlates of motion sickness. Appl. Ergon. 2021, 92, 103315. [Google Scholar] [CrossRef]
- Koohestani, A.; Nahavandi, D.; Asadi, H.; Kebria, P.M.; Khosravi, A.; Alizadehsani, R.; Nahavandi, S. A Knowledge Discovery in Motion Sickness: A Comprehensive Literature Review. IEEE Access 2019, 7, 85755–85770. [Google Scholar] [CrossRef]
- Lee, J.D.; Alsaid, A. A Machine Vision Approach for Estimating Motion Discomfort in Simulators and in Self-Driving; SAFER-SIM University Transport Center: Iowa City, IA, USA; University of Madison: Madison, WI, USA, 2019. [Google Scholar]
- Money, K.E. Motion Sickness. Physiol. Rev. 1970, 50, 1–39. [Google Scholar] [CrossRef]
- Cheung, B.S.K.; Howard, I.P.; Money, K.E. Visually-induced sickness in normal and bilaterally labyrinthine-defective subjects. Aviat. Space Environ. Med. 1991, 62, 527–531. [Google Scholar]
- Golding, J.F. Motion sickness susceptibility. Auton. Neurosci. 2006, 129, 67–76. [Google Scholar] [CrossRef]
- Golding, J.F. Predicting individual differences in motion sickness susceptibility by questionnaire. Personal. Individ. Differ. 2006, 41, 237–248. [Google Scholar] [CrossRef]
- Sharma, K. Susceptibility to Motion Sickness. Acta Genet. Med. Gemellol. Twin Res. 1980, 29, 157–162. [Google Scholar] [CrossRef] [PubMed]
- Reavley, C.M.; Golding, J.F.; Cherkas, L.F.; Spector, T.D.; MacGregor, A.J. Genetic Influences on Motion Sickness Susceptibility in Adult Women: A Classical Twin Study. Aviat. Space Environ. Med. 2006, 77, 1148–1152. [Google Scholar] [PubMed]
- Hromatka, B.S.; Tung, J.Y.; Kiefer, A.K.; Do, C.B.; Hinds, D.A.; Eriksson, N. Genetic variants associated with motion sickness point to roles for inner ear development, neurological processes, and glucose homeostasis. Hum. Mol. Genet. 2015, 24, 2700–2708. [Google Scholar] [CrossRef] [PubMed]
- Mittelstaedt, J.M. Individual predictors of the susceptibility for motion-related sickness: A systematic review. J. Vestib. Res. 2020, 30, 165–193. [Google Scholar] [CrossRef] [PubMed]
- Turner, M.; Griffin, M.J. Motion Sickness Incidence during a Round-The-World Yacht Race. Aviat. Space Environ. Med. 1995, 66, 849–856. [Google Scholar]
- Dobie, T.; McBride, D.; Dobie, T., Jr.; May, J. The effects of age and sex on susceptibility to motion sickness. Aviat. Space Environ. Med. 2001, 72, 13–20. [Google Scholar]
- Flanagan, M.B.; Alvarado, E.; May, J.G.; Dobie, T.G. Sex differences in tolerance to visually induced motion sickness. Aviat. Space Environ. Med. 2001, 76, 642–646. [Google Scholar]
- Golding, J.F.; Kadzere, P.; Gresty, M.A. Motion Sickness Susceptibility Fluctuates through the Menstrual Cycle. Aviat. Space Environ. Med. 2005, 76, 970–973. [Google Scholar]
- Grunfeld, E.; Gresty, M.A. Relationship between motion sickness, migraine and menstruation in crew members of a “round the world” yacht race. Brain Res. Bull. 1998, 47, 433–436. [Google Scholar] [CrossRef]
- Paillard, A.C.; Quarck, G.; Paolino, F.; Denise, P.; Paolino, M.; Golding, J.F.; Ghulyan-Bedikian, V. Motion sickness susceptibility in healthy subjects and vestibular patients: Effects of gender, age and trait-anxiety. J. Vestib. Res. 2013, 23, 203–209. [Google Scholar] [CrossRef]
- Turner, M.; Griffin, M.J. Motion sickness in public road transport: Passenger behaviour and susceptibility. Ergonomics 1999, 42, 444–461. [Google Scholar] [CrossRef]
- Huppert, D.; Grill, E.; Brandt, T. Survey of motion sickness susceptibility in children and adolescents aged 3 months to 18 years. J. Neurol. 2019, 266 (Suppl. S1), 65–73. [Google Scholar] [CrossRef]
- Besnard, S.; Bois, J.; Hitier, M.; Vogt, J.; Laforet, P.; Golding, J.F. Motion Sickness Lessons from the Southern Ocean. Aerosp. Med. Hum. Perform. 2021, 92, 720–727. [Google Scholar] [CrossRef]
- Saredakis, D.; Szpak, A.; Birckhead, B.; Keage, H.A.D.; Rizzo, A.; Loetscher, T. Factors Associated with Virtual Reality Sickness in Head-Mounted Displays: A Systematic Review and Meta-Analysis. Front. Hum. Neurosci. 2020, 14, 96. [Google Scholar] [CrossRef]
- Hurter, J.; Maraj, C.; Murphy, S. Commercial virtual reality displays: Issues of performance and simulator sickness from exocentric depth-perception tasks. Displays 2021, 70, 102095. [Google Scholar] [CrossRef]
- Zhou, Y.; Zhang, J.; Fang, F. Vergence-accommodation conflict in optical see-through display: Review and prospect. Results Opt. 2021, 5, 100160. [Google Scholar] [CrossRef]
- Golding, J.F. Motion sickness susceptibility questionnaire revised and its relationship to other forms of sickness. Brain Res. Bull. 1998, 47, 507–516. [Google Scholar] [CrossRef]
- Lamb, S.; Kwok, K.C.S. MSSQ-Short Norms May Underestimate Highly Susceptible Individuals: Updating the MSSQ-Short Norms. Hum. Factors J. Hum. Factors Ergon. Soc. 2015, 57, 622–633. [Google Scholar] [CrossRef]
- Kennedy, R.S.; Graybiel, A. The Dial Test: A Standardized Procedure for the Experimental Production of Canal Sickness Symptomatology in a Rotating Environment; U.S. Naval School of Aviation Medicine: Pensacola, FL, USA, 1965; NSAM 113. [Google Scholar]
- Stanney, K.M.; Hale, K.S.; Nahmens, I.; Kennedy, R.S. What to Expect from Immersive Virtual Environment Exposure: Influences of Gender, Body Mass Index, and Past Experience. Hum. Factors J. Hum. Factors Ergon. Soc. 2003, 45, 504–520. [Google Scholar] [CrossRef]
- Nooij, S.A.E.; Bockisch, C.J.; Bülthoff, H.H.; Straumann, D. Beyond sensory conflict: The role of beliefs and perception in motion sickness. PLoS ONE 2021, 16, e0245295. [Google Scholar] [CrossRef]
- Howarth, P.A.; Hodder, S.G. Characteristics of habituation to motion in a virtual environment. Displays 2008, 29, 117–123. [Google Scholar] [CrossRef]
- Golding, J.F.; Markey, H.M.; Stott, J.R.R. The effects of motion direction, body axis, and posture on motion sickness induced by low frequency linear oscillation. Aviat. Space Environ. Med. 1995, 66, 1046–1051. [Google Scholar] [PubMed]
- Golding, J.F.; Markey, H.M. Effect of frequency of horizontal linear oscillation on motion sickness and somatogravic illusion. Aviat. Space Environ. Med. 1996, 67, 121–126. [Google Scholar] [PubMed]
- Golding, J.F.; Finch, M.I.; Stott, J.R.R. Frequency effect of 0.35–1.0 hz horizontal translational oscillation on motion sickness and the somatogravic illusion. Aviat. Space Environ. Med. 1997, 68, 396–402. [Google Scholar] [PubMed]
- Golding, J.F.; Phil, D.; Mueller, A.G.; Gresty, M.A. A motion sickness maximum around the 0.2 Hz frequency range of horizontal translational oscillation. Aviat. Space Environ. Med. 2001, 72, 188–192. [Google Scholar]
- Griffin, M.J.; Mills, K.L. Effect of frequency and direction of horizontal oscillation on motion sickness. Aviat. Space Environ. Med. 2002, 73, 537–543. [Google Scholar]
- Griffin, M.J.; Mills, K.L. Effect of magnitude and direction of horizontal oscillation on motion sickness. Aviat. Space Environ. Med. 2002, 73, 640–646. [Google Scholar]
- Donohew, B.E.; Griffin, M.J. Motion sickness: Effect of the frequency of lateral oscillation. Aviat. Space Environ. Med. 2004, 75, 649–656. [Google Scholar]
- Butler, C.; Griffin, M.J. Motion sickness with combined fore-aft and pitch oscillation: Effect of phase and the visual scene. Aviat. Space Environ. Med. 2009, 80, 946–954. [Google Scholar] [CrossRef]
- Howarth, H.V.C.; Griffin, M.J. Effect of roll oscillation frequency on motion sickness. Aviat. Space Environ. Med. 2003, 74, 326–331. [Google Scholar]
- Joseph, J.A.; Griffin, M.J. Motion sickness: Effect of the magnitude of roll and pitch oscillation. Aviat. Space Environ. Med. 2008, 79, 390–396. [Google Scholar] [CrossRef]
- Donohew, B.E.; Griffin, M.J. Motion sickness with combined lateral and roll oscillation: Effect of percentage compensation. Aviat. Space Environ. Med. 2010, 81, 22–29. [Google Scholar] [CrossRef]
- Bles, W. Coriolis effects and motion sickness modelling. Brain Res. Bull. 1998, 47, 543–549. [Google Scholar] [CrossRef]
- Bos, J.E. Less sickness with more motion and/or mental distraction. J. Vestib. Res. 2015, 25, 23–33. [Google Scholar] [CrossRef]
- Golding, J.F.; Stott, J.R.R. Effect of sickness severity on habituation to repeated motion challenges in aircrew referred for airsickness treatment. Aviat. Space Environ. Med. 1995, 66, 625–630. [Google Scholar]
- Kuiper, O.X.; Bos, J.E.; Schmidt, E.A.; Diels, C.; Wolter, S. Knowing what’s coming: Unpredictable motion causes more sickness. Hum. Factors 2020, 62, 1339–1348. [Google Scholar] [CrossRef]
- Probst, T.; Krafczyk, S.; Buchele, W.; Brandt, T. Visuelle Praevention der Bewegungskrankheit im Auto. Arch. Psychiatr. Nervenkrankh. 1982, 231, 409–421. [Google Scholar] [CrossRef]
- Kuiper, O.X.; Bos, J.E.; Diels, C. Looking forward: In-vehicle auxiliary display positioning affects carsickness. Appl. Ergon. 2018, 68, 169–175. [Google Scholar] [CrossRef]
- Bohrmann, D.; Bengler, K. Reclined posture for enabling autonomous driving. In Proceedings of the International Conferance on Human Systems Engineering and Design (IHSE 2019), Munchen, Germany, 1–18 September 2020; Ahram, T., Ed.; Springer Nature: Cham, Switzerland, 2020; pp. 1–7. [Google Scholar]
- Kuiper, O.X.; Bos, J.E.; Schmidt, E.A.; Diels, C. Knowing what’s coming: Anticipatory audio cues can mitigate motion sickness. Appl. Ergon. 2020, 85, 103068. [Google Scholar] [CrossRef]
- Diels, C.; Bos, J.E. Great Expectations: On the Design of Predictive Motion Cues to Alleviate Carsickness. In HCI in Mobility, Transport, and Automotive Systems. HCII 2021, Proceedings of the International Conference on Human-Computer Interaction, Malaga, Spain, 22–24 September 2021; Lecture Notes in Computer Science; Krömker, H., Ed.; Springer: Cham, Switzerland, 2021; p. 12791. [Google Scholar]
- Asch, S.E.; Witkin, H.A. Studies in space orientation: I. Perception of the upright with displaced visual fields. J. Exp. Psychol. 1948, 38, 325–337. [Google Scholar] [CrossRef]
- Bos, J.E.; Nooij, S.A.E.; Souman, J.L. (Im)possibilities of studying carsickness in a driving simulator. In Proceedings of the Driving Simulator Conference Europe, Munich, Germany, 14–17 September 2021; pp. 59–63. [Google Scholar]
- Correia Gracio, B.J.; Bos, J.E.; Van Paassen, M.M.; Mulder, M. Perceptual scaling of visual and inertial cues. Effects of field of view, image size, depth cues, and degree of freedom. Exp. Brain Res. 2014, 232, 637–646. [Google Scholar] [CrossRef] [PubMed]
- Bos, J.E. Skyscraper sickness: Three reasons why tall buildings can be more sickening than ships. In Proceedings of the Motion Sickness Conference, Akureyri, Iceland, 8–10 July 2019. [Google Scholar]
- Salter, S.; Diels, C.; Herriotts, P.; Kanarachos, S.; Thake, D. Motion Sickness in Automated Vehicles with Forward and Rearward Facing Seating Orientations. Appl. Ergon. 2019, 78, 54–61. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).