Implementing HoLEP in an Academic Department With Multiple Surgeons in Training: Mentoring Is the Key for Success
Abstract
:Introduction
Materials and Methods
Study population
HoLEP: equipment, technique, and follow-up
Statistical analyses
Results
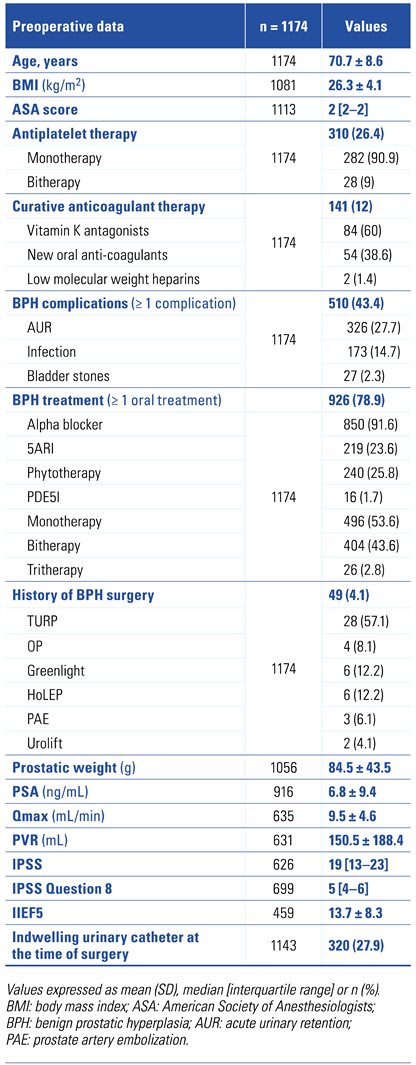 |
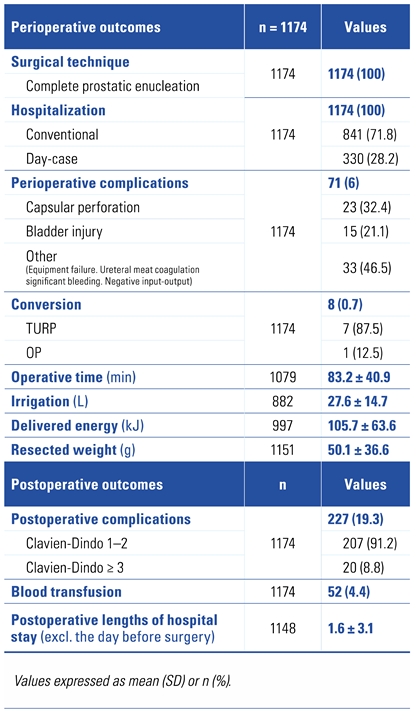 |
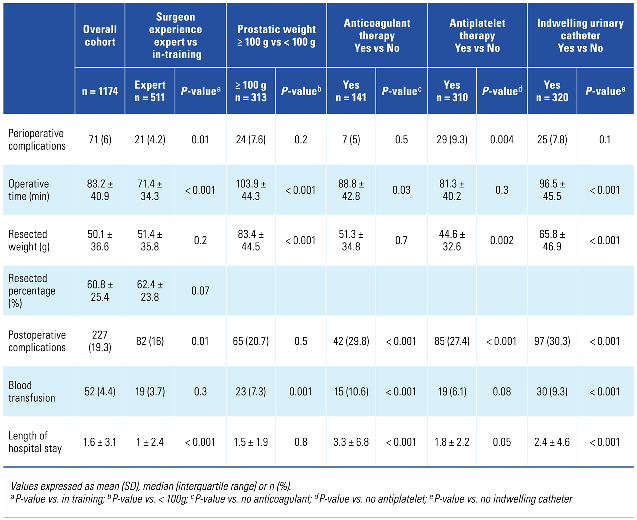 |
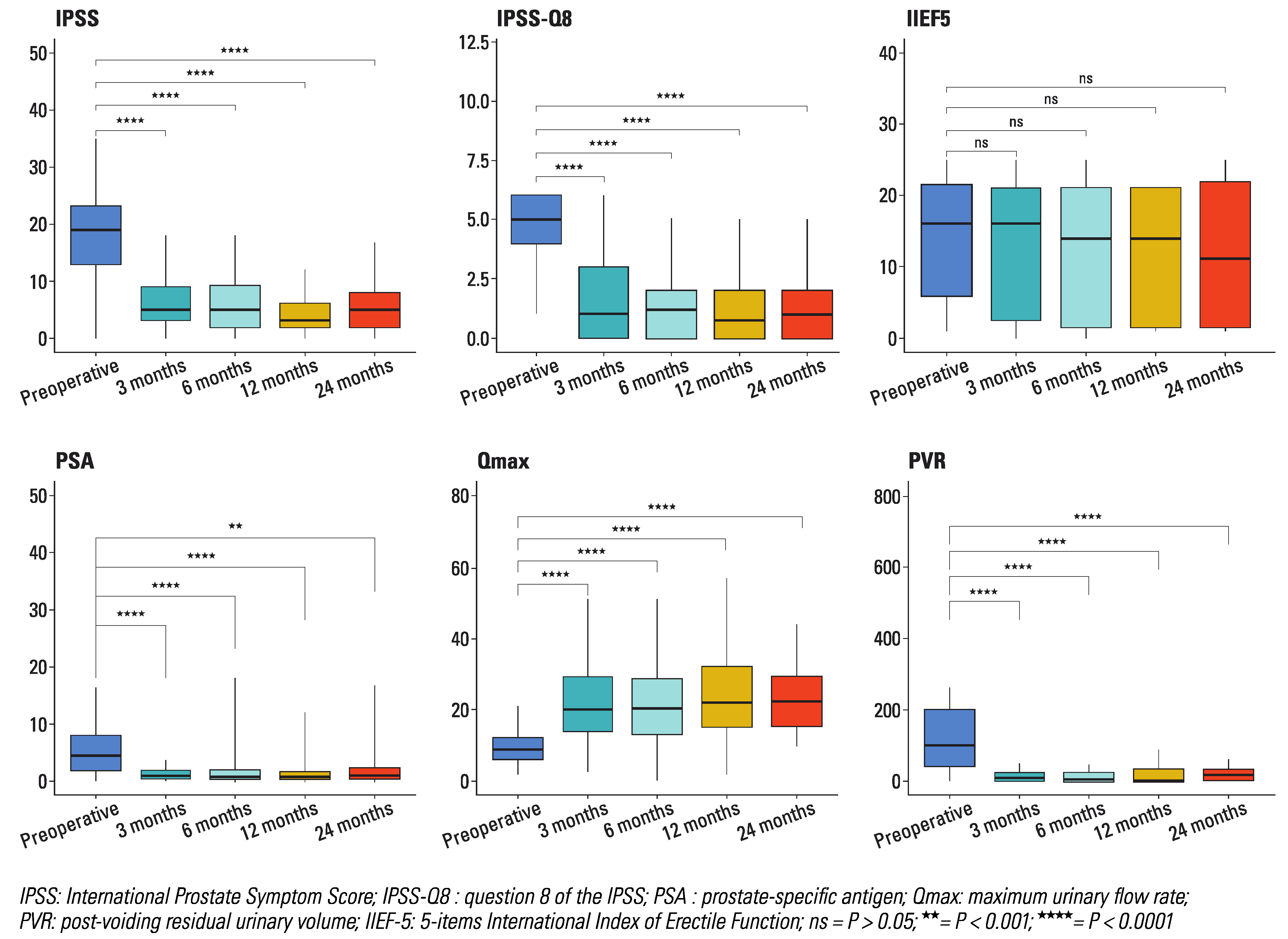
Discussion
Supplementary Materials
Conflicts of Interest
Abbreviations
| BPH | benign prostatic hyperplasia |
| HoLEP | holmium laser enucleation of the prostate |
| mTURP | monopolar transurethral resection of the prostate |
| OP | open prostatectomy |
| UI | urinary incontinence |
References
- Professionals, S.-O. EAU Guidelines: Management of Non-Neurogenic Male LUTS. n.d. Available online: https://uroweb.org/guideline/treatment-of-non-neurogenic-male-luts/#5 (accessed on 27 October 2019).
- Lebdai, S.; Chevrot, A.; Doizi, S.; Pradère, B.; Delongchamps, N.B.; Baumert, H.; et al. Surgical and interventional management of benign prostatic obstruction: Guidelines from the Committee for Male Voiding Disorders of the French Urology Association [article in French]. Prog Urol. 2021, 31, 249–265. [Google Scholar] [CrossRef]
- Tan, A.; Liao, C.; Mo, Z.; Cao, Y. Meta-analysis of holmium laser enucleation versus transurethral resection of the prostate for symptomatic prostatic obstruction. Br J Surg. 2007, 94, 1201–1208. [Google Scholar] [CrossRef] [PubMed]
- Gilling, P.J.; Wilson, L.C.; King, C.J.; Westenberg, A.M.; Frampton, C.M.; Fraundorfer, M.R. Long-term results of a randomized trial comparing holmium laser enucleation of the prostate and transurethral resection of the prostate: results at 7 years. BJU Int. 2012, 109, 408–411. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Qiu, J.; Hou, Q.; Wang, D.; Huang, W.; Hu, C.; et al. Endoscopic enucleation versus open prostatectomy for treating large benign prostatic hyperplasia: a meta-analysis of randomized controlled trials. Schwentner C. ed. PLoS One 2015, 10, e0121265. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.; Wu, X.; Xu, A.; Ren, R.; Zhou, X.; Wen, Y.; et al. Transurethral enucleation of the prostate versus transvesical open prostatectomy for large benign prostatic hyperplasia: a systematic review and meta-analysis of randomized controlled trials. World J Urol. 2016, 34, 1207–1219. [Google Scholar] [CrossRef] [PubMed]
- Tooher, R.; Sutherland, P.; Costello, A.; Gilling, P.; Rees, G.; Maddern, G.; et al. A systematic review of holmium laser prostatectomy for benign prostatic hyperplasia. J Urol. 2004, 171, 1773–1781. [Google Scholar] [CrossRef] [PubMed]
- Duc, A.L.; Gilling, P.J. Holmium laser resection of the prostate. Eur Urol. 1999, 35, 155–160. [Google Scholar] [CrossRef] [PubMed]
- Fraundorfer, M.R.; Gilling, P.J. Holmium:YAG laser enucleation of the prostate combined with mechanical morcellation: preliminary results. Eur Urol. 1998, 33, 69–72. [Google Scholar] [CrossRef]
- Robert, G.; Cornu, J.-N.; Fourmarier, M.; Saussine, C.; Descazeaud, A.; Azzouzi, A.-R.; et al. Multicentre prospective evaluation of the learning curve of holmium laser enucleation of the prostate (HoLEP). BJU Int. 2016, 117, 495–499. [Google Scholar] [CrossRef]
- Gilling, P.J.; Cass, C.B.; Malcolm, A.R.; Fraundorfer, M.R. Combination holmium and Nd:YAG laser ablation of the prostate: initial clinical experience. J Endourol. 1995, 9, 151–153. [Google Scholar] [CrossRef]
- Mallet, R.; Gamé, X. Énucléation prostatique au laser holmium (HoLEP) « en bloc ». [The en bloc holmium enucleation of the prostate: Technique, tips and tricks]. Prog Urol. 2017, 27, F71–F74. [Google Scholar] [CrossRef]
- Romero-Otero, J.; García-González, L.; García-Gómez, B.; Justo-Quintas, J.; García-Rojo, E.; González-Padilla, D.A.; et al. Factors influencing intraoperative blood loss in patients undergoing holmium laser enucleation of the prostate (HoLEP) for benign prostatic hyperplasia: a large multicenter analysis. Urology 2019, 132, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Montorsi, F.; Naspro, R.; Salonia, A.; Suardi, N.; Briganti, A.; Zanoni, M.; et al. Holmium laser enucleation versus transurethral resection of the prostate: results from a 2-center prospective randomized trial in patients with obstructive benign prostatic hyperplasia. J Urol. 2008, 179 (Suppl. 5), S87–S90. [Google Scholar] [CrossRef] [PubMed]
- Vavassori, I.; Valenti, S.; Naspro, R.; Vismara, A.; Dell’Acqua, V.; Manzetti, A.; et al. Three-year outcome following holmium laser enucleation of the prostate combined with mechanical morcellation in 330 consecutive patients. Eur Urol. 2008, 53, 599–606. [Google Scholar] [CrossRef] [PubMed]
- Ahyai, S.A.; Lehrich, K.; Kuntz, R.M. Holmium laser enucleation versus transurethral resection of the prostate: 3-year follow-up results of a randomized clinical trial. Eur Urol. 2007, 52, 1456–1464. [Google Scholar] [CrossRef] [PubMed]
- Enikeev, D.; Taratkin, M.; Morozov, A.; Singla, N.; Gabdulina, S.; Tarasov, A.; et al. Long-term outcomes of holmium laser enucleation of the prostate: a 5-year single-center experience. J Endourol. 2020, 34, 1055–1063. [Google Scholar] [CrossRef] [PubMed]
- Elzayat, E.A.; Elhilali, M.M. Holmium laser enucleation of the prostate (HoLEP): long-term results, reoperation rate, and possible impact of the learning curve. Eur Urol. 2007, 52, 1465–1472. [Google Scholar] [CrossRef]
- Nam, J.K.; Kim, H.W.; Lee, D.H.; Han, J.-Y.; Lee, J.Z.; Park, S.-W. Risk factors for transient urinary incontinence after holmium laser enucleation of the prostate. World J Mens Health 2015, 33, 88. [Google Scholar] [CrossRef] [PubMed]
- Cho, M.C.; Park, J.H.; Jeong, M.S.; Yi, J.-S.; Ku, J.H.; Oh, S.-J.; et al. Predictor of de novo urinary incontinence following holmium laser enucleation of the prostate. Neurourol Urodyn. 2011, 30, 1343–1349. [Google Scholar] [CrossRef]
- Houssin, V.; Olivier, J.; Brenier, M.; Pierache, A.; Lamiado, M.; Mouton, M.; et al. Predictive factors of urinary incontinence after holmium laser enucleation of the prostate: a multicentric evaluation. World J Urol. 2021, 39, 143–148. [Google Scholar] [CrossRef]
- Shigemura, K.; Yamamichi, F.; Kitagawa, K.; Yamashita, M.; Oka, Y.; Tanaka, H.; et al. Does surgeon experience affect operative time, adverse events and continence outcomes in holmium laser enucleation of the prostate? a review of more than 1,000 cases. J Urol. 2017, 198, 663–670. [Google Scholar] [CrossRef] [PubMed]
- Abrams, P.; Andersson, K.E.; Birder, L.; Brubaker, L.; Cardozo, L.; Chapple, C.; et al. Fourth International Consultation on Incontinence recommendations of the international scientific committee: evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourol Urodyn. 2010, 29, 213–240. [Google Scholar] [CrossRef] [PubMed]
- Elshal, A.M.; Nabeeh, H.; Eldemerdash, Y.; Mekkawy, R.; Laymon, M.; El-Assmy, A.; et al. Prospective assessment of learning curve of holmium laser enucleation of the prostate for treatment of benign prostatic hyperplasia using a multidimensional approach. J Urol. 2017, 197, 1099–1107. [Google Scholar] [CrossRef] [PubMed]
- Elkoushy, M.A.; Elshal, A.M.; Elhilali, M.M. Reoperation after holmium laser enucleation of the prostate for management of benign prostatic hyperplasia: assessment of risk factors with time to event analysis. J Endourol. 2015, 29, 797–804. [Google Scholar] [CrossRef] [PubMed]
- Du, C.; Jin, X.; Bai, F.; Qiu, Y. Holmium laser enucleation of the prostate: the safety, efficacy, and learning experience in China. J Endourol. 2008, 22, 1031–1036. [Google Scholar] [CrossRef]
- Vincent, M.W.; Gilling, P.J. HoLEP has come of age. World J Urol. 2015, 33, 487–493. [Google Scholar] [CrossRef]
This is an open access article under the terms of a license that permits non-commercial use, provided the original work is properly cited. © 2023 The Authors. Société Internationale d'Urologie Journal, published by the Société Internationale d'Urologie, Canada.
Share and Cite
Klein, C.; Marquette, T.; Capon, G.; Alezra, E.; Blanc, P.; Estrade, V.; Bernhard, J.-C.; Bladou, F.; Robert, G. Implementing HoLEP in an Academic Department With Multiple Surgeons in Training: Mentoring Is the Key for Success. Soc. Int. Urol. J. 2023, 4, 11-18. https://doi.org/10.48083/UJCR1584
Klein C, Marquette T, Capon G, Alezra E, Blanc P, Estrade V, Bernhard J-C, Bladou F, Robert G. Implementing HoLEP in an Academic Department With Multiple Surgeons in Training: Mentoring Is the Key for Success. Société Internationale d’Urologie Journal. 2023; 4(1):11-18. https://doi.org/10.48083/UJCR1584
Chicago/Turabian StyleKlein, Clément, Thibault Marquette, Grégoire Capon, Eric Alezra, Peggy Blanc, Vincent Estrade, Jean-Christophe Bernhard, Franck Bladou, and Grégoire Robert. 2023. "Implementing HoLEP in an Academic Department With Multiple Surgeons in Training: Mentoring Is the Key for Success" Société Internationale d’Urologie Journal 4, no. 1: 11-18. https://doi.org/10.48083/UJCR1584
APA StyleKlein, C., Marquette, T., Capon, G., Alezra, E., Blanc, P., Estrade, V., Bernhard, J.-C., Bladou, F., & Robert, G. (2023). Implementing HoLEP in an Academic Department With Multiple Surgeons in Training: Mentoring Is the Key for Success. Société Internationale d’Urologie Journal, 4(1), 11-18. https://doi.org/10.48083/UJCR1584





