A Model for Examining Challenges and Opportunities in Use of Cloud Computing for Health Information Systems
Abstract
:1. Introduction
Problem Statement and Significance
2. Overview of Health Information Systems
- Clinical information management: This relates to patient information and includes EHR, information extracted from the internal submodules, or the integration with other third-party systems. These sources can be from laboratories, radiology, inpatient, outpatient, emergency department, or pharmacies. Clinical decision support, knowledgebase, and order communication systems are also considered in this category.
- Operational management: This includes all non-clinical-related functions such as financials—billing and payroll; and human resources, which includes rosters and shift management. Operational management also includes procurement, supply chain management, maintenance, and engineering.
- Strategic decision support: This helps higher management in strategic planning and better organizational control. This may include better marketing insights, market trends, and competitor behavior.
- Electronic networking [2,16]: This includes all interfaces that involve health information movement over network. Examples are web-based telemedicine and e-health and pEHR that helps patients to have more control and empowerment over their health profiles remotely, away from the healthcare organizations’ physical location. Also, network integration with other systems and their parties can be considered in this category.
3. Cloud Computing
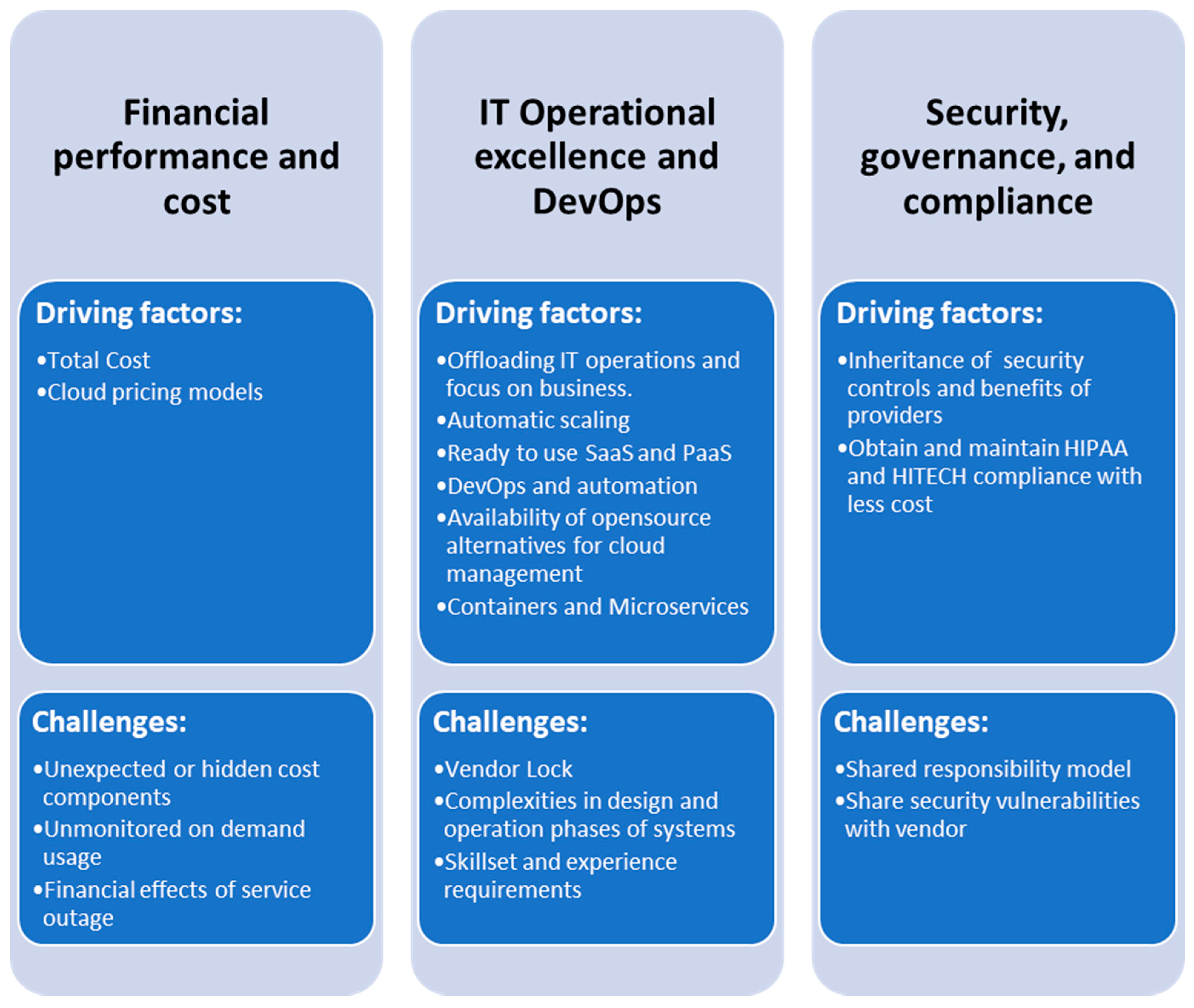
4. Drivers and Challenges for Cloud Based HIS
4.1. Financial Performance and Cost
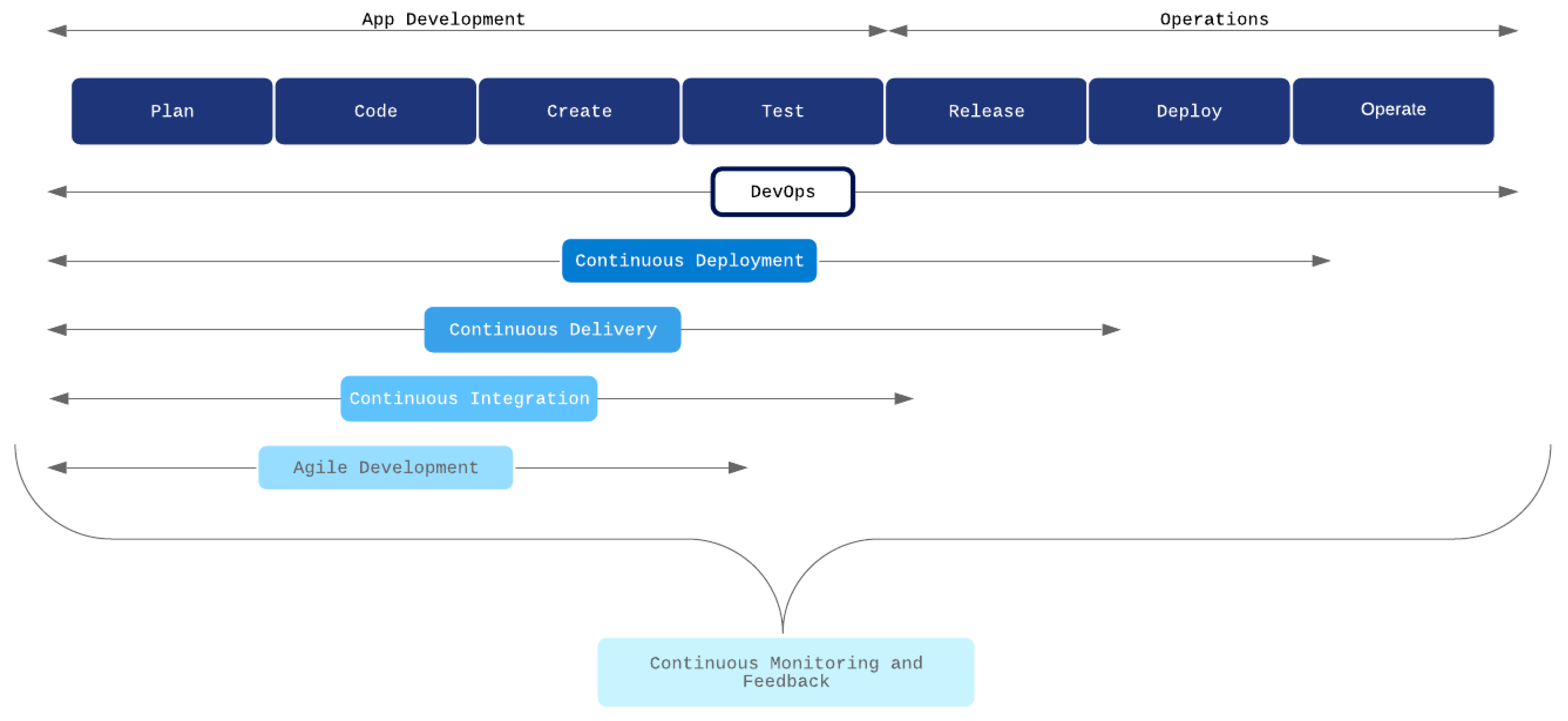
4.2. IT Operational Excellence and DevOps
4.3. Security, Governance, and Compliance
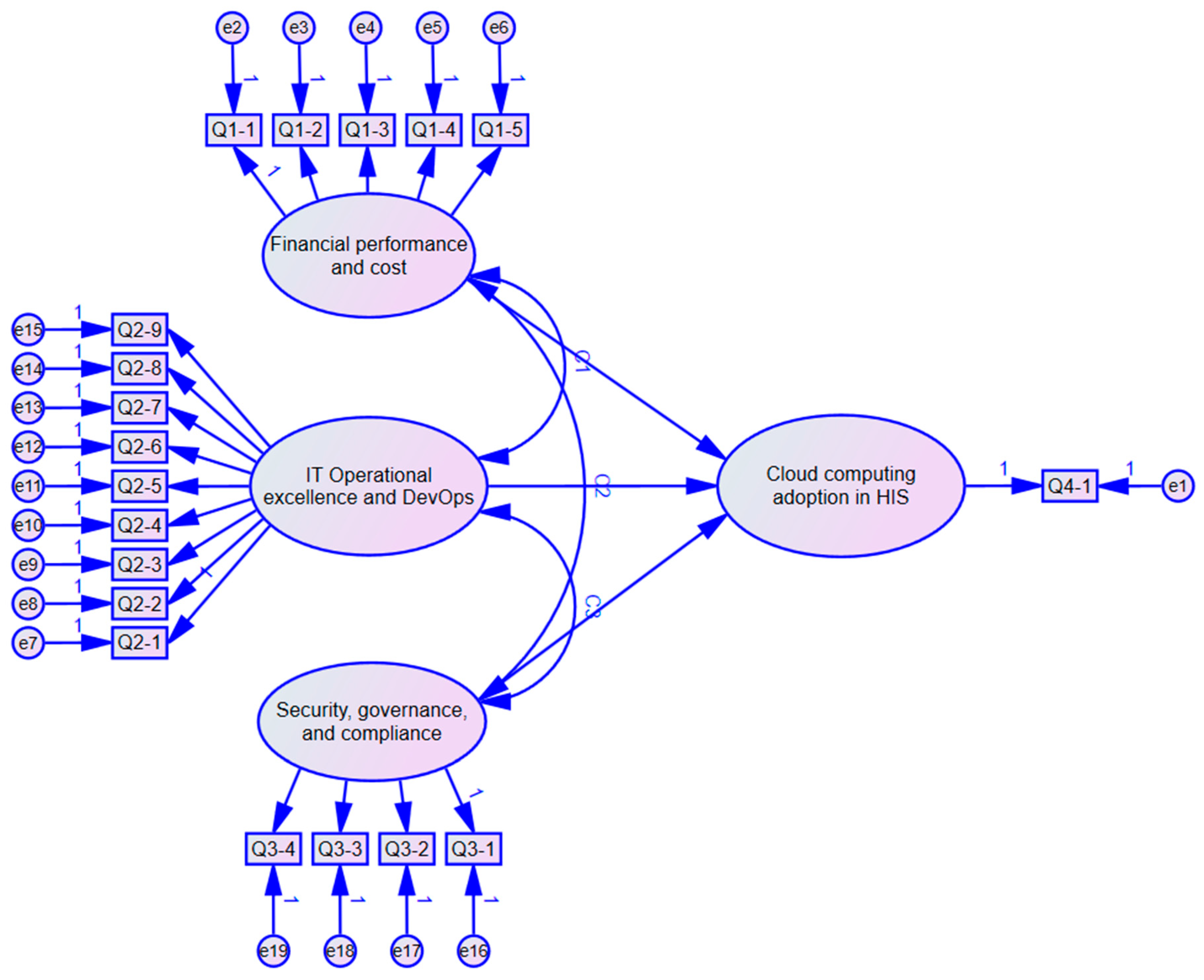
5. Research Model and Issues for Additional Research
- Q1-1: Cloud computing services reduce the total cost of operations (TCO) for IT.
- Q1-2: Cloud pricing models provide flexibility in infrastructure deployment and cost savings.
- Q1-3: There may be hidden costs of cloud computing that the organization will need to manage.
- Q1-4: Cloud computing can lead to unmonitored on-demand usage, thus increasing costs.
- Q1-5: Service outages of cloud computing providers can lead to an undesirable financial impact.
- Q2-1: Offloading IT operations and refocusing on business is a primary benefit of cloud adoption.
- Q2-2: Automatic scaling of cloud infrastructure is a priority feature for an organization’s infrastructure needs.
- Q2-3: Ready-to-use SaaS and PaaS of cloud providers is a feature that is attractive to the organization.
- Q2-4: DevOps and automation facilities of cloud providers will provide the agility needed by the organization’s HIS.
- Q2-5: Containers and microservices architecture are the current or target roadmap for architecting application in the organization.
- Q2-6: Opensource alternatives for cloud management will help the organization avoid vendor lock-in and ease migration issues.
- Q2-7: Possible vendor lock-in of a cloud provider is a source of concern.
- Q2-8: Cloud architecture complexities in design and operation phases are a source of concern.
- Q2-9: Limited availability of skilled and experienced personnel is a source of concern.
- Q3-1: Inheritance of security controls and benefits of cloud providers will alleviate security concerns in the organization.
- Q3-2: Obtaining and maintaining HIPAA and HITECH compliance can be done more cost-effectively and easily when using a cloud provider.
- Q3-3: Shared responsibility model for security is a source of concern for the organization.
- Q3-4: Shared security vulnerabilities with the cloud vendor are a source of concern for the organization.
- Q4-1: The organization is ready to adopt a cloud-enabled/native HIS.
6. Proposed Model Use for Academic Study
7. Conclusions and Future Research
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Laudon, K.C.; Laudon, J.P. Management Information Systems: Managing the Digital Firm, 16th ed.; Pearson: New York, NY, USA, 2019. [Google Scholar]
- Koutsouris, D.-D.; Lazakidou, A.A. Concepts and trends in healthcare information systems. In Annals of Information Systems; Springer International Publishing: Berlin, Germany, 2014. [Google Scholar]
- Rudd, K.; Puttkammer, N.; Antilla, J.; Richards, J.; Heffron, M.; Tolentino, H.; Jacobs, D.; KatjiuanJo, P.; Prybylski, D.; Shepard, M.; et al. Building workforce capacity for effective use of health information systems: Evaluation of a blended eLearning course in Namibia and Tanzania. Int. J. Med. Inform. 2019, 131, 103945. [Google Scholar] [CrossRef] [PubMed]
- Bonney, W. Applicability of business intelligence in electronic health record. Procedia Soc. Behav. Sci. 2013, 73, 257–262. [Google Scholar] [CrossRef] [Green Version]
- Gaardboe, R.; Nyvang, T.; Sandalgaard, N. Business intelligence success applied to healthcare information systems. Procedia Comput. Sci. 2017, 121, 483–490. [Google Scholar] [CrossRef]
- Sharda, R.; Delen, D.; Turban, E. Business Intelligence and Analytics: Systems for Decision Support, 10th ed.; Pearson: New York, NY, USA, 2015. [Google Scholar]
- Shen, C.; Chang, R.; Hsu, C.; Chang, I. How business intelligence maturity enabling hospital agility. Telemat. Inform. 2017, 34, 450–456. [Google Scholar] [CrossRef]
- Marston, S.; Li, Z.; Bandyopadhyay, S.; Zhang, J.; Ghalsasi, A. Cloud computing—The business perspective. Decis. Support Syst. 2011, 51, 176–189. [Google Scholar] [CrossRef]
- Bass, L.; Ravichandran, A.; Taylor, K.; Waterhouse, P. The software architect and DevOps. IEEE Softw. 2018, 35, 8–10. [Google Scholar] [CrossRef]
- Newman, S. Building Microservices: Designing Fine-Grained Systems; O’Reilly Media: Newton, MA, USA, 2015. [Google Scholar]
- Yusof, M.; Papazafeiropoulou, A.; Paul, R.; Stergioulas, L. Investigating evaluation frameworks for health information systems. Int. J. Med. Inform. 2008, 77, 377–385. [Google Scholar] [CrossRef]
- Sligo, J.; Gauld, R.; Roberts, V.; Villa, L. A literature review for large-scale health information system project planning, implementation and evaluation. Int. J. Med. Inform. 2017, 97, 86–97. [Google Scholar] [CrossRef] [PubMed]
- Eslami Andargoli, A.; Scheepers, H.; Rajendran, D.; Sohal, A. Health information systems evaluation frameworks: A systematic review. Int. J. Med. Inform. 2017, 97, 195–209. [Google Scholar] [CrossRef]
- Handayani, P.; Hidayanto, A.; Pinem, A.; Hapsari, I.; Sandhyaduhita, P.; Budi, I. Acceptance model of a hospital information system. Int. J. Med. Inform. 2017, 99, 11–28. [Google Scholar] [CrossRef] [PubMed]
- Glandon, G.L.; Smaltz, D.H.; Slovensky, D.J. Information systems for healthcare management. In Information Systems, 8th ed.; Health Administration Press: Chicago, IL, USA, 2013. [Google Scholar]
- Thurston, J. Meaningful use of electronic health records. J. Nurse Pract. 2014, 10, 510–513. [Google Scholar] [CrossRef]
- Nguyen, L.; Bellucci, E.; Nguyen, L. Electronic health records implementation: An evaluation of information system impact and contingency factors. Int. J. Med. Inform. 2014, 83, 779–796. [Google Scholar] [CrossRef] [PubMed]
- ISO TC 215 Health Informatics—Electronic Health Record—Definition, Scope, and Context; ISO: Geneva, Switzerland, 2005.
- Crowe, B.; Sim, L. Assessment of the effect of the ready availability of radiology results on clinical decision making at Princess Alexandra Hospital Brisbane, Australia. Int. Congr. Ser. 2004, 1268, 254–259. [Google Scholar] [CrossRef]
- Jayaratne, M.; Nallaperuma, D.; De Silva, D.; Alahakoon, D.; Devitt, B.; Webster, K.; Chilamkurti, N. A data integration platform for patient-centered e-healthcare and clinical decision support. Future Gener. Comput. Syst. 2019, 92, 996–1008. [Google Scholar] [CrossRef]
- Okazaki, E.; Yao, R.; Sirven, J.; Crepeau, A.; Noe, K.; Drazkowski, J.; Hoerth, M.; Salinas, E.; Csernak, L.; Mehta, N. Usage of EpiFinder clinical decision support in the assessment of epilepsy. Epilepsy Behav. 2018, 82, 140–143. [Google Scholar] [CrossRef] [PubMed]
- Plebani, M.; Aita, A.; Padoan, A.; Sciacovelli, L. Decision support and patient safety. Clin. Lab. Med. 2019, 39, 231–244. [Google Scholar] [CrossRef] [PubMed]
- Hassol, A.; Deitz, D.; Goldberg, H.; Honicker, M.; Younkin, J.; Chaundy, K.; Walker, J.M.; Cummins, M.R. Health information exchange. CIN Comput. Inform. Nurs. 2016, 34, 145–150. [Google Scholar] [CrossRef]
- Benson, T.; Grieve, G. Why interoperability is hard. In Principles of Health Interoperability; Health Information Technology Standards; Springer: Cham, Switzerland, 2021. [Google Scholar] [CrossRef]
- Everson, J.; Patel, V.; Adler-Milstein, J. Information blocking remains prevalent at the start of 21st century cures act: Results from a survey of health information exchange organizations. J. Am. Med. Inform. Assoc. 2021, ocaa323. [Google Scholar] [CrossRef]
- Vest, J.R.; Gamm, L.D. Health information exchange: Persistent challenges and new strategies. J. Am. Med Inform. Assoc. 2010, 17, 288–294. [Google Scholar] [CrossRef] [Green Version]
- Alsulame, K.; Khalifa, M.; Househ, M. E-Health status in Saudi Arabia: A review of current literature. Health Policy Technol. 2016, 5, 204–210. [Google Scholar] [CrossRef]
- Sultan, N. Making use of cloud computing for healthcare provision: Opportunities and challenges. Int. J. Inf. Manag. 2014, 34, 177–184. [Google Scholar] [CrossRef]
- Kros, J.; Kirchoff, J.; Falasca, M. The impact of buyer-supplier relationship quality and information management on industrial vending machine benefits in the healthcare industry. J. Purch. Supply Manag. 2019, 25, 100506. [Google Scholar] [CrossRef]
- Kwon, I.; Kim, S.; Martin, D. Healthcare supply chain management; strategic areas for quality and financial improvement. Technol. Forecast. Soc. Chang. 2016, 113, 422–428. [Google Scholar] [CrossRef]
- Branco, T.; de Sá-Soares, F.; Rivero, A. Key issues for the successful adoption of cloud computing. Procedia Comput. Sci. 2017, 121, 115–122. [Google Scholar] [CrossRef]
- Senyo, P.; Addae, E.; Boateng, R. Cloud computing research: A review of research themes, frameworks, methods and future research directions. Int. J. Inf. Manag. 2018, 38, 128–139. [Google Scholar] [CrossRef] [Green Version]
- Alharbi, F.; Atkins, A.; Stanier, C.; Al-Buti, H. Strategic value of cloud computing in healthcare organisations using the balanced scorecard approach: A case study from a Saudi hospital. Procedia Comput. Sci. 2016, 98, 332–339. [Google Scholar] [CrossRef] [Green Version]
- Ali, O.; Shrestha, A.; Soar, J.; Wamba, S. Cloud computing-enabled healthcare opportunities, issues, and applications: A systematic review. Int. J. Inf. Manag. 2018, 43, 146–158. [Google Scholar] [CrossRef]
- Meri, A.; Hasan, M.; Danaee, M.; Jaber, M.; Jarrar, M.; Safei, N.; Dauwed, M.; Abd, S.; Al-bsheish, M. Modelling the utilization of cloud health information systems in the Iraqi public healthcare sector. Telemat. Inform. 2019, 36, 132–146. [Google Scholar] [CrossRef]
- Daim, T.U.; Behkami, N.; Basoglu, N.; Kök, O.M.; Hogaboam, L. Healthcare Technology Innovation Adoption; Springer International Publishing: Berlin, Germany, 2016. [Google Scholar] [CrossRef]
- Miniati, R.; Iadanza, E.; Dori, F. Clinical Engineering: From Devices to Systems; Elsevier Inc.: Amsterdam, The Netherlands, 2015. [Google Scholar]
- Kratzke, N.; Quint, P. Understanding cloud-native applications after 10 years of cloud computing–A systematic mapping study. J. Syst. Softw. 2017, 126, 1–16. [Google Scholar] [CrossRef]
- Baldominos Gomez, A.; Rada, F.; Saez, Y. DataCare: Big data analytics solution for intelligent healthcare management. Int. J. Interact. Multimed. Artif. Intell. 2018, 4, 13. [Google Scholar] [CrossRef] [Green Version]
- Karaca, Y.; Moonis, M.; Zhang, Y.; Gezgez, C. Mobile cloud computing based stroke healthcare system. Int. J. Inf. Manag. 2019, 45, 250–261. [Google Scholar] [CrossRef]
- Carvalho, J.; Rocha, Á.; van de Wetering, R.; Abreu, A. A maturity model for hospital information systems. J. Bus. Res. 2019, 94, 388–399. [Google Scholar] [CrossRef]
- Gellweiler, C. Operational excellence as the main customer value: Information technology vendors’ perspective. Bus. Syst. Res. J. 2019, 10, 13–30. [Google Scholar] [CrossRef] [Green Version]
- AbuKhousa, E.; Mohamed, N.; Al-Jaroodi, J. E-health cloud: Opportunities and challenges. Future Internet 2012, 4, 621–645. [Google Scholar] [CrossRef] [Green Version]
- Makhlouf, R. Cloudy transaction costs: A dive into cloud computing economics. J. Cloud Comput. 2020, 9, 1. [Google Scholar] [CrossRef] [Green Version]
- Amazon AWS. Linux Virtual Machines Pricing. Available online: https://aws.amazon.com/ec2/pricing/ (accessed on 16 December 2020).
- Microsoft Azure. Amazon EC2 Pricing. Available online: https://azure.microsoft.com/en-us/pricing/details/virtual-machines/linux/ (accessed on 16 December 2020).
- Kim, W.; Kim, S.D.; Lee, E.; Lee, S. Adoption issues for cloud computing. In Proceedings of the 7th International Conference on Advances in Mobile Computing and Multimedia, Kuala Lumpur, Malaysia, 14–16 December 2009; pp. 2–5. [Google Scholar]
- Shatil, A.S.; Younas, S.; Pourreza, H.; Figley, C.R. Heads in the cloud: A primer on neuroimaging applications of high performance computing. Magn. Reson. Insights 2016, 8, 69–80. [Google Scholar] [CrossRef] [Green Version]
- Toffetti, G.; Brunner, S.; Blöchlinger, M.; Spillner, J.; Bohnert, T. Self-managing cloud-native applications: Design, implementation, and experience. Future Gener. Comput. Syst. 2017, 72, 165–179. [Google Scholar] [CrossRef] [Green Version]
- Shadija, D.; Rezai, M.; Hill, R. Microservices: Granularity vs. Performance. In Companion Proceedings of the 10th International Conference on Utility and Cloud Computing (UCC ‘17 Companion), New York, NY, USA, 5–8 December 2017; pp. 215–220. [Google Scholar] [CrossRef]
- Gupta, V.; Kapur, P.; Kumar, D. Modeling and measuring attributes influencing DevOps implementation in an enterprise using structural equation modeling. Inf. Softw. Technol. 2017, 92, 75–91. [Google Scholar] [CrossRef]
- Di Francesco, P.; Lago, P.; Malavolta, I. Architecting with microservices: A systematic mapping study. J. Syst. Softw. 2019, 150, 77–97. [Google Scholar] [CrossRef] [Green Version]
- Hunter, T., II. Advanced Microservices. In Advanced Microservices; Apress: Berkeley, CA, USA, 2017. [Google Scholar] [CrossRef]
- Balajee, N. How Does DevOps Process Flow? Medium.Com. Available online: https://medium.com/devopsnews/how-does-devops-process-flow-f1d56e93408c (accessed on 16 January 2020).
- Hasselbring, W. Microservices for scalability. In Proceedings of the 7th ACM/SPEC on International Conference on Performance Engineering (ICPE ’16), Delft, The Netherlands, 12–16 March 2016; Association for Computing Machinery: New York, NY, USA, 2016; pp. 133–134. [Google Scholar] [CrossRef]
- Vicert. Microservices in Healthcare: Granulate to Accelerate. Available online: https://vicert.com/local/resources/assets/pdf/WhitePaper_MicroservicesinHealthcare.pdf (accessed on 16 January 2021).
- Balis, U.; Williams, C.; Sica, J.; Killen, R. The growing need for microservices in bioinformatics. J. Pathol. Inform. 2016, 7, 45. [Google Scholar] [CrossRef]
- Khaloufi, H.; Abouelmehdi, K.; Beni-hssane, A.; Saadi, M. Security model for big healthcare data lifecycle. Procedia Comput. Sci. 2018, 141, 294–301. [Google Scholar] [CrossRef]
- Ghazvini, A.; Shukur, Z. Security challenges and success factors of electronic healthcare system. Procedia Technol. 2013, 11, 212–219. [Google Scholar] [CrossRef] [Green Version]
- Khalifa, M. Barriers to health information systems and electronic medical records implementation. A field study of Saudi Arabian hospitals. Procedia Comput. Sci. 2013, 21, 335–342. [Google Scholar] [CrossRef] [Green Version]
- AWS. Architecting for HIPAA Security and Compliance on Amazon Web Services Amazon Web Services. May 2020. Available online: https://aws.amazon.com/compliance/hipaa-compliance/ (accessed on 16 July 2020).
- Varghese, B.; Buyya, R. Next generation cloud computing: New trends and research directions. Future Gener. Comput. Syst. 2018, 79, 849–861. [Google Scholar] [CrossRef] [Green Version]
- Fatima, A.; Colomo-Palacios, R. Security aspects in healthcare information systems: A systematic mapping. Procedia Comput. Sci. 2018, 138, 12–19. [Google Scholar] [CrossRef]
- Zheng, W.; Wu, Y.; Chen, L. Business intelligence for patient-centeredness: A systematic review. Telemat. Inform. 2018, 35, 665–676. [Google Scholar] [CrossRef]
- Bouayad, A.; Blilat, A.; Mejhed, N.E.H.; El Ghazi, M. Cloud computing: Security challenges. In Proceedings of the 2012 Colloquium in Information Science and Technology, Fez, Morocco, 22–24 October 2012; pp. 26–31. [Google Scholar] [CrossRef]
- Kumar, P.; Raj, P.; Jelciana, P. Exploring data security issues and solutions in cloud computing. Procedia Comput. Sci. 2018, 125, 691–697. [Google Scholar] [CrossRef]
- Marakhimov, A.; Joo, J. Consumer adaptation and infusion of wearable devices for healthcare. Comput. Hum. Behav. 2017, 76, 135–148. [Google Scholar] [CrossRef]
- Hussien, H.M.; Yasin, S.M.; Udzir, S.N.I.; Zaidan, A.A.; Zaidan, B.B. A systematic review for enabling of develop a blockchain technology in healthcare application: Taxonomy, substantially analysis, motivations, challenges, recommendations and future direction. J. Med. Syst. 2019, 43, 1–35. [Google Scholar] [CrossRef]
- Zhang, L.; Taotao, W.; Soung, C.L. Speeding up block propagation in blockchain network: Uncoded and coded designs. arXiv 2021, arXiv:2101.00378. [Google Scholar]
- Pawar, M.K.; Patil, P.; Hiremath, P.S. A Study on Blockchain Scalability. In Advances in Intelligent Systems and Computing; Tuba, M., Akashe, S., Joshi, A., Eds.; ICT Systems and Sustainability; Springer: Singapore, 2021; Volume 1270. [Google Scholar] [CrossRef]
- Dabbagh, M.; Choo, K.K.R.; Beheshti, A.; Tahir, M.; Safa, N.S. A survey of empirical performance evaluation of permissioned blockchain platforms: Challenges and opportunities. Comput. Secur. 2021, 100, 102078. [Google Scholar] [CrossRef]
- Wang, H.; Song, Y. Secure cloud-based EHR system using attribute-based cryptosystem and blockchain. J. Med. Syst. 2018, 42, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Jiang, S.; Cao, J.; Wu, H.; Yang, Y.; Ma, M.; He, J. Blochie: A blockchain-based platform for healthcare information exchange. In Proceedings of the 2018 IEEE international conference on smart computing (smartcomp), Taormina, Sicily, Italy, 18–20 June 2018; pp. 49–56. [Google Scholar]
- Hilty, D.M.; Armstrong, C.M.; Edwards-Stewart, A.; Gentry, M.T.; Luxton, D.D.; Krupinski, E.A. Sensor, wearable, and remote patient monitoring competencies for clinical care and training: Scoping review. J. Technol. Behav. Sci. 2021, 6, 1–26. [Google Scholar] [CrossRef]
- Alamri, A. Ontology middleware for integration of IoT healthcare information systems in EHR systems. Computers 2018, 7, 51. [Google Scholar] [CrossRef] [Green Version]
- Angelo, R. The internet of things (IoT), electronic health record (EHR), and federal legislation: The case for a national electronic personal health information (EPHI) record system. Issues Inf. Syst. 2020, 21, 279–288. [Google Scholar]
| Company | Nature of Responsibility of the Interviewee | Industry | Product/Services of the Company |
|---|---|---|---|
| 1 | Chief Internal Auditor | Investment | Palestinian investment firm that invested in many local hospitals. |
| 2 | Consultant | Financial and security Auditing | One of the Big four accounting firms that participated in external auditing of private hospitals. |
| 3 | Chief Product Officer (CPO) | SaaS, Hospitality | Hospitality SaaS Cloud hosted provider |
| 4 | Chief Nursing Officer (CNO) | Healthcare | Privately held hospital with locally hosted HIS |
| 5 | CEO | Healthcare | Privately held hospital with locally hosted HIS |
| 6 | Advisory and board member | SaaS, Healthcare | Hybrid cloud SaaS provider for HIS complementary functions |
| 7 | Director of design and architecture | SaaS, Hospitality | Hospitality SaaS Cloud hosted provider |
| 8 | VP of Engineering | SaaS, Healthcare | Hybrid cloud SaaS provider for HIS complementary functions |
| 9 | CTO | IT solutions | Outsourcing company with multiple, on-premises and cloud hosted solutions. |
| 10 | CTO | Security | IT Security firm with clients in healthcare field |
| 11 | Chief Financial Officer (CFO) | Healthcare | Privately held hospital with hybrid cloud HIS |
| 12 | IT Manager | Healthcare | Public hospital with on-premises HIS |
| 13 | Technology Evangelist | IT solutions | A well-known open-source IT solutions company helping many clients in many sectors to adapt cloud computing. |
| 14 | QA Manager | Healthcare | Public hospital with on-premises HIS |
| 15 | CIO | Healthcare | Privately held regional system in US transitioning to Cerner hosted HIS |
| 16 | Chief Medical Officer (CMO) | Healthcare | Large specialty hospital in India without an EHR and separate laboratory systems |
| Financial performance and cost | Assessment of the benefits of using reservation and excess capacity usage pricing schemes over on-demand pricing. Measurement of customer satisfaction on cost and billing of cloud providers. Establishment of models to estimate savings due to the use of cloud providers over the conventional datacenters. |
| IT Operational excellence and DevOps | Quantitative measurement of the performance gains resulting from using cloud infrastructure in comparison to traditional and on-premises data center. Measurement of benefits of hardware generation upgrades. Longitudinal studies comparing scaling provided by well forecasted on-premises hardware to cloud-provided auto scaling features through the use of financial metrics. Measurement of the satisfaction of healthcare institutions of service availability and support of different cloud vendors. Establishment of a framework for HIS implementation using DevOps and microservices with empirical focus on measuring software lifecycle KPIs like delivery time, requirement satisfaction, performance, availability, and scalability, and comparing them to traditional implementations. |
| Security, governance, and compliance | Qualitative research to infer the factors for adapting cloud SaaS and PaaS solutions or opensource solutions in the healthcare context along with associated security risks. Design and implementation of a framework for HIS implementation that complies with international standards with responsibilities definitions. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Marsy, A.; Chaudhary, P.; Rodger, J.A. A Model for Examining Challenges and Opportunities in Use of Cloud Computing for Health Information Systems. Appl. Syst. Innov. 2021, 4, 15. https://doi.org/10.3390/asi4010015
Al-Marsy A, Chaudhary P, Rodger JA. A Model for Examining Challenges and Opportunities in Use of Cloud Computing for Health Information Systems. Applied System Innovation. 2021; 4(1):15. https://doi.org/10.3390/asi4010015
Chicago/Turabian StyleAl-Marsy, Ahmad, Pankaj Chaudhary, and James Allen Rodger. 2021. "A Model for Examining Challenges and Opportunities in Use of Cloud Computing for Health Information Systems" Applied System Innovation 4, no. 1: 15. https://doi.org/10.3390/asi4010015
APA StyleAl-Marsy, A., Chaudhary, P., & Rodger, J. A. (2021). A Model for Examining Challenges and Opportunities in Use of Cloud Computing for Health Information Systems. Applied System Innovation, 4(1), 15. https://doi.org/10.3390/asi4010015







