Abstract
Objective: Transperineal prostate (TP) biopsy is the key diagnostic tool for evaluating prostate cancer and is feasible under local anaesthetic (LA) alone. However, concerns about its tolerability encourage use of a multimodal analgesia approach. Pre-emptive over-the-counter analgesia with LA may provide a simple and low-risk option. The objective of this study was to investigate the effects of over-the-counter analgesia on TP biopsies conducted under LA. Methods: This interventional single-centre study investigated 160 participants who undertook a TP biopsy under LA, with and without pre-emptive analgesia (1 g of paracetamol and 400 mg of ibuprofen). Pain tolerability was measured using a visual analogue scale (VAS) at three procedural points (probe insertion, LA infiltration, and biopsy); an overall average VAS score was subsequently calculated. The abstracted secondary variables include patient details (age, prostate size, and PSA level), biopsy details (number of cores and volume of LA used), and preferability for LA use in future TP biopsies. An inferential statistical analysis was performed using Wilcoxon’s Rank Sum non-parametric test, Pearson’s test of correlation, and Pearson’s Chi-squared test. Results: The groups were comparable in age, prostate size, and PSA level. Median VAS scores were consistently lower in the intervention cohort, but without statistical significance. A higher volume of LA was associated with lower overall VAS (p = 0.03). LA was strongly preferred over GA for hypothetical future TP biopsies in both cohorts. Conclusions: Pre-emptive analgesia does not significantly improve tolerability of TP biopsy under LA. Our study substantiates evidence that TP biopsy is generally well tolerated under LA and preferred over GA.
1. Introduction
Australia has one of the highest rates of prostate cancer, and it has remained a leading cause of death from cancer since 2001 [1,2]. Early detection and diagnosis of prostate cancer are important aspects to its timely treatment and contribute to a decrease in prostate cancer-related mortality [3]. Targeted prostate biopsy is crucial in the diagnostic pathway for prostate cancer, with transperineal (TP) prostate biopsy superseding the transrectal (TR) approach as the gold standard diagnostic tool for prostate cancer in Australia [4]. Compared to the TR approach, TP biopsy shows significantly lower rates of infectious complications and does not compromise on diagnostic ability [5,6,7].
Nevertheless, there are logistical concerns with implementing the TP approach and the pain it may elicit, compared to TR biopsy, which can be well tolerated as an ambulatory procedure [8]. Traditionally, TP biopsy is performed under general anaesthetic (GA) with systematic sampling of the prostate gland; however, the development of freehand techniques and increased sensitivity of imaging scans, including multiparametric magnetic resonance imaging (mpMRI), have enabled a targeted approach which reduces the numbers of cores necessary for diagnosis and therefore limits the patient’s experience of pain [8]. Numerous studies have explored pain scores of TP biopsy under local anaesthetic (LA) using a freehand technique and report it as a generally well-tolerated procedure [9,10,11,12,13]. Pain tolerability has been quantified in these studies using standard numerical rating scales, with the visual analogue scale (VAS) gaining popularity in its ability to capture fine-grained measurements [1]. In addition, approximately 95% of patients who underwent a TP biopsy were able to complete the procedure [14], and the literature reports 85% to 94% of patients would elect to undertake a TP biopsy under LA again if required [10,15].
While TP biopsy under LA is shown to be both feasible and largely tolerable, pain is still a concern among patients and doctors alike. Multimodal analgesia with over the counter (OTC) analgesics has been previously shown to provide effective pain relief in the post-operative setting [16,17], and non-steroidal anti-inflammatory drugs have been used as pre-emptive analgesia in other outpatient procedures to good effect [18]. As such, OTC analgesics have potential as a low-risk and easily available option for further improving TP biopsy tolerability.
The purpose of this study was to investigate whether pre-emptive OTC analgesia adds value as a pain management tool for TP biopsy under LA.
2. Materials and Method
2.1. Study Design and Setting
This study was initially designed as an audit activity following the Royal Australasian College of Surgeons’ Surgical Audit Guide [19], as depicted in Figure 1. Pain scores for targeted TP biopsies using LA were measured, and our practice was changed to include pre-emptive analgesia. This interventional study reviewed male patients who undertook a TP prostate biopsy under LA and compared them as a control group to a new cohort of patients who underwent the same procedure with the addition of pre-emptive analgesia (1 g of paracetamol and 400 mg of ibuprofen), taken 1 h prior to the biopsy. The procedures were performed at the Sydney Adventist Hospital from August 2021 to March 2023. Data were first collected for the control cohort, followed by the intervention group.
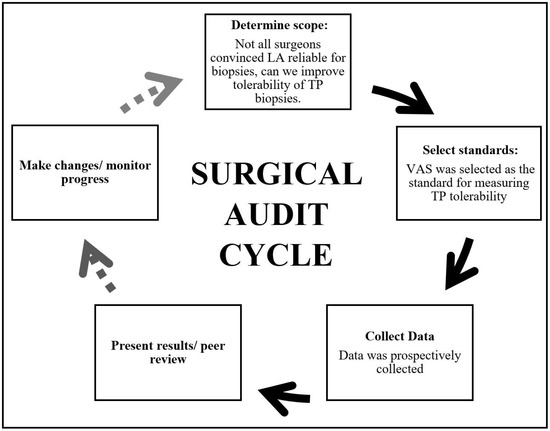
Figure 1.
The Surgical Audit Cycle of this project was designed with reference to the Royal Australasian College of Surgeons’ Surgical Audit Guide [20]. Solid lines indicate what was achieved in this project, while dotted lines represent possible future directions.
2.2. Participants
The inclusion criteria were males requiring targeted prostate biopsy in conjunction with an abnormal mpMRI. There were two patient cohorts: the control and the intervention group. There were 113 patients in the control cohort (mean age = 67 years, SD = 8.3, median = 67, and IQR = 11) and 47 patients in the intervention group (mean age = 67 years, SD = 7.8, median = 66, and IQR = 9.5). Patients were excluded from the project if they were unable to tolerate the procedure; these patients received a TP biopsy under sedation instead (Figure 2).
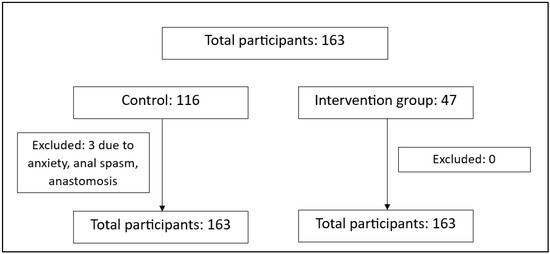
Figure 2.
Details of participants included at each stage of the study. Reasons for excluding participants are described.
2.3. Methodology
All patients underwent a TP prostate biopsy using an ultrasound guide (Canon Aplio i600, Canon Medical Systems Corporation, Sydney, Australia) with a purpose-specific perineal biopsy guide. Patients were placed in a lithotomy position, and the scrotum was displaced superiorly with adhesive tape to provide access to the perineum. A digital rectal examination was performed immediately prior to the application of Betadine (Povidone-iodine) to the perineum, and a lubricated ultrasound probe was inserted transrectally. Local anaesthetic, 1% lignocaine with 0.0005% adrenaline (Aspen Pharmacare Australia Pty Ltd., Sydney, Australia), was infiltrated initially into the perineal skin as well as structures of the pelvic floor under ultrasound guidance using a spinal analgesic needle (Uniever, Unisis Corporation Japan, Tokyo, Japan). The surgeon used his discretion to determine the amount of LA to achieve adequate anaesthesia. Multiple core biopsies were taken using a Tru Core 11 Automatic biopsy instrument 18 G × 20 cm (Argon Medical Devices, Plano, TX, USA). Our practice was to take four cores from each abnormal Prostate Imaging-Reporting and Data System lesion as determined by mpMRI.
2.4. Outcome Assessments
The primary outcome was pain tolerability as evaluated using a 10 cm visual analogue scale (VAS) at three procedural points: probe insertion, LA infiltration, and biopsy. Zero and ten centimetres represented no pain and pain as bad as it could possibly be, respectively (see Appendix A). Following the procedure, patients were asked to mark their pain score on the VAS. The distance between zero and the mark made by the patient was recorded in centimetres (cm) for data analysis. The average of the three VAS scores were calculated to determine an overall VAS score.
Secondary variables included patient factors (age, prostate size, and PSA level), biopsy factors (number of biopsy cores taken and volume of LA used), and patient preference for LA with subsequent TP biopsies.
2.5. Statistical Analysis
The absence of previous data on pre-emptive analgesia in the TP biopsy setting did not allow for a power calculation to be performed. Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS), version 28.0.1.0 (SPSS Inc., IBM Corp., Armonk, NY, USA). The central tendency (mean ± standard deviation and the median with the interquartile range (IQR)) of these variables were also determined. The Wilcoxon Rank Sum test was used to compare characteristics and demographics between the control and intervention groups. Pearson’s test of correlation was used to compare quantitative variables within either group. Participants’ choice of LA versus GA for future TP biopsy was calculated as a percentage. Pearson’s Chi-squared test was used to test the significance between LA versus GA preference in the two groups. Statistical significance was defined at a p-value < 0.05.
2.6. Ethics
Ethics approval was obtained by the Adventist HealthCare Limited as a Quality Improvement project with the ethics number (2021-11-15). Patient data were de-identified and collected onto a password-protected and anonymised spreadsheet that was accessed exclusively by the research team.
3. Results
3.1. Group Comparability and Demographics
Participants in the control and intervention groups were directly comparable (see Table 1). It was noted that there were two outliers in the intervention group at 597 ng/mL and 239 ng/mL, which resulted in a spuriously high mean. Upon excluding the aforementioned PSA outliers, the mean (±SD) changed from 26.3 (±91.8) to 8.8 (±7.9).

Table 1.
Mean ± standard deviation, median with IQR, and the p-value of the age, prostate size, and PSA levels in the control and intervention group subjects. Wilcoxon Rank Sum test was used to find significance. Significance was taken as p < 0.05.
3.2. VAS Comparison
There was an overall decrease in VAS scores observed in the intervention group, with the exception of VAS-LA infiltration. However, these variations were not statistically significant (see Table 2). In both groups, LA infiltration recorded the highest VAS scores. The lowest VAS scores were recorded during the passage of the biopsy needle.

Table 2.
Mean ± SD, median and IQR, and the p-value of the VAS at probe insertion, LA infiltration, biopsy, and the overall VAS in the control and intervention group subjects. Wilcoxon Rank Sum test was used to find significance. Significance was taken as p < 0.05.
3.3. Correlation Analysis
Univariate analyses with the selected variables were analysed with each VAS subgroup (Table 3).

Table 3.
Pearson correlation, p-value, and 95% confidence intervals of four VAS scores: the overall VAS, VAS at probe insertion, VAS at LA infiltration, and VAS of the biopsy. The age, prostate size, PSA level, number of cores, and volume of LA were compared between the control and intervention group for each VAS measurement. Pearson’s test of correlation was used to find significance. Significance was taken as p < 0.05, and results that were significant are highlighted.
There were various negative correlations found to be statistically significant. In the intervention group, the observed negative correlations were VAS-Overall and volume of LA; VAS-Probe insertion and prostate size; and VAS-LA infiltration and volume of LA. In the control group, there was one observed negative correlation between VAS-LA infiltration and age. These are further summarised in Table A1 and Figure A1, Figure A2, Figure A3 and Figure A4.
3.4. Choice for Next Procedure
The relationship between our control and intervention group was not statistically significant in their preference between LA and GA (see Table 4).

Table 4.
Participants’ choice of general anaesthetic versus local anaesthetic for future TP biopsy in the control and intervention groups. Pearson’s Chi-squared test was used to find significance. Significance was taken as p < 0.05.
4. Discussion
Our study found that the majority of the mean and median VAS scores in the intervention group decreased compared to the control group; however, this small difference failed to meet statistical significance.
An alternate method of analysis is by examining the minimal clinically important difference (MCID). The MCID reflects the minimum amount of reduction in VAS score required to produce any clinical pain improvement regardless of the statistical significance. Upon analysis of the current literature surrounding urological procedures, the MCID for TP biopsy has not yet been determined. In other publications, the MCID has fluctuated depending on setting and procedure. In the emergency department, it was found to be 0.9 cm [21], whilst surgical studies demonstrate a range between 1.8 cm to 5.2 cm post hallux valgus surgery [22], and 2.46 cm for patellofemoral inlay arthroplasty [23]. This high variability and specificity of MCID between different settings and operative procedures hindered the direct comparison of our findings to MCID from non-TP biopsy related literature. Additional research to determine the specific MCID for TP biopsy could provide more meaning and context to our study.
The VAS scores in this study are largely comparable to those in the literature in both their raw values and trends. Our findings showed a median VAS-Overall of 2.4 and 2.0 for the control and intervention groups, respectively. Similar studies exploring the tolerability of TP biopsy under LA using VAS scores report a wide range of median VAS-Overall between 1.0 and 4.5 [9,24]. Interestingly, this variability is maintained even when the overall VAS is further divided into the three procedural points: probe insertion, LA infiltration, and biopsy. The literature reports a median VAS for each of the aforementioned points in the ranges 1.1–6.0, 2.0–5.0, and 2.0–4.5, respectively [7,10,13,24]. In comparison, the median VAS scores in our study were in the ranges 1.5–1.7, 2.7–3.0, and 1.4–1.7 respectively, with the intervention group obtaining the lowest score at all three points. VAS-LA infiltration was consistently the most painful part of the procedure for both the control and intervention groups, with this pattern affirmed by other studies as well [9,10,13,24]. As such, our findings for VAS-Probe insertion are consistent with those in the literature [10,13,24], but our patient population appears to experience decreased pain at LA infiltration and biopsy compared to similar studies [10,24]. Given there is variation in study technique within the literature, such as the number of biopsy cores taken, volume of LA used, and procedural time, these factors may be responsible for the wide range of VAS scores and the discrepancy between our results and the pre-existing literature.
There were observed correlations in the data analysis between pain scores and volume of LA. Higher volume of LA was correlated with lower pain scores in the intervention cohort, and this was a consistent finding in VAS-Overall (Pearson correlation −0.32, p = 0.03), as well as in VAS-LA infiltration (Pearson correlation −0.36, p = 0.02). However, these are weak correlations, and suspiciously, the same result was not observed at the subsequent procedural point of biopsy, where LA would take effect to reduce pain. Nevertheless, other studies support findings where a higher volume of LA correlates with lower overall pain scores. A randomised controlled trial reported an inverse relationship between volume of LA and pain, particularly with LA administered at the apical region [20]. Similarly, a non-systematic literature review on analgesia forms for TP biopsy indicates some evidence linking higher volumes of LA with lower VAS-Overall scores, and higher VAS-LA infiltration scores [25]. This relationship is not clearly defined, however, as none of the studies in the non-systematic literature review measures a direct relationship between the volume of LA used and VAS at LA infiltration. Regardless, this corroborates the evidence above that LA infiltration is the most painful part of the procedure and suggests that an increased volume of LA at this point of the procedure may improve its overall tolerability.
This study also found a weak correlation between reduced pain during probe insertion and larger prostate size in the intervention group (Pearson correlation −0.33, p = 0.03). Interestingly, we did not observe an association between decreased pain scores and prostate size in any other part of the procedure. In addition, our data did not find a significant difference in prostate size (p = 0.35) or VAS-Probe insertion (p = 0.17) between our control and intervention groups. Thus, the weak significance displayed in these data is unlikely to be clinically significant. This is consistent with previous studies showing prostate size is not correlated with pain during transrectal ultrasound [26,27].
In addition, this study observed a higher age group was linked with lower pain scores during LA infiltration in the control group (Pearson correlation −0.22, p = 0.02). This relationship between age and pain is controversial and supported by some studies [28,29], while rejected by others [30]. In our study, the association between age and pain was an isolated finding (i.e., age does not appear to have a negative correlation with any other VAS procedural points, and it is only within the control population). It is therefore difficult to conclude an association between older age and greater pain tolerance.
Other than pain scores, tolerability was measured by documenting patient preference for anaesthetic agent in hypothetical future TP biopsies. There was a strong preference for LA use in both groups, with 92% of the control cohort and 96% of the intervention group preferring LA over GA for future TP biopsy, but this was not statistically significant (p = 0.40). This range is consistent with the literature, which noted that 85–96% of patients would prefer LA compared to GA [10,12]. While the increased percentage of patients preferring LA over GA in our intervention group is promising, the benefit of OTC analgesia remains unclear. Larger-scale studies would be needed to support this finding.
In summary, this study identified multiple statistically significant negative correlations between a number of variables and VAS scores. While the role of OTC analgesia could not be conclusively applied to clinical practice, our results reinforce the complexity of variables affecting TP biopsy tolerability.
Strengths and Limitations
Our study is one of the few which investigates which patient and biopsy factors may contribute to pain scores in TP biopsy under LA.
This study is both strengthened and limited by it being a single-centre study. Compared to multi-centre studies, there is greater consistency in the treatment and care our patients received. However, as a single-centre study, the extent to which our results can be generalised to other centres is unknown.
A limitation is that this study may be underpowered to demonstrate any difference. Moreover, this study did not review the regular medications of individual participants, specifically those for analgesia, which may have been taken in adjunct and impact their pain levels.
5. Conclusions
Our project sought to further improve the tolerability of TP biopsy under LA, and while pre-emptive OTC analgesia was not shown to have a clinically significant effect, our analysis substantiates existing evidence that TP biopsy is indeed well tolerated under LA, even without pre-emptive analgesia.
Author Contributions
Conceptualization, H.H.W.; methodology, H.H.W.; formal analysis, H.H.W.; investigation, S.T.-L.W., Y.X., M.J.C., A.J. and H.H.W.; resources, H.H.W.; data curation, S.T.-L.W. and H.H.W.; writing—original draft preparation, S.T.-L.W.; writing—review and editing, S.T.-L.W., Y.X., M.J.C., A.J. and H.H.W.; supervision, H.H.W.; project administration, H.H.W.; funding acquisition, H.H.W. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Human Research Ethics Committee of Adventist Healthcare Limited (protocol code 2021-11-15 and date of approval 15 November 2021).
Informed Consent Statement
Patient consent was waived due to this being an approved quality improvement project.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors on request.
Conflicts of Interest
The authors report no conflicts of interest.
Abbreviations
| GA | general anaesthetic |
| LA | local anaesthetic |
| MCID | minimally clinically important difference |
| mpMRI | multiparametric magnetic resonance imaging |
| OTC | over the counter |
| PSA | prostate-specific antigen |
| TP | transperineal |
| TR | transrectal |
| VAS | visual analogue scale |
Appendix A
Patient Name (First, Last): _________________________________________
MRN: ___________________________________________________________
Date of biopsy: ___________________________________________________
- Please mark on the line below your worst level of pain during PROBE INSERTION:
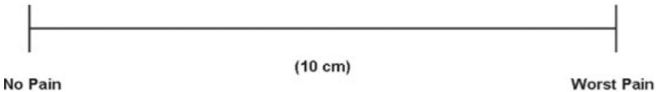
- 2.
- Please mark on the line below your worst level of pain during LOCAL ANAESTHETIC INFILTRATION:
- 3.
- Please mark on the line below your worst level of pain during BIOPSY:
- 4.
- Would you be willing to undergo the same procedure under local anaesthetic or would you prefer sedation or a general anaesthetic?
 Local anaesthetic
Local anaesthetic Sedation or general anaestheticFor office use only:Please fill out any additional analgesia used post-operatively. Leave blank if none was used.
Sedation or general anaestheticFor office use only:Please fill out any additional analgesia used post-operatively. Leave blank if none was used.Analgesic Doses Route Total Dose Were there any complications prior to discharge? Circle: Yes/NoDetails:_______________________________________________________________________________________________________________________________________________
Details of biopsy:
- Unilateral/Bilateral
- Number of cores:Left: ____________________Right: ___________________
- Use of needle guide: YES/NO
- Volume of local anaesthetic _____________________mL
- PSA: _______________, volume of prostate: __________________other details (if any):
- Detection details (biopsy results):
Appendix B
There were insufficient data to demonstrate a threshold dose of local anaesthetic associated with a VAS of under 3 total in the control group or intervention group, including when accounting or differences in core numbers.
Inconclusive refers to when the highest volume of LA used in the group is not associated with a VAS < 3.

Table A1.
Comparison of the LA volume used, and threshold VAS in the control and intervention group as subdivided by number of cores. Cores: biopsy cores taken; LA: local anaesthetic; US: ultrasound; VAS: visual analogue scale; VAS-Biopsy: VAS when the needle biopsy is taken; VAS-LA infiltration: VAS when LA was administered; VAS-Probe insertion: VAS at ultrasound probe insertion; VAS-Overall: the average VAS of the score at US insertion, LA infiltration, and when the biopsy is taken.
Table A1.
Comparison of the LA volume used, and threshold VAS in the control and intervention group as subdivided by number of cores. Cores: biopsy cores taken; LA: local anaesthetic; US: ultrasound; VAS: visual analogue scale; VAS-Biopsy: VAS when the needle biopsy is taken; VAS-LA infiltration: VAS when LA was administered; VAS-Probe insertion: VAS at ultrasound probe insertion; VAS-Overall: the average VAS of the score at US insertion, LA infiltration, and when the biopsy is taken.
| For all Core Numbers | For 4 Cores | For 5–8 Cores | For 9–24 Cores | |||||
|---|---|---|---|---|---|---|---|---|
| LA Volume | Control | Intervention | Control | Intervention | Control | Intervention | Control | Intervention |
| Highest volume in the group | 40 mL | 27 mL | 30 mL | 20 mL | 30 mL | 27 mL | 40 mL | 25 mL |
| VAS-Overall < 3 | 40 mL | 27 mL | Inconclusive | 20 mL | 25 mL | 27 mL | 40 mL | Inconclusive |
| VAS-Probe insertion < 3 | 40 mL | 27 mL | Inconclusive | 20 mL | 25 mL | 27 mL | 40 mL | Inconclusive |
| Amount of LA used where VAS-LA infiltration < 3 | 40 mL | 27 mL | Inconclusive | Inconclusive | 30 mL | 27 mL | 40 mL | Inconclusive |
| Amount of LA used where VAS-Biopsy < 3 | Conclusive | 27 mL | 30 mL | 17 mL | 25 mL | 27 mL | Inconclusive | Inconclusive |
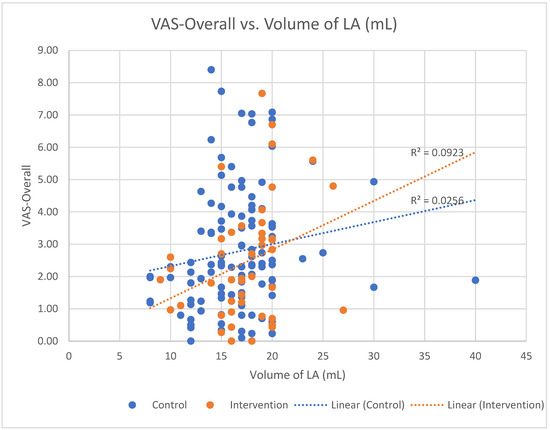
Figure A1.
The VAS-Overall score associated with the volume of LA used in the control and intervention cohorts.
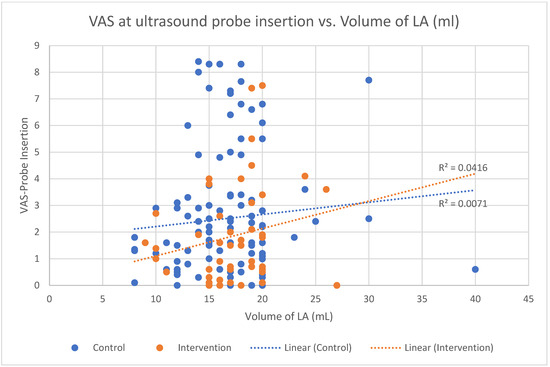
Figure A2.
The VAS at ultrasound probe insertion associated with the volume of LA used in the control and intervention cohorts.
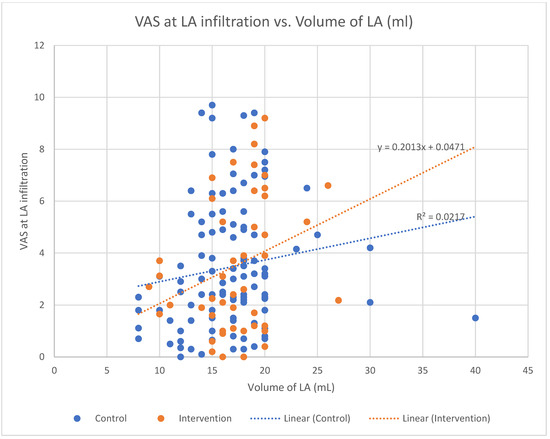
Figure A3.
The VAS at LA infiltration linked to the volume of LA used in the control and intervention cohorts.
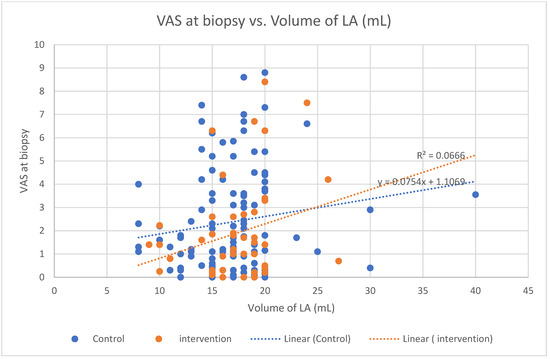
Figure A4.
The VAS at biopsy linked to the volume of LA administered for the control and intervention cohort.
References
- Sung, Y.-T.; Wu, J.-S. The visual analogue scale for rating, ranking and paired-comparison (VAS-RRP): A new technique for psychological measurement. Behav. Res. Methods 2018, 50, 1694–1715. [Google Scholar] [CrossRef] [PubMed]
- Welfare AIoHa. Cancer in Australia 2021; Australian Institute of Health and Welfare: Canberra, Australia, 2021. Available online: https://www.aihw.gov.au/ (accessed on 24 October 2023).
- Mottet, N.; van den Bergh, R.C.; Briers, E.; Van den Broeck, T.; Cumberbatch, M.G.; De Santis, M.; Fanti, S.; Fossati, N.; Gandaglia, G.; Gillessen, S. EAU-EANM-ESTRO-ESUR-SIOG guidelines on prostate cancer—2020 update. Part 1: Screening, diagnosis, and local treatment with curative intent. Eur. Urol. 2021, 79, 243–262. [Google Scholar] [CrossRef] [PubMed]
- Moe, A.; Hayne, D. Transrectal ultrasound biopsy of the prostate: Does it still have a role in prostate cancer diagnosis? Transl. Androl. Urol. 2020, 9, 3018. [Google Scholar] [CrossRef]
- Meyer, A.R.; Joice, G.A.; Schwen, Z.R.; Partin, A.W.; Allaf, M.E.; Gorin, M.A. Initial experience performing in-office ultrasound-guided transperineal prostate biopsy under local anesthesia using the precisionpoint transperineal access system. Urology 2018, 115, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Shen, P.-F.; Zhu, Y.-C.; Wei, W.-R.; Li, Y.-Z.; Yang, J.; Li, Y.-T.; Li, D.-M.; Wang, J.; Zeng, H. The results of transperineal versus transrectal prostate biopsy: A systematic review and meta-analysis. Asian J. Androl. 2012, 14, 310. [Google Scholar] [CrossRef]
- Hu, J.C.; Assel, M.; Allaf, M.E.; Ehdaie, B.; Vickers, A.J.; Cohen, A.J.; Ristau, B.T.; Green, D.A.; Han, M.; Rezaee, M.E. Transperineal versus transrectal magnetic resonance imaging–targeted and systematic prostate biopsy to prevent infectious complications: The PREVENT randomized trial. Eur. Urol. 2024, 86, 61–68. [Google Scholar] [CrossRef]
- Grummet, J.; Gorin, M.A.; Popert, R.; O’Brien, T.; Lamb, A.D.; Hadaschik, B.; Radtke, J.P.; Wagenlehner, F.; Baco, E.; Moore, C.M. “TREXIT 2020”: Why the time to abandon transrectal prostate biopsy starts now. Prostate Cancer Prostatic Dis. 2020, 23, 62–65. [Google Scholar] [CrossRef] [PubMed]
- Bass, E.; Donaldson, I.; Freeman, A.; Jameson, C.; Punwani, S.; Moore, C.; Arya, M.; Emberton, M.; Ahmed, H. Magnetic resonance imaging targeted transperineal prostate biopsy: A local anaesthetic approach. Prostate Cancer Prostatic Dis. 2017, 20, 311–317. [Google Scholar] [CrossRef]
- Hong, A.; Hemmingway, S.; Wetherell, D.; Dias, B.; Zargar, H. Outpatient transperineal prostate biopsy under local anaesthesia is safe, well tolerated and feasible. ANZ J. Surg. 2022, 92, 1480–1485. [Google Scholar] [CrossRef]
- Lopez, J.F.; Campbell, A.; Omer, A.; Stroman, L.; Bondad, J.; Austin, T.; Reeves, T.; Phelan, C.; Leiblich, A.; Philippou, Y. Local anaesthetic transperineal (LATP) prostate biopsy using a probe-mounted transperineal access system: A multicentre prospective outcome analysis. BJU Int. 2021, 128, 311–318. [Google Scholar] [CrossRef]
- Smith, J.B.; Popert, R.; Nuttall, M.C.; Vyas, L.; Kinsella, J.; Cahill, D. Transperineal sector prostate biopsies: A local anesthetic outpatient technique. Urology 2014, 83, 1344–1349. [Google Scholar] [CrossRef] [PubMed]
- Thurtle, D.; Starling, L.; Leonard, K.; Stone, T.; Gnanapragasam, V. Improving the safety and tolerability of local anaesthetic outpatient transperineal prostate biopsies: A pilot study of the CAMbridge PROstate Biopsy (CAMPROBE) method. J. Clin. Urol. 2018, 11, 192–199. [Google Scholar] [CrossRef] [PubMed]
- Wertheimer, S.; Budzyn, J.; Perkins, S.; Borchert, A.; Rogers, C.; Patel, A. Patient Tolerability With Office Transperineal Biopsy Using a Reusable Needle Guide. Urology 2021, 154, 339–341. [Google Scholar] [CrossRef]
- Hogan, D.; Kanagarajah, A.; Yao, H.H.; Wetherell, D.; Dias, B.; Dundee, P.; Chu, K.; Zargar, H.; O’Connell, H.E. Local versus general anesthesia transperineal prostate biopsy: Tolerability, cancer detection, and complications. BJUI Compass 2021, 2, 428–435. [Google Scholar] [CrossRef]
- Lubis, A.M.; Maruanaya, S.; Tantri, A.R.; Pontoh, L.A.P.; Ifran, N.N.P.P.S. The use of combination paracetamol and ibuprofen in postoperative pain after total knee arthroplasty, a randomized controlled trial. Pain Physician 2021, 24, E1199. [Google Scholar]
- Bailey, E.; Worthington, H.; Coulthard, P. Ibuprofen and/or paracetamol (acetaminophen) for pain relief after surgical removal of lower wisdom teeth, a Cochrane systematic review. Br. Dent. J. 2014, 216, 451–455. [Google Scholar] [CrossRef] [PubMed]
- Dahl, J.B.; Møiniche, S. Pre-emptive analgesia. Br. Med. Bull. 2005, 71, 13–27. [Google Scholar] [CrossRef]
- Hall, B.; Coll, S.; Crozier, J.; Hill, A.; Hill, N.; Ooi, E.; Woo, H.; Wu, R. Surgical Audit Guide; Royal Australiasian College of Surgeons: East Melbourne, Australia, 2021; Available online: https://www.surgeons.org/-/media/Project/RACS/surgeons-org/files/reports-guidelines-publications/manuals-guidelines/surgical-audit-and-peer-review-guide.pdf (accessed on 24 October 2023).
- Kuppusamy, S.; Faizal, N.; Quek, K.F.; Razack, A.; Dublin, N. The efficacy of periprostatic local anaesthetic infiltration in transrectal ultrasound biopsy of prostate: A prospective randomised control study. World J. Urol. 2010, 28, 673–676. [Google Scholar] [CrossRef]
- Kelly, A.M. Does the clinically significant difference in visual analog scale pain scores vary with gender, age, or cause of pain? Acad. Emerg. Med. 1998, 5, 1086–1090. [Google Scholar] [CrossRef]
- Sutton, R.M.; McDonald, E.L.; Shakked, R.J.; Fuchs, D.; Raikin, S.M. Determination of minimum clinically important difference (MCID) in visual analog scale (VAS) pain and foot and ankle ability measure (FAAM) scores after hallux valgus surgery. Foot Ankle Int. 2019, 40, 687–693. [Google Scholar] [CrossRef]
- Rupp, M.-C.; Khan, Z.A.; Dasari, S.P.; Berthold, D.P.; Siebenlist, S.; Imhoff, A.B.; Chahla, J.; Pogorzelski, J. Establishing the Minimal Clinically Important Difference (MCID) and Patient Acceptable Symptomatic State (PASS) for VAS Pain, WOMAC, and Lysholm Scores Following Patellofemoral Inlay Arthroplasty. J. Arthroplast. 2023, 38, 2580–2586. [Google Scholar] [CrossRef] [PubMed]
- Kum, F.; Elhage, O.; Maliyil, J.; Wong, K.; Faure Walker, N.; Kulkarni, M.; Namdarian, B.; Challacombe, B.; Cathcart, P.; Popert, R. Initial outcomes of local anaesthetic freehand transperineal prostate biopsies in the outpatient setting. BJU Int. 2020, 125, 244–252. [Google Scholar] [CrossRef] [PubMed]
- McGrath, S.; Christidis, D.; Clarebrough, E.; Ingle, R.; Perera, M.; Bolton, D.; Lawrentschuk, N. Transperineal prostate biopsy–tips for analgesia. BJU Int. 2017, 120, 164–167. [Google Scholar] [CrossRef] [PubMed]
- Bastide, C.; Lechevallier, E.; Eghazarian, C.; Ortega, J.; Coulange, C. Tolerance of pain during transrectal ultrasound-guided biopsy of the prostate: Risk factors. Prostate Cancer Prostatic Dis. 2003, 6, 239–241. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hou, C.-P.; Lin, Y.-H.; Hsieh, M.-C.; Chen, C.-L.; Chang, P.-L.; Huang, Y.-C.; Tsui, K.-H. Identifying the variables associated with pain during transrectal ultrasonography of the prostate. Patient Prefer. Adherence 2015, 9, 1207–1212. [Google Scholar] [CrossRef]
- Marra, G.; Zhuang, J.; Marquis, A.; Zhao, X.; Calleris, G.; Kan, Y.; Oderda, M.; Huang, H.; Faletti, R.; Zhang, Q. Pain in men undergoing transperineal free-hand multiparametric magnetic resonance imaging fusion targeted biopsies under local anesthesia: Outcomes and predictors from a multicenter study of 1,008 patients. J. Urol. 2020, 204, 1209–1215. [Google Scholar] [CrossRef]
- Dell’Atti, L.; Borea, P.A.; Russo, G.R. Age:“a natural anesthetic” in pain perception during the transrectal ultrasound-guided prostate biopsy procedure. Urol. J. 2011, 78, 257–261. [Google Scholar] [CrossRef]
- Fabiani, A.; Servi, L.; Filosa, A.; Fioretti, F.; Maurelli, V.; Tombolini, F.; Tallè, M.; Mammana, G. May ultrasound probe size influence pain perception of needle piercing during transrectal prostate biopsy? A prospective evaluation. Arch. Ital. Urol. Androl. 2016, 88, 223–227. [Google Scholar] [CrossRef][Green Version]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Published by MDPI on behalf of the Société Internationale d’Urologie. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).