Outcomes of Robotic Surgery for Low-Volume Surgeons
Abstract
:Introduction
Low-Volume Robotic Surgeons and/or Hospital
Methods
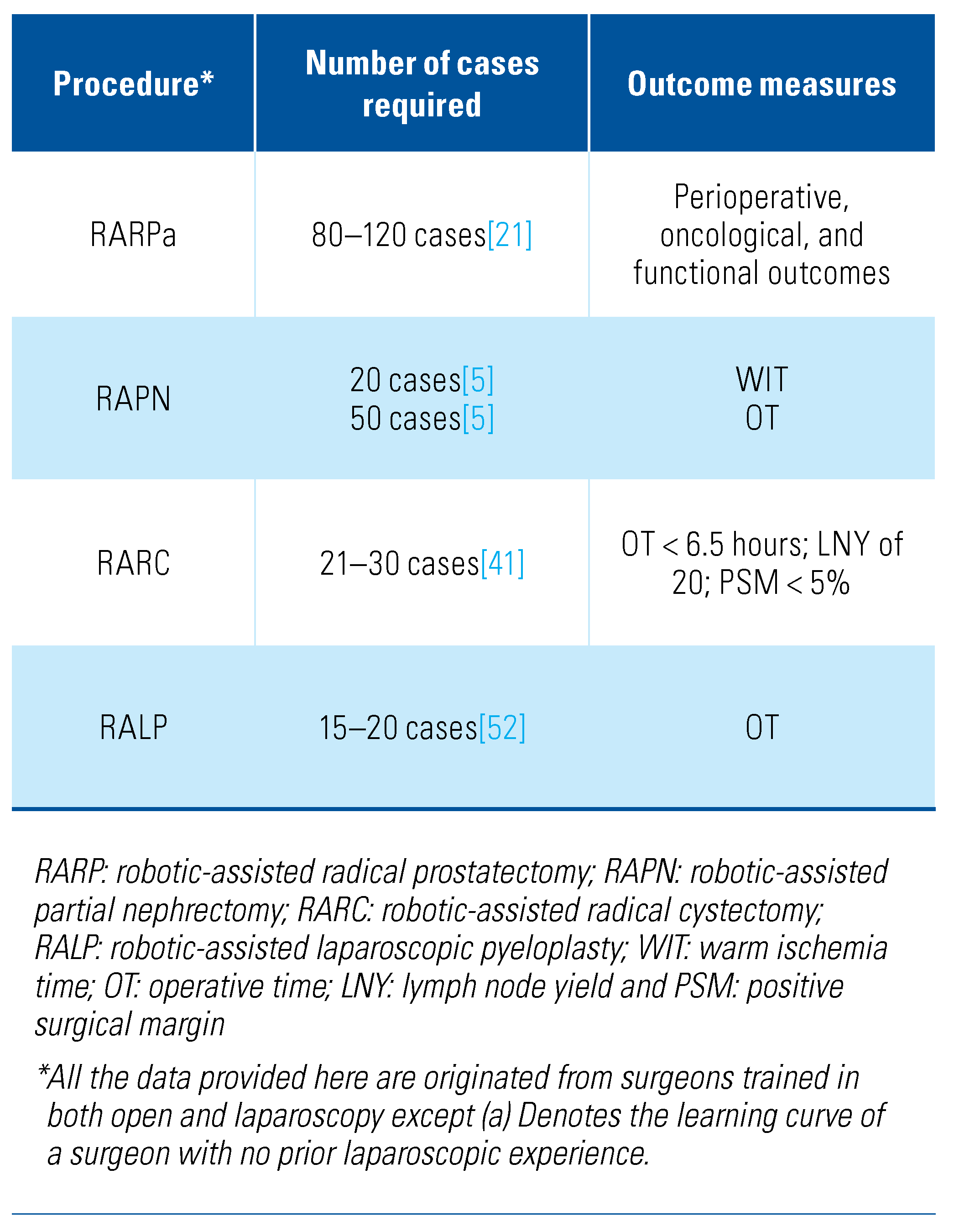
Radical Prostatectomy
Partial Nephrectomy
Radical Cystectomy
Pyeloplasty
Ergonomics
Role of Various Robotic Training Models
Conclusion
Competing Interests
Abbreviations
| EBL | estimated blood loss |
| LNY | lymph node yield |
| LPN | laparoscopic partial nephrectomy |
| OT | operative time |
| PSM | positive surgical margin |
| RALP | robotic-assisted laparoscopic pyeloplasty |
| RAPN | robotic-assisted partial nephrectomy |
| RARC | robotic-assisted radical cystectomy |
| RARP | robotic-assisted radical prostatectomy |
| WIT | warm ischemia time |
References
- Venkatramani, V. Urovision 2020: The future of urology. Indian J. Urol. 2015, 31, 150–155. [Google Scholar] [CrossRef]
- Buia, A.; Stockhausen, F.; Hanisch, E. Laparoscopic surgery: A qualified systematic review. World J. Methodol. 2015, 5, 238–254. [Google Scholar] [CrossRef]
- Kumar, R.; Hemal, A.K. Emerging role of robotics in urology. J. Minim. Access Surg. 2005, 1, 202–210. [Google Scholar] [CrossRef]
- Vincent, C.; Moorthy, K.; Sarker, S.K.; Chang, A.; Darzi, A.W. Systems approaches to surgical quality and safety: From concept to measurement. Ann. Surg. 2004, 239, 475–482. [Google Scholar] [CrossRef] [PubMed]
- Abboudi, H.; Khan, M.S.; Guru, K.A.; Froghi, S.; de Win, G.; Van Poppel, H.; et al. Learning curves for urological procedures: A systematic review: Learning curves for urological procedures. BJU Int. 2014, 114, 617–629. [Google Scholar] [CrossRef] [PubMed]
- Shah, J.; Vyas, A.; Vyas, D. The history of robotics in surgical specialties. Am. J. Robot. Surg. 2014, 1, 12–20. [Google Scholar] [CrossRef]
- Ashrafian, H.; Clancy, O.; Grover, V.; Darzi, A. The evolution of robotic surgery: Surgical and anaesthetic aspects. Br. J. Anaesth. 2017, 119 (Suppl. 1), i72–i84. [Google Scholar] [CrossRef] [PubMed]
- Farivar, B.S.; Flannagan, M.; Leitman, I.M. General surgery residents’ perception of robot-assisted procedures during surgical training. J. Surg. Educ. 2015, 72, 235–242. [Google Scholar] [CrossRef]
- Dhanani, N.H.; Olavarria, O.A.; Bernardi, K.; Lyons, N.B.; Holihan, J.L.; Loor, M.; et al. The evidence behind robot-assisted abdominopelvic surgery: A systematic review. Ann. Intern. Med. 2021, 174, 1110–1117. [Google Scholar] [CrossRef]
- Wilt, T.J.; Shamliyan, T.A.; Taylor, B.C.; MacDonald, R.; Kane, R.L. Association between hospital and surgeon radical prostatectomy volume and patient outcomes: A systematic review. J. Urol. 2008, 180, 820–828; discussion 828–829. [Google Scholar] [CrossRef]
- Panaiyadiyan, S.; Kumar, R. Robotic assistance helps low-volume surgeons deliver better outcomes to their patients. Indian J. Urol. 2021, 37, 1. [Google Scholar] [CrossRef] [PubMed]
- Anderberg, M.; Larsson, J.; Kockum, C.C.; Arnbjörnsson, E. Robotics versus laparoscopy—An experimental study of the transfer effect in maiden users. Ann. Surg. Innov. Res. 2010, 4, 3. [Google Scholar] [CrossRef]
- Ahlering, T.E.; Skarecky, D.; Lee, D.; Clayman, R.V. Successful transfer of open surgical skills to a laparoscopic environment using a robotic interface: Initial experience with laparoscopic radical prostatectomy. J. Urol. 2003, 170, 1738–1741. [Google Scholar] [CrossRef] [PubMed]
- Azhar, R.A.; Elkoushy, M.A.; Aldousari, S. Robot-assisted urological surgery in the Middle East: Where are we and how far can we go? Arab. J. Urol. 2019, 17, 106–113. [Google Scholar] [CrossRef] [PubMed]
- Koukourikis, P.; Rha, K.H. Robotic surgical systems in urology: What is currently available? Investig. Clin. Urol. 2021, 62, 14–22. [Google Scholar] [CrossRef] [PubMed]
- Gershman, B.; Meier, S.K.; Jeffery, M.M.; Moreira, D.M.; Tollefson, M.K.; Kim, S.P.; et al. Redefining and contextualizing the hospital volume-outcome relationship for robot-assisted radical prostatectomy: Implications for centralization of care. J. Urol. 2017, 198, 92–99. [Google Scholar] [CrossRef] [PubMed]
- Bravi, C.A.; Tin, A.; Vertosick, E.; Mazzone, E.; Martini, A.; Dell’Oglio, P.; et al. The impact of experience on the risk of surgical margins and biochemical recurrence after robot-assisted radical prostatectomy: A learning curve study. J. Urol. 2019, 202, 108–113. [Google Scholar] [CrossRef]
- Godtman, R.A.; Persson, E.; Cazzaniga, W.; Sandin, F.; Carlsson, S.; Ahlgren, G.; et al. Association of surgeon and hospital volume with short-term outcomes after robot-assisted radical prostatectomy: Nationwide, population-based study. PLoS ONE 2021, 16, e0253081. [Google Scholar] [CrossRef]
- Coelho, R.F.; Rocco, B.; Patel, M.B.; Orvieto, M.A.; Chauhan, S.; Ficarra, V.; et al. Retropubic, laparoscopic, and robot-assisted radical prostatectomy: A critical review of outcomes reported by high-volume centers. J. Endourol. 2010, 24, 2003–2015. [Google Scholar] [CrossRef]
- Leow, J.J.; Leong, E.K.; Serrell, E.C.; Chang, S.L.; Gruen, R.L.; Png, K.S.; et al. Systematic review of the volume-outcome relationship for radical prostatectomy. Eur. Urol. Focus. 2018, 4, 775–789. [Google Scholar] [CrossRef]
- Vickers, A.J.; Savage, C.J.; Hruza, M.; Tuerk, I.; Koenig, P.; Martínez-Piñeiro, L.; et al. The surgical learning curve for laparoscopic radical prostatectomy: A retrospective cohort study. Lancet Oncol. 2009, 10, 475–480. [Google Scholar] [CrossRef]
- Gumus, E.; Boylu, U.; Turan, T.; Onol, F.F. The learning curve of robot- assisted radical prostatectomy. J. Endourol. 2011, 25, 1633–1637. [Google Scholar] [CrossRef]
- Hirasawa, Y.; Yoshioka, K.; Nasu, Y.; Yamamoto, M.; Hinotsu, S.; Takenaka, A.; et al. Impact of surgeon and hospital volume on the safety of robot-assisted radical prostatectomy: A multi-institutional study based on a national database. Urol. Int. 2017, 98, 334–342. [Google Scholar] [CrossRef]
- Garg, H.; Seth, A.; Singh, P.; Kumar, R. Changing trends in robot- assisted radical prostatectomy: Inverse stage migration-a retrospective analysis. Prostate Int. 2021, 9, 157–162. [Google Scholar] [CrossRef] [PubMed]
- Azhar, R.A.; Aldousari, S.; Alghamdi, M.M.; Alotaibi, M.F.; Alkhateeb, S.S.; Nassir, A.M.; et al. Robot-assisted radical prostatectomy in low-volume regions: Should it be abandoned or adopted? A multi-institutional outcome study. J. Endourol. 2021, 35, 1013–1019. [Google Scholar] [CrossRef]
- Afferi, L.; Moschini, M.; Baumeister, P.; Zamboni, S.; Cornelius, J.; Ineichen, G.; et al. Trends in risk-group distribution and Pentafecta outcomes in patients treated with nerve-sparing, robot-assisted radical prostatectomy: A 10-year low-intermediate volume single- center experience. World J. Urol. 2021, 39, 389–397. [Google Scholar] [CrossRef]
- Miller, D.C.; Hollingsworth, J.M.; Hafez, K.S.; Daignault, S.; Hollenbeck, B.K. Partial nephrectomy for small renal masses: An emerging quality of care concern? J. Urol. 2006, 175 Pt 1, 853–857; discussion 858. [Google Scholar] [CrossRef] [PubMed]
- You, C.; Du, Y.; Wang, H.; Peng, L.; Wei, T.; Zhang, X.; et al. Laparoscopic versus open partial nephrectomy: A systemic review and meta- analysis of surgical, oncological, and functional outcomes. Front. Oncol. 2020, 10, 583979. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.; Wang, W.; Xiong, Z.; Yang, Z.; Li, J.; Shen, Y.; et al. Comparison of perioperative outcomes between laparoscopic and open partial nephrectomy for different complexity renal cell carcinoma based on the R.E.N.A.L. nephrometry score. CMAR 2021, 13, 7455–7461. [Google Scholar] [CrossRef]
- Jain, S.; Gautam, G. Robotics in urologic oncology. J. Minim. Access Surg. 2015, 11, 40–44. [Google Scholar] [CrossRef]
- Abouassaly, R.; Alibhai, S.M.H.; Tomlinson, G.; Timilshina, N.; Finelli, A. Unintended consequences of laparoscopic surgery on partial nephrectomy for kidney cancer. J. Urol. 2010, 183, 467–472. [Google Scholar] [CrossRef]
- Cheung, H.; Wang, Y.; Chang, S.L.; Khandwala, Y.; Del Giudice, F.; Chung, B.I. Adoption of robot-assisted partial nephrectomies: A population-based analysis of U.S. surgeons from 2004 to 2013. J. Endourol. 2017, 31, 886–892. [Google Scholar] [CrossRef] [PubMed]
- Hanzly, M.; Frederick, A.; Creighton, T.; Atwood, K.; Mehedint, D.; Kauffman, E.C.; et al. Learning curves for robot-assisted and laparoscopic partial nephrectomy. J. Endourol. 2015, 29, 297–303. [Google Scholar] [CrossRef]
- Gill, I.S.; Kamoi, K.; Aron, M.; Desai, M.M. 800 Laparoscopic partial nephrectomies: A single surgeon series. J. Urol. 2010, 183, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Aldousari, S.; Yaiesh, S.; Alkandari, O. Total robotic surgical volume influences outcomes of low-volume robotic-assisted partial nephrectomy over an extended duration. CUAJ 2021, 15. [Google Scholar] [CrossRef]
- Dias, B.; Ali, M.; Dubey, S.; Krishnaswamy, S.; Rao, A.; Dubey, D. Impact of learning curve on the perioperative outcomes following robot-assisted partial nephrectomy for renal tumors. Indian J. Urol. 2018, 34, 62. [Google Scholar] [CrossRef]
- Motoyama, D.; Matsushita, Y.; Watanabe, H.; Tamura, K.; Suzuki, T.; Ito, T.; et al. Initial learning curve for robot-assisted partial nephrectomy performed by a single experienced robotic surgeon. Asian J. Endosc. Surg. 2020, 13, 59–64. [Google Scholar] [CrossRef] [PubMed]
- Peyronnet, B.; Tondut, L.; Bernhard, J.-C.; Vaessen, C.; Doumerc, N.; Sebe, P.; et al. Impact of hospital volume and surgeon volume on robot- assisted partial nephrectomy outcomes: A multicentre study. BJU Int. 2018, 121, 916–922. [Google Scholar] [CrossRef]
- Yokoyama, M.; Ishioka, J.; Toba, M.; Fukushima, H.; Tanaka, H.; Yoshida, S.; et al. Trends and safety of robot-assisted partial nephrectomy during the initial 2-year period after government approval in Japan: A nationwide database study from 2016 to 2018. Int. J. Urol. 2021, 28, 1268–1272. [Google Scholar] [CrossRef]
- Basatac, C.; Akpinar, H. « Trifecta » outcomes of robot-assisted partial nephrectomy: Results of the « low volume » surgeon. Int. Braz. J. Urol. 2020, 46, 943–949. [Google Scholar] [CrossRef]
- Parekh, D.J.; Reis, I.M.; Castle, E.P.; Gonzalgo, M.L.; Woods, M.E.; Svatek, R.S.; et al. Robot-assisted radical cystectomy versus open radical cystectomy in patients with bladder cancer (RAZOR): An open-label, randomised, phase 3, non-inferiority trial. Lancet 2018, 391, 2525–2536. [Google Scholar] [CrossRef] [PubMed]
- Venkatramani, V.; Reis, I.M.; Castle, E.P.; Gonzalgo, M.L.; Woods, M.E.; Svatek, R.S.; et al. Predictors of recurrence, and progression-free and overall survival following open versus robotic radical cystectomy: Analysis from the RAZOR Trial with a 3-Year followup. J. Urol. 2020, 203, 522–529. [Google Scholar] [CrossRef] [PubMed]
- Hayn, M.H.; Hussain, A.; Mansour, A.M.; Andrews, P.E.; Carpentier, P.; Castle, E.; et al. The Learning curve of robot-assisted radical cystectomy: Results from the International Robotic Cystectomy Consortium. Eur. Urol. 2010, 58, 197–202. [Google Scholar] [CrossRef]
- Guru, K.A.; Perlmutter, A.E.; Butt, Z.M.; Piacente, P.; Wilding, G.E.; Tan, W.; et al. The learning curve for robot-assisted radical cystectomy. JSLS 2009, 13, 509–514. [Google Scholar] [CrossRef] [PubMed]
- Hayn, M.H.; Hellenthal, N.J.; Hussain, A.; Andrews, P.E.; Carpentier, P.; Castle, E.; et al. Does previous robot-assisted radical prostatectomy experience affect outcomes at robot-assisted radical cystectomy? Results from the International Robotic Cystectomy Consortium. Urology 2010, 76, 1111–1116. [Google Scholar] [CrossRef] [PubMed]
- Shrivastava, N.; Nayak, B.; Dogra, P.; Kumar, R.; Singh, P. Robot-assisted laparoscopic radical cystectomy with extracorporeal urinary diversion: Initial experience and outcomes. Indian J. Urol. 2018, 34, 122–126. [Google Scholar] [CrossRef]
- Dothan, D.; Raisin, G.; Jaber, J.; Kocherov, S.; Chertin, B. Learning curve of robotic-assisted laparoscopic pyeloplasty (RALP) in children: How to reach a level of excellence? J. Robotic Surg. 2021, 15, 93–97. [Google Scholar] [CrossRef]
- Hemal, A.K.; Mishra, S.; Mukharjee, S.; Suryavanshi, M. Robot assisted laparoscopic pyeloplasty in patients of ureteropelvic junction obstruction with previously failed open surgical repair. Int. J. Urol. 2008, 15, 744–746. [Google Scholar] [CrossRef]
- Nayyar, R.; Gupta, N.P.; Hemal, A.K. Robotic management of complicated ureteropelvic junction obstruction. World J. Urol. 2010, 28, 599–602. [Google Scholar] [CrossRef]
- Bora, G.S.; Parmar, K.; Mavuduru, R.S. Robot-assisted pyeloplasty for pelvi-ureteric junction obstruction of lower moiety in partial duplex system: A technical challenge. Indian. J. Urol. 2016, 32, 314–316. [Google Scholar] [CrossRef]
- Numakura, K.; Muto, Y.; Saito, M.; Narita, S.; Inoue, T.; Habuchi, T. Robot- assisted laparoscopic pyeloplasty for ureteropelvic junction obstruction with duplex system. Urol. Case Rep. 2020, 30, 101138. [Google Scholar] [CrossRef] [PubMed]
- Dirie, N.I.; Ahmed, M.A.; Mohamed, M.A.; Zhang, Z.; Wang, S. Robot-assisted laparoscopic pyeloplasty in adults: A comparison analysis of primary versus redo pyeloplasty in a single center. Urol. J. 2020, 18, 45–50. [Google Scholar] [CrossRef] [PubMed]
- Tasian, G.E.; Casale, P. The robotic-assisted laparoscopic pyeloplasty: Gateway to advanced reconstruction. Urol. Clin. N. Am. 2015, 42, 89–97. [Google Scholar] [CrossRef] [PubMed]
- Sorensen, M.D.; Delostrinos, C.; Johnson, M.H.; Grady, R.W.; Lendvay, T.S. Comparison of the learning curve and outcomes of robotic assisted pediatric pyeloplasty. J. Urol. 2011, 185 (Suppl. 6), 2517–2522. [Google Scholar] [CrossRef] [PubMed]
- Bowen, D.K.; Lindgren, B.W.; Cheng, E.Y.; Gong, E.M. Can proctoring affect the learning curve of robotic-assisted laparoscopic pyeloplasty? Experience at a high-volume pediatric robotic surgery center. J. Robotic Surg. 2017, 11, 63–67. [Google Scholar] [CrossRef] [PubMed]
- Maheshwari, P.; Arora, A. Robot-assisted pyeloplasty: The way forward. J. Min. Access Surg. 2021, 17, 274. [Google Scholar] [CrossRef] [PubMed]
- Gabrielson, A.T.; Clifton, M.M.; Pavlovich, C.P.; Biles, M.J.; Huang, M.; Agnew, J.; et al. Surgical ergonomics for urologists: A practical guide. Nat. Rev. Urol. 2021, 18, 160–169. [Google Scholar] [CrossRef] [PubMed]
- Catanzarite, T.; Tan-Kim, J.; Whitcomb, E.L.; Menefee, S. Ergonomics in surgery: A review. Female Pelvic Med. Reconstr. Surg. 2018, 24, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Kumar, R.; Nayak, B. Robotic versus conventional laparoscopic pyeloplasty: A single surgeon concurrent cohort review. Indian. J. Urol. 2013, 29, 19–21. [Google Scholar] [CrossRef]
- Margossian, H.; Garcia-Ruiz, A.; Falcone, T.; Goldberg, J.M.; Attaran, M.; Miller, J.H.; et al. Robotically assisted laparoscopic tubal anastomosis in a porcine model: A pilot study. J. Laparoendosc. Adv. Surg. Tech. A 1998, 8, 69–73. [Google Scholar] [CrossRef]
- Santok, G.D.; Raheem, A.A.; Kim, L.H.; Chang, K.; Chung, B.H.; Choi, Y.D.; et al. Proctorship and mentoring: Its backbone and application in robotic surgery. Investig. Clin. Urol. 2016, 57 (Suppl. 2), S114. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, A.; Tan, L.G.L.; Chiong, E.; Rha, K.H.; Tiong, H.Y. Transitioning to robotic partial nephrectomy with a team-based proctorship achieves the desired improved outcomes over open and laparoscopic partial nephrectomy. Updates Surg. 2021, 73, 1189–1196. [Google Scholar] [CrossRef] [PubMed]
- Mason, M.D.; Herndon, C.D.A.; Herbst, K.W.; Poston, T.L.; Brandt, E.J.; Peters, C.A.; et al. Proctor environment facilitates faculty training in pediatric robotic-assisted laparoscopic pyeloplasty. J. Robotic Surg. 2014, 8, 365–369. [Google Scholar] [CrossRef]
- Santomauro, M.; Reina, G.A.; Stroup, S.P.; L’Esperance, J.O. Telementoring in robotic surgery. Curr. Opin. Urol. 2013, 23, 141–145. [Google Scholar] [CrossRef] [PubMed]
- El Sherbiny, A.; Eissa, A.; Ghaith, A.; Morini, E.; Marzotta, L.; Sighinolfi, M.C.; et al. Training in urological robotic surgery. Future perspectives. Arch. Esp. Urol. 2018, 71, 97–107. [Google Scholar]
- Canalichio, K.L.; Berrondo, C.; Lendvay, T.S. Simulation training in urology: State of the art and future directions. Adv. Med. Educ. Pract. 2020, 11, 391–396. [Google Scholar] [CrossRef]
This is an open access article under the terms of a license that permits non-commercial use, provided the original work is properly cited. © 2022 The Authors. Société Internationale d'Urologie Journal, published by the Société Internationale d'Urologie, Canada.
Share and Cite
Panaiyadiyan, S.; Kumar, R. Outcomes of Robotic Surgery for Low-Volume Surgeons. Soc. Int. Urol. J. 2022, 3, 323-330. https://doi.org/10.48083/PPSC8658
Panaiyadiyan S, Kumar R. Outcomes of Robotic Surgery for Low-Volume Surgeons. Société Internationale d’Urologie Journal. 2022; 3(5):323-330. https://doi.org/10.48083/PPSC8658
Chicago/Turabian StylePanaiyadiyan, Sridhar, and Rajeev Kumar. 2022. "Outcomes of Robotic Surgery for Low-Volume Surgeons" Société Internationale d’Urologie Journal 3, no. 5: 323-330. https://doi.org/10.48083/PPSC8658
APA StylePanaiyadiyan, S., & Kumar, R. (2022). Outcomes of Robotic Surgery for Low-Volume Surgeons. Société Internationale d’Urologie Journal, 3(5), 323-330. https://doi.org/10.48083/PPSC8658





