Abstract
The lower urinary tract (LUT), in particular the prostate, has been theoretically recognized as a target for SARS-CoV-2. Moreover, common pathophysiological mechanisms have been described for BPE/LUTS and COVID-19, including RAS dysregulation, androgen receptors, and MetS-related factors. These factors raise concerns about the possibility of worse urological outcomes due to BPE/LUTS progression in COVID-19 patients. The available results suggest a correlation between SARS-CoV-2 infection, exacerbation or new onset of LUTS, and semen impairment. BPE patients’ care and management have been deeply affected by COVID-19. In the midst of the pandemic, the main urological guidelines suggested postponement of BPH-related deferrable medical examinations and surgery. Telemedicine, therefore, gained attention and interest. Clinical evidence of impaired QoL or complications expedited surgical intervention. An informed consent covering the risk of COVID-19 and a negative molecular PCR within 72 h of surgery were mandatory. A reduction in procedures under general anaesthesia was recommended. Long waiting lists accrued worldwide during the pandemic, leading to regular review of the BPE waiting lists and patients’ clinical status, encouraging the increase of minimally invasive office-based procedures, even in the post-COVID-19 era, and the improvement of telemedicine. Prospective studies are still needed to assess the course of LUTS/BPE patients after COVID-19.
Introduction
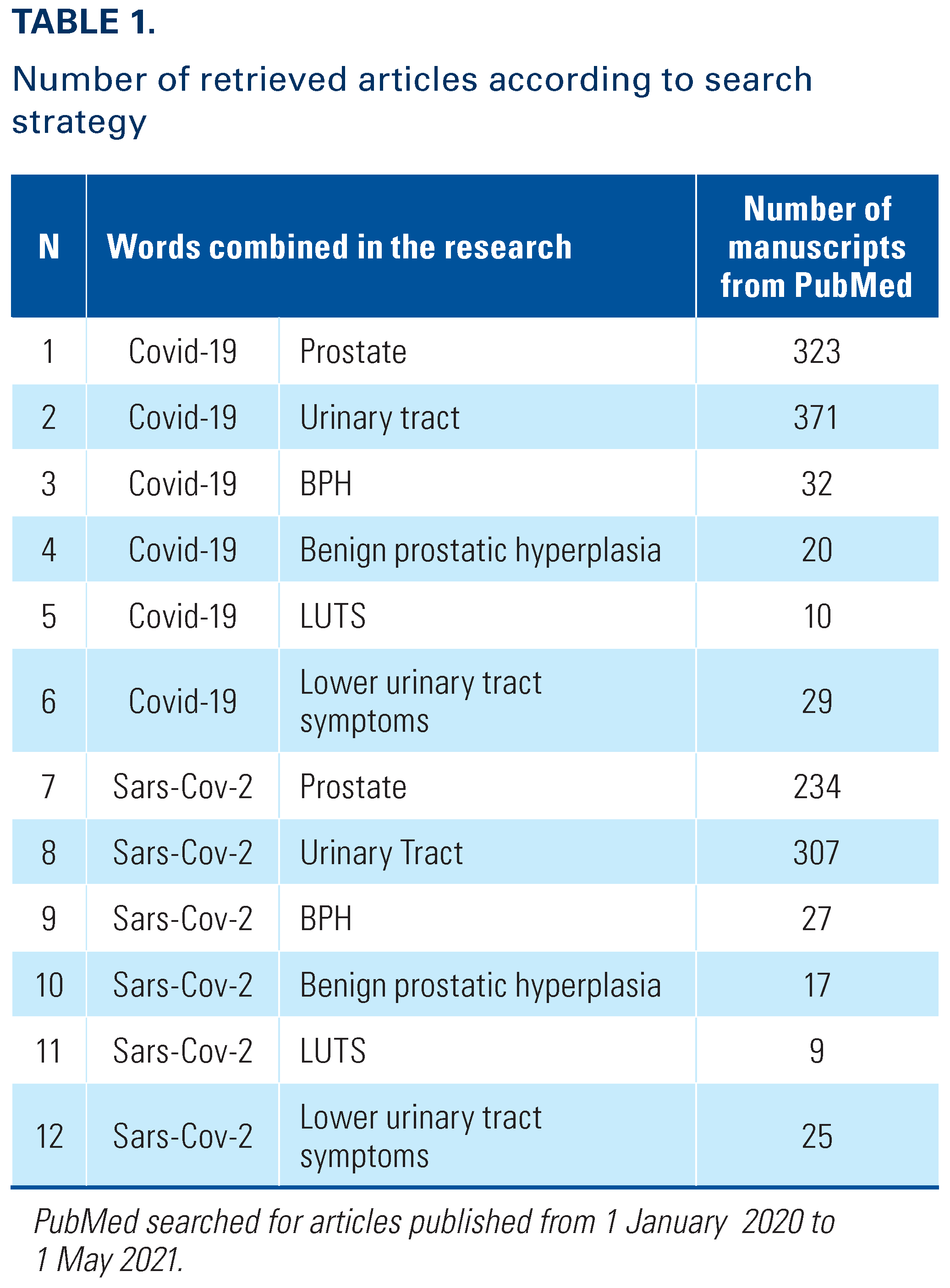
The COVID-19 pandemic due to SARS-CoV-2 represents one of the most severe threats to human health in the last century. Epidemiologic data suggest that COVID-19 preponderance and severity have been worse in elderly men, who are also more prone to benign prostatic enlargement (BPE), with significant implication from the pathophysiological point of view for development and progression of both conditions (Figure 1) [1,2,3].
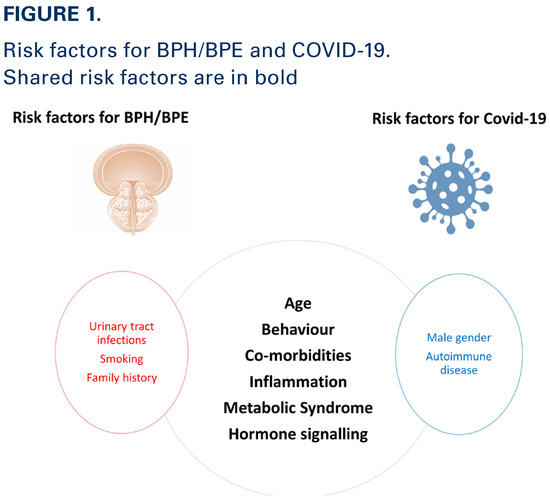
Figure 1.
Moreover, during the last year, most urologic centres all over the word progressively discontinued visits and surgical procedures for several benign diseases, including benign prostatic obstruction (BPO), which had a significant impact on quality of life and daily activities of millions of men. The management of lower urinary tract symptoms (LUTS) due to benign prostatic hyperplasia (BPH) during the pandemic remains an outstanding practical challenge.
The aim of the present review is to better understand the pathophysiology of Sars-CoV-2 infection in the male urinary tract and to evaluate the risks related to COVID-19 in men under medical treatment for BPO, including the clinical progression of LUTS after COVID-19 infection. We have focused on the management of LUTS/BPO patients during COVID-19 with the aim of learning how we might be prepared to deal with future pandemics.
Materials and Methods
Search Strategy and Study Selection
An extensive MEDLINE, Embase, and Cochrane search was performed, using the following terms: “COVID-19,” “SARS-Cov-2,” “prostate,” “urinary tract,” “BPH,” “benign prostatic hyperplasia,” “LUTS,” “lower urinary tract symptoms” (Table 1).

Table 1.
The search for articles published before May 1, 2021, was restricted to English-language articles and studies of human participants. A hand-search of bibliographies of retrieved papers for additional references was performed. Details of the literature search process are outlined in the flow chart (Figure 2). The identification of relevant abstracts, the selection of studies based on the criteria described above, and the subsequent data extraction were performed independently by 2 of the authors, and conflicts resolved by a third investigator. Full-text articles and meeting abstracts were included.
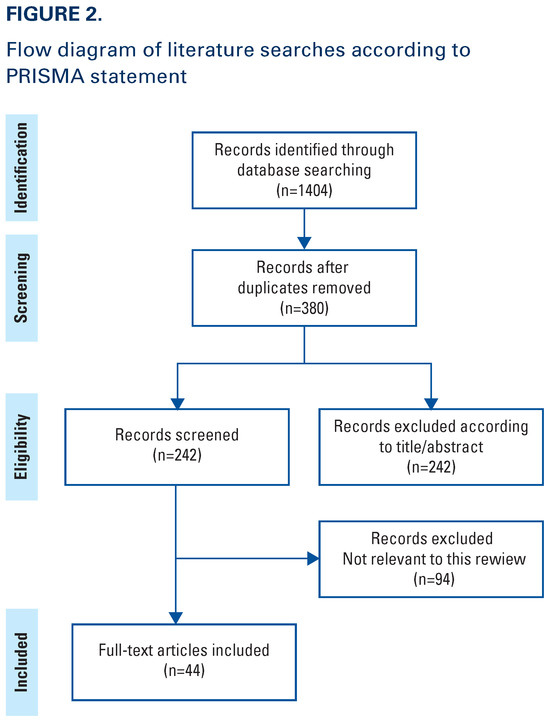
Figure 2.
Outcome and Quality Assessment
The principal outcomes of this analysis were to evaluate (1) the pathophysiology of SARS-CoV-2 infection in male LUT; (2) the risks related to COVID-19 in men under medical treatment for BPO; (3) the risk of LUTS progression after COVID-19; (4) the management of LUTS/BPO patients during the pandemic, including the need for surgery; and (5) what we have learned for the future.
Pathophysiological Considerations
The lower urinary tract (LUT), in particular the prostate, has been recognized as a hypothetical target for SARS-CoV-2 (Figure 3). Currently, only a few clinical studies have evaluated the effect of COVID-19 on the male LUT, and these suggest a relation between SARS-CoV-2 and LUTS. A systematic review by Haghpanah et al.3 reported that hyperactivation of the renin-angiotensin system (RAS) during a SARS-CoV-2 infection may lead to activation of pro-inflammatory pathways, cytokine release, and exacerbation of LUTS, and may trigger prostate inflammatory processes. Another systematic review of 16 studies evaluating the involvement of the urinary and male genital system in COVID-19, reported de novo LUTS and deterioration of pre-existing LUTS [4]. Interestingly, Karabulut et al. [5] prospectively followed 63 men diagnosed with COVID-19 and divided them into 3 categories based upon IPSS (mild, moderate, severe). Patients with severe LUTS (IPSS 20-35) had longer hospital stays, more frequent and faster time to admission in intensive care, and higher mortality rates.
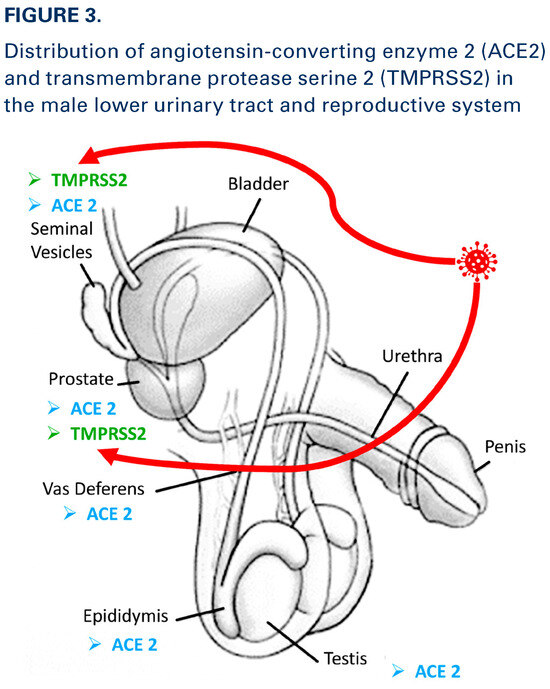
Figure 3.
SARS-CoV-2 invades host cells using a structural spike (S) protein which binds to the angiotensin-converting enzyme (ACE2) receptor [6]. In addition to a viral inflammatory response with an increase in neutrophils and monocytes, there is loss of the epithelial-endothelial barrier integrity with edema resulting in impaired oxygen diffusion [7]. Ultimately diffuse coagulation and viral sepsis from dysregulated host response to infection leads to multi-organ failure [8].
The devastating effects of SARS-CoV-2 on multiple organ systems have been well described. A number of studies have examined the pathophysiology and resultant effects of COVID-19 in urine, semen, and the male genitourinary tract [9]. The target cell for infections, ACE2 receptor, has been identified in up to 2.4% of urothelial cells, potentially making them susceptible to SARS-CoV-2 infection [10]. When SARS-CoV-2 binds to the ACE2 receptor, RAS becomes hyperactivated, resulting in pro-inflammatory cytokine release. This can cause inflammation within the prostate, which is exacerbated when the androgen receptor (AR), responsible for BPH pathophysiology, is activated by COVID-19, which may, itself, be androgen-mediated. SARS-CoV-2 entry into cells is dependent on S protein cleavage by the transmembrane protease serine 2 (TMPRSS2) expressed on the surface of human cells, which is mediated by androgens and the ARs [5].
Mumm et al. [11] found increased urinary frequency in 7/57 male patients with COVID-19, but viral RNA was not detected in the urine of these patients. It has been hypothesized that SARS-CoV-2 could potentially induce viral cystitis through either viremia from basal urothelial cells or urine from the luminal side. However, it seems more likely that cystitis could be blood borne, since no viral RNA was seen in urine, but rather was present in serum. Accordingly, the term COVID-19-associated cystitis (CAC) has been used to describe the new onset of urinary frequency > 12 episodes in 24 h and >3 episodes of nocturia [12]. Lamb et al. [12]. collected urine in patients with CAC and healthy age-matched controls. All COVID-19 patients had elevated levels of inflammatory cytokines, including IL-6, IL-8, and IP-10 in their urine, while COVID-19 negative controls showed no elevated cytokines. Therefore, the risk of SARS-CoV-2 transmission through urine seems a remote possibility. In a meta-analysis by Kashi et al. [13], COVID-19 was detected in 24 of 533 samples (4.5%) with a viral shedding frequency of 1.18%.
Regarding semen parameters, Holtmann et al. [14] studied men recovered from mild and moderate COVID-19 infections. Men with moderate infections demonstrated a statistically significant reduction in sperm concentration, total number of sperm per ejaculate, and progressive and complete motility, whereas mild cases and controls showed no differences. Gacci et al. [9] reported that one-quarter of men who recovered from COVID-19 demonstrated oligo-crypto-azoospermia. Pathological levels of IL-8 in semen occurred in 76.7% of patients, with a significant correlation between oligo-crypto-azoospermia appearance and COVID-19 severity. Conversely, Guo et al. [15] found normal semen parameters in a cohort of men who had recovered from mild COVID-19.
Medical Treatments for LUTS Due to BPE and COVID-19
5-alpha-reductase inhibitors (5-ARIs) therapeutically reduce the size of the prostate gland by decreasing the serum and intraprostatic dihydrotestosterone (DHT) level [16], and block 5-AR isoform 3, which is expressed in the respiratory epithelium and fibroblasts [17]. Androgens, including DHT, disrupt communication between fibroblasts and type II alveolar cells by a mechanism involving transforming growth factor beta (TGF-β) and epidermal growth factor EGF (EGF) receptor signalling pathways [18,19].
Interstitial pneumonia is the main cause of life-threatening respiratory disorders at the severe stage of COVID-19 infection. Proper functioning of respiratory epithelium and maintenance and restoration of lung surfactant layer may be controlled by androgen metabolism, in which 5-alpha-reductase plays a key role [20]. Therefore, 5-ARIs may negatively affect such functions by disrupting androgen metabolism [21]. However, further studies are still needed to assess whether a discontinuation of 5-alpha-reductase inhibitors may be beneficial for patients who tested positive for SARS-CoV-2, especially for those at high risk for the disease [22]. Conversely, some studies suggest that men chronically exposed to 5-ARIs may be less vulnerable to severe COVID-19 [23], and 5-ARIs may reduce viral shedding, inflammatory response, and time to remission.
Animal studies and retrospective clinical trials suggest that alpha-blockers, especially non-selective ones such as prazosin, may prevent cytokine storm in COVID-19 patients and subsequent need for mechanical ventilation, and may possibly reduce mortality [24]. However, in a retrospective study, Nishimura et al. [25] showed no significant impact of alpha-blockers on hospitalization and the need for ICU admission for COVID-19.
Overall, the impact of medical therapy for BPE/LUTS on COVID-19 severity, progression, and prognosis is still unclear.
Risk of BPE/LUTS Progression After COVID-19
SARS-CoV-2 Infection and RAS
The RAS is a hormonal cascade that regulates blood pressure and cardiovascular function through angiotensin-II (Ang-II) and angiotensin-converting enzyme (ACE). RAS hyperactivity is associated with hypertension [3]. RAS components are locally present in the prostate. Ang-II has been detected in the epithelial basal layer of the prostate, and Ang-II receptor type 1 (AT1R) has been found in the smooth muscle cells of both vessels and the stroma [26]. The expression of ACE and Ang-II is markedly increased in BPE patients. SARS-CoV-2 notably binds to ACE2 receptors, which are expressed in many human tissues such as lung, kidney, prostate, and pancreas, and infects the target tissue [27]. Since ACE2 counteracts the proliferative and inflammatory effects of Ang-II by controlling and inhibiting infection and inflammation, it is hypothesized that COVID-19 and a subsequent downregulation of ACE2 could lead to worsening of BPE/LUTS. Therefore, diminished ACE2 expression and the following ACE2 loss of function in cellular membranes of prostate tissue, due to SARS-CoV-2, could represent trigger signals for BPE/LUTS progression [3]. However, further studies are needed to assess the effects and the clinical impact of SARS-CoV-2 on these pathways.
SARS-CoV-2 Infection and ARs
ARs are widely expressed in both epithelial and stromal prostate cells. Epithelial cell proliferation leads to stromal cell growth via epithelial–stromal cell interaction and epithelial–mesenchymal transition, with increasing evidence linking ARs to BPH through induced stromal proliferation [28]. Wambier et al. [29] hypothesized that SARS-CoV-2 infection may be also androgen-mediated. Indeed, TMPRSS2, a serine protease essential for priming of the viral spike protein, requires AR activity for its gene transcription [29]. Lamy et al. [30] reported a greater risk of developing severe COVID-19 among male patients with androgenetic alopecia, supporting the hypothesis that COVID-19 might be androgen-mediated. However, much controversy still exists regarding the role of androgen pathways in the pathophysiology of COVID-19.
Metabolic Syndrome: Is MetS Associated with both BPE/LUTS and COVID-19?
The propensity for development of BPE/LUTS is well documented in patients with metabolic syndrome (MetS) due to prostatic gland proliferation induced by insulin, related trophic factors, sex steroid hormonal change, and consequently increased inflammation and oxidative stress [31,32]. ACE2, the main entry receptor for SARS-CoV-2, is also expressed in adipose tissue and pancreatic beta cells and could help explain why some COVID-19 patients present new onset or exacerbation of pre-existing metabolic conditions such as diabetes [3,33]. Moreover, patients with obesity induced MetS presented an enhanced ACE2 expression that may increase the susceptibility to SARS-CoV-2 infection [34].
Indeed, Ghoneim et al. observed that patients with a primary diagnosis of MetS experienced a significative cumulative higher incidence of COVID-19 (OR 7.00 [6.11–8.01]) [35].
Taking into account that MetS components are recognized as risk factors for BPE/LUTS [32] and currently associated with worse clinical outcomes in COVID-19 patients, a pathophysiological interconnection appears possible and should be addressed in future clinical studies.
BPE/LUTS Management During the Pandemic
General Considerations
The care and management of BPE patients have been deeply affected by the COVID-19 pandemic, and the use of tele-urology (telephone and/or video virtual consultations) where facilities permitted was implemented or augmented. Non-operative alternatives and reduction in investigations, including imaging modalities, was advised [36,37,38]. In particular, Morselli et al. [39] tested the use of the MyBPHcare App, a new app developed by uCARE project from the SIU Office of Research, which proved a useful solution to avoiding contagion for both patients and physician during the pandemic.
Amparore et al. [40] reviewed the COVID-19 related guideline modifications of 13 urological associations, which suggested postponing deferrable medical examinations. Shared indications for urgent face-to-face (F2F) consultations for BPE/LUTS were clot retention, acute urinary retention, and chronic retention.
A more robust triage and upgrade of technical telemedicine support was required to comply with these recommendations [41,42]. Inpatient admissions were indicated for indwelling catheter requirements, Rezum treatment, significant haematuria requiring haemostatic transurethral resection, and other minimally invasive surgical therapies (MISTs) for BPE or bladder stones. Non-urgent surgical interventions were postponed [43,44].
In May of 2020, the European Association of Urology Guidelines Office Rapid Reaction Group published a disease risk stratification. The categories were Life threatening (P4), High priority with potential harm if delays exceeded 6 weeks (P3), Intermediate priority with harm possible but unlikely with delays of up to 3 to 4 months (P2), and Low priority with harm unlikely with up to 6-month treatment delays (P1) [45]. It was identified that delays in definitive treatment following initial care did not increase threat to patients with BPE. Moreover, there was evidence that BPE did not worsen outcome of COVID-19 patients [46], even though a weak theoretical possibility of LUTS exacerbation with COVID existed [3].
Requirements for BPE/LUTS Surgery during the Pandemic
Clinical evidence of impaired QoL or complications (recurrent or significant haematuria, symptomatic bladder stones, upper tract compromise), and consequent upgrade of patient priority risk, expedited surgical intervention. An informed consent covering the risk of COVID-19 and associated complications was a prerequisite for surgery [45,47,48], and a negative molecular PCR status within 72 h of surgery was mandatory [47].
Level 2 or 3 PPE was recommended for use by the anaesthetic team. The population within the operating theatre was regulated, and the procedure performed by the surgeon with the greatest experience to limit the operating time [45]. A reduction in procedures under general anaesthesia was recommended [43]. The Urological Society of Australia and New Zealand recommended barring theatre suite access to non-anaesthetic team members for 20 min after intubation or extubation [49].
Surgeons were required to aspirate bubbles during endoscopic procedures to reduce the theoretic probability of steam and smoke bubble aerosolization [43]. A closed suction system for irrigation fluids was recommended [50]. Chlorine (500 to 10 000 mg/L), 75% ethanol, peracetic acid [51] or other locally approved disinfectant with effect against COVID-19 was recommended [45]. Chlorhexidine was reportedly ineffective against COVID-19 [45].
Challenges of Instituted Modifications
It was expected that extending the period before surgery for BPE would imply more catheter-related urethral injuries, catheter-associated urinary tract infections (CAUTIs), and antibiotic use [40,52,53]. To prevent this, UroShield (Ideal Medical Solutions, Surrey, United Kingdom) was developed as an external device to cause acoustic vibrations that reduce the biofilm around indwelling catheters. It has been approved by the National Institute for Health and Care Excellence (NICE) for use in the United Kingdom [54]. In Canada, the BIP Foley TempSensor (Bactiguard, Tullinge, Sweden) [55] was granted interim approval during the COVID-19 pandemic. It uses silver alloy hydrogel and is associated with a 47% reduction in CAUTIs [56].
Older patients with BPE, aged ≥ 65 years, have been documented to experience declines in social function and increased levels of anxiety and depression due to worsening LUTS following delays in BPE treatment [57]. Indeed, the COVIDSurge Collaborative study involving/conducted in 190 countries alluded to treatment delays causing a reduction in physical ability and work productivity. In lowand middle-income countries, this resulted in many patients being unable to pay for their surgery by the time it was scheduled, which, in turn, resulted in further deterioration of their physical condition and overall well-being [58].
Recovery of Elective Surgery for BPE/LUTS
Long waiting lists accrued worldwide during the pandemic. Pathways to catch up exigently and safely on elective surgery were essential. Regular review of the BPE waiting lists and patients’ clinical status was paramount, with re-evaluation of assigned priorities, and feedback to designated Elective Care Recovery Leads [41].
Adherence to guidelines for outpatient care of non-urgent benign conditions was reported to decrease inpatient admissions by 43% during the COVID pandemic in one centre in China [59]. Cross-site flexibility for urologists was also established to permit urgent surgeries in hospitals in the independent sector, which were experiencing less COVID-related capacity strain [41].
In a bid to permit TURPs but limit the strain on inpatient bed availability, another centre in the United Kingdom showed a significant reduction in decision-making time and overnight stays when specialist nurses took decisions about who required a ward-based or clinic-based TWOC, postoperatively [60].
In April 2020, the National Health Service in Fife, Scotland, adopted local anaesthetic (LA) technique to reduce operating theatre and general anaesthesia requirements [61].
Finance and Insurance-Related Issues
Although coverage for telehealth expanded with COVID-19, poor reimbursement provisions of extant Telehealth Commercial Payer Statutes occurred in America [62]. Some states in America established reimbursement parity for virtual and F2F consultations only in January 2021 [62]. The use of separate insurance coverage for telemedicine consultations was discouraged to eliminate the exclusion of some practitioners [62]. Also cost-shifting protections restricting higher patient charges for virtual consultations were encouraged [63].
Relevant waivers were provided by the Federation of State Medical Boards in America [62]. In France, L’Assurance Maladie, the national insurance provider, increased coverage provisions from thousands to over 5 million by April 2020 [64]. Belgian policies included reimbursement for virtual triage as well [32]. On the market front, a global decline in sales and revenue from BPE treatment-related devices was recorded, with a 5.2% decline in sales and −2.9% in annual growth rate [65].
Lessons Learned: What We Have to Do in Future
Promoting Telemedicine
Before 2020, telemedicine was gaining attention, but its widespread use was limited. Several papers had determined that the use of telemedicine was effective in urology. In prostate cancer, it served as a means for continuing patient treatment and care. The main advantages reported by patients were savings on travel time and costs and reduced family time interruption [66]. Concern was expressed for the potential risk of inaccuracy, suboptimal documentation, inability to examine, and the omission of relevant clinical information during telephone consultations [67].
The adoption of telemedicine and its potential use after the pandemic were analyzed in a global survey of 620 urologists. This survey demonstrated that 81% of urologists who were regular users during the pandemic planned to continue in the future. A proportion (68%) felt that at least half of their appointments should be done F2F. The use of telemedicine increased from 16% before the pandemic to 46% at the time of the report [68].
Symptom scores and bladder diaries can be emailed to patients [69]. However, tele-apps, such as MyBPH Care (Ydeal, Portugal), permitted monitoring of LUTS through virtual interactions and QoL-related patient-reported outcome measures, patient-initiated contact, and the issuance of timely prescriptions or identification of a need for F2F reviews [39].
Minimally Invasive Office-Based Procedures for BPE/LUTS
The delayed definitive management of BPE patients through the pandemic implies significant challenges due to the high prevalence of the disease, and its natural history being linked to progression and deterioration. The long-term sequelae on outcomes from the postponed diagnosis and treatment remain to be determined. As many of the international societies recommended deferring BPE treatment, a close follow-up to prevent potential complications as well as optimization of medical therapy and inclusion of minimally invasive ambulatory procedures is recommended [40].
Moreover, depending on the severity, BPE-related symptoms can have significant effects on mental health [57]. The allocation of operating rooms to COVID-positive cases, restrictions regarding oxygen demands and the pressing need for ventilators during the pandemic highlighted the need to treat more BPE patients using MISTs, under local anaesthesia or light IV sedation, to limit adverse sequelae from these delays [43,50].
Meetings, Education, and Training
The pandemic and the consequent lockdowns in many countries came with an unprecedented opportunity to move from physical to virtual events. While networking opportunities were identified as higher in F2F meetings, online webinars were more cost-effective. Learning opportunities and reach of audience were higher with hybrid meetings. In one survey undertaken in the first year of the pandemic, more than half of all respondents reported a preference for hybrid meetings [70].
Surgical training was adversely affected during the pandemic. The reduction in BPE surgeries and surgical ward availability for inpatient care resulted in a loss of surgical exposure. Recommendations for the more skilled surgeons to perform procedures to minimize operating times and complications further reduced trainee exposure [71].
Deployment of residents and faculty staff to COVID-19 wards, quarantines, closure of services, and reduced patient contact time have had a negative effect on medical education. A nationwide survey conducted by the Society of Academic Urologists (SAU) reported reserve staffing in 80% of the programmes, resident redeployment in 26%, and residents under formal quarantine in 55% of programmes [72].
Several programmes were developed in different modalities. Virtual education programmes have enabled urology trainees to pursue their education during the pandemic. Although the long-term impact on training is still unknown, new and innovative educational strategies have been developed [73].
Conclusion
The pandemic has had a revolutionary impact on BPH management and has created awareness of knowledge deficits and alternative approaches to care, which require more research. Preliminary epidemiological and pathophysiological information suggest a potential correlation between Covid-19 and LUTS due to BPE. The risk-benefit analysis of medical treatment for BPE in COVID-19 patients is still under investigation. The use of telemedicine and minimally invasive office-based procedures should be improved in the postCOVID-19 era.
Competing Interests
None declared.
Abbreviations
| ACE2 | angiotensin-converting enzyme |
| BPE | benign prostatic enlargement |
| BPH | benign prostatic hyperplasia |
| CAC | COVID-19 associated cystitis |
| F2F | face-to-face |
| LUTS | lower urinary tract symptoms |
| MetS | metabolic syndrome |
| PPE | personal protection equipment |
| RAS | renin-angiotensin system |
| TMPRSS2 | transmembrane protease serine 2 |
References
- Li, L.Q.; Huang, T.; Wang, Y.Q.; Wang, Z.P.; Liang, Y.; Huang, T.B.; et al. COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J. Med. Virol. 2020, 92, 577–583. [Google Scholar] [CrossRef] [PubMed]
- Guan, W.J.; Ni, Z.Y.; Hu, Y.; Liang, W.H.; Ou, C.Q.; He, J.X.; et al. China Medical Treatment Expert Group for Covid-19. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Haghpanah, A.; Masjedi, F.; Salehipour, M.; Hosseinpour, A.; Roozbeh, J.; Dehghani, A. Is COVID-19 a risk factor for progression of benign prostatic hyperplasia and exacerbation of its related symptoms?: A systematic review. Prostate Cancer Prostatic Dis. 2021, 18, 1–12. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Creta, M.; Sagnelli, C.; Celentano, G.; Napolitano, L.; La Rocca, L.; Capece, M.; et al. SARS-CoV-2 infection affects the lower urinary tract and male genital system: A systematic review. J. Med. Virol. 2021, 93, 3133–3142. [Google Scholar] [CrossRef] [PubMed]
- Karabulut, I.; Cinislioglu, A.E.; Cinislioglu, N.; Yilmazel, F.K.; Utlu, M.; Alay, H.; et al. The effect of the presence of lower urinary system symptoms on the prognosis of COVID-19: Preliminary results of a prospective study. Urol. Int. 2020, 104, 853–858. [Google Scholar] [CrossRef] [PubMed]
- Barnes, C.O.; West, A.P., Jr.; Huey-Tubman, K.E.; Hoffmann, M.A.G.; Sharaf, N.G.; Hoffman, P.R.; et al. Structures of human antibodies bound to SARS-CoV-2 spike reveal common epitopes and recurrent features of antibodies. Cell 2020, 182, 828–842. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Xu, Z.; Shi, L.; Wang, Y.; Zhang, J.; Huang, L.; Zhang, C.; et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020, 8, 420–422. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tang, N.; Li, D.; Wang, X.; Sun, Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J. Thromb. Haemost. 2020, 18, 844–847. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gacci, M.; Coppi, M.; Baldi, E.; Sebastianelli, A.; Zaccaro, C.; Morselli, S.; et al. Semen impairment and occurrence of SARS-CoV-2 virus in semen after recovery from COVID-19. Hum. Reprod. 2021, 36, 1520–1529. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zou, X.; Chen, K.; Zou, J.; Han, P.; Hao, J.; Han, Z. Single-cell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019-nCoV infection. Front. Med. 2020, 14, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Mumm, J.N.; Osterman, A.; Ruzicka, M.; Stihl, C.; Vilsmaier, T.; Munker, D.; et al. Urinary frequency as a possibly overlooked symptom in COVID-19 patients: Does SARS-CoV-2 cause viral cystitis? Eur. Urol. 2020, 78, 624–628. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lamb, L.E.; Dhar, N.; Timar, R.; Wills, M.; Dhar, S.; Chancellor, M.B. COVID-19 inflammation results in urine cytokine elevation and causes COVID-19 associated cystitis (CAC). Med. Hypotheses 2020, 145, 110375. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kashi, A.H.; De la Rosette, J.; Amini, E.; Abdi, H.; Fallah-Karkan, M.; Vaezjalali, M. Urinary viral shedding of COVID-19 and its clinical associations: A systematic review and meta-analysis of observational studies. Urol. J. 2020, 17, 433–441. [Google Scholar] [CrossRef] [PubMed]
- Holtmann, N.; Edimiris, P.; Andree, M.; Doehmen, C.; Baston-Buest, D.; Adams, O.; et al. Assessment of SARS-CoV-2 in human semen-a cohort study. Fertil. Steril. 2020, 114, 233–238. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Guo, L.; Zhao, S.; Li, W.; Wang, Y.; Li, L.; Jiang, S.; et al. Absence of SARS-CoV-2 in semen of a COVID-19 patient cohort. Andrology 2021, 9, 42–47. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kim, E.H.; Brockman, J.A.; Andriole, G.L. The use of 5-alpha reductase inhibitors in the treatment of benign prostatic hyperplasia. Asian J. Urol. 2018, 5, 28–32. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Azzouni, F.; Godoy, A.; Li, Y.; Mohler, J. The 5 alpha-reductase isozyme family: A review of basic biology and their role in human diseases. Adv. Urol. 2012, 2012, 530121. [Google Scholar] [CrossRef]
- Bresson, E.; Seaborn, T.; Côté, M.; Cormier, G.; Provost, P.R.; Piedboeuf, B.; et al. Gene expression profile of androgen modulated genes in the murine fetal developing lung. Reprod. Biol. Endocrinol. 2010, 8. [Google Scholar] [CrossRef] [PubMed]
- Bhaskaran, M.; Kolliputi, N.; Wang, Y.; Gou, D.; Chintagari, N.R.; Liu, L. Transdifferentiation of alveolar epithelial type II cells to type I cells involves autocrine signaling by transforming growth factor β1 through the SMAD pathway. J. Biol. Chem. 2007, 282, 3968–3976. [Google Scholar] [CrossRef] [PubMed]
- Provost, P.R.; Simard, M.; Tremblay, Y. A link between lung androgen metabolism and the emergence of mature epithelial type II cells. Am. J. Respir. Crit. Care Med. 2004, 170, 296–305. [Google Scholar] [CrossRef]
- Adamowicz, J.; Juszczak, K.; Drewa, T. May patients receiving 5-alphareductase inhibitors be in higher risk of COVID-19 complications? Med. Hypotheses 2020, 140, 109751. [Google Scholar] [CrossRef] [PubMed]
- Kroumpouzos, G. Effects of 5-alpha reductase inhibitors on lung function: A reason for discontinuation during COVID-19 pandemic? Dermatol. Ther. 2020, 33, e13535. [Google Scholar] [CrossRef] [PubMed]
- Lazzeri, M.; Duga, S.; Azzolini, E.; Fasulo, V.; Buffi, N.; Saita, A.; et al. The Humanitas Gavazzeni COVID-19 Task Force. Impact of chronic exposure to 5-alpha reductase inhibitors on the risk of hospitalization for COVID-19: A case-control study in male population from two COVID-19 regional centers of Lombardy (Italy). Minerva Urol. Nefrol. 2021. [Google Scholar] [CrossRef]
- Staedtke, V.; Bai, R.; Kim, K.; Darvas, M.; Davila, M.L.; Riggins, G.J.; et al. Disruption of a self-amplifying catecholamine loop reduces cytokine release syndrome. Nature 2018, 564, 273–277. [Google Scholar] [CrossRef]
- Nishimura, A. Alpha-1 blockers and susceptibility to COVID-19 in benign prostate hyperplasia patients: An international cohort study. medRxiv 2021. [Google Scholar] [CrossRef]
- Dinh, D.T.; Frauman, A.G.; Somers, G.R.; Ohishi, M.; Zhou, J.; Casley, D.J.; et al. Evidence for activation of the renin-angiotensin system in the human prostate: Increased angiotensin II and reduced AT(1) receptor expression in benign prostatic hyperplasia. J. Pathol. 2002, 196, 213–219. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Zhong, L.; Deng, J.; Peng, J.; Dan, H.; Zeng, X.; et al. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int J Oral Sci. 2020, 12, 8. [Google Scholar] [CrossRef] [PubMed]
- Alonso-Magdalena, P.; Brössner, C.; Reiner, A.; Cheng, G.; Sugiyama, N.; Warner, M.; et al. A role for epithelial-mesenchymal transition in the etiology of benign prostatic hyperplasia. Proc. Natl. Acad. Sci. USA 2009, 106, 2859–2863. [Google Scholar] [CrossRef] [PubMed]
- Wambier, C.G.; Goren, A. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection is likely to be androgen mediated. J. Am. Acad. Dermatol. 2020, 83, 308–309. [Google Scholar] [CrossRef]
- Lamy, P.J.; Rébillard, X.; Vacherot, F.; de la Taille, A. Androgenic hormones and the excess male mortality observed in COVID-19 patients: New convergent data. World J. Urol. 2020. [Google Scholar] [CrossRef]
- Breyer, B.N.; Sarma, A.V. Hyperglycemia and insulin resistance and the risk of BPH/LUTS: An update of recent literature. Curr. Urol. Rep. 2014, 15, 462. [Google Scholar] [CrossRef] [PubMed]
- DiBello, J.R.; Ioannou, C.; Rees, J.; Challacombe, B.; Maskell, J.; Choudhury, N.; et al. Prevalence of metabolic syndrome and its components among men with and without clinical benign prostatic hyperplasia: A large, cross-sectional, UK epidemiological study. BJU Int. 2016, 117, 801808. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.K.; Lin, S.S.; Ji, X.J.; Guo, L.M. Binding of SARS coronavirus to its receptor damages islets and causes acute diabetes. Acta Diabetol. 2010, 47, 193–199. [Google Scholar] [CrossRef] [PubMed]
- Higham, A.; Singh, D. Increased ACE2 expression in bronchial epithelium of COPD patients who are overweight. Obesity 2020, 28, 1586–1589. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ghoneim, S.; Butt, M.U.; Hamid, O.; Shah, A.; Asaad, I. The incidence of COVID-19 in patients with metabolic syndrome and non-alcoholic steatohepatitis: A population-based study. Metabol. Open. 2020, 8, 100057. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mehrotra, A.; Ray, K.; Brockmeyer, D.M.; Barnett, M.L.; Bender, J.A. Rapidly converting to “virtual practices”: Outpatient care in the era of COVID-19. NEJM Catal. 2020, 1, 1–5. [Google Scholar]
- Ohannessian, R.; Duong, T.A.; Odone, A. Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: A call to action. JMIR Public. Health Surveill. 2020, 6, e18810. [Google Scholar] [CrossRef] [PubMed]
- Smith, W.R.; Atala, A.J.; Terlecki, R.P.; Kelly, E.E.; Matthews, C.A. Implementation guide for rapid integration of an outpatient telemedicine program during the COVID-19 pandemic. J. Am. Coll. Surg. 2020, 231, 216–222. [Google Scholar] [CrossRef] [PubMed]
- Morselli, S.; Liaci, A.; Nicoletti, R.; Pecoraro, A.; Gemma, L.; Polverino, P.; et al. The use of a novel smartphone app for monitoring male LUTS treatment during the COVID-19 outbreak. Prostate Cancer Prostatic Dis. 2020, 23, 724–726. [Google Scholar] [CrossRef]
- Amparore, D.; Campi, R.; Checcucci, E.; Sessa, F.; Pecoraro, A.; Minervini, A.; et al. Forecasting the future of urology practice: A comprehensive review of the recommendations by international and European associations on priority procedures during the COVID-19 pandemic. Eur. Urol. Focus. 2020, 6, 1032–1048. [Google Scholar] [CrossRef]
- O’Flynn, K.; McGrath, J.; Harrison, S. A Framework for Re-Establishing and Developing Urology Services in the COVID-19 Era. NHS GIRFT. 2020. Available online: https://gettingitrightfirsttime.co.uk/wp-content/ uploads/2017/07/A-framework-for-reestablishing-and-developingurology-services-v1.0-4-Sept-2020.pdf (accessed on 25 June 2021).
- Raheem, A.A.; Ghazwani, Y.; Alowidah, I.; Azhar, R.A.; Alomar, M.; Alzahrani, A.; et al. Impact of COVID-19 on endourology surgical practice in Saudi Arabia: A national multicenter study. Asian J. Urol. 2021. [Google Scholar] [CrossRef] [PubMed]
- Alva Pinto, A.M.; González, M.S. Endourology and benign prostatic hyperplasia in COVID-19 pandemic. Int. Braz. J. Urol. 2020, 46 (S1), 34–38. [Google Scholar] [CrossRef]
- Stensland, K.D.; Morgan, T.M.; Moinzadeh, A.; Lee, C.T.; Briganti, A.; Catto, J.W.F.; et al. Considerations in the triage of urologic surgeries during the COVID-19 pandemic. Eur. Urol. 2020, 77, 663–666. [Google Scholar] [CrossRef] [PubMed]
- Ribal, M.J.; Cornford, P.; Briganti, A.; Knoll, T.; Gravas, S.; Babjuk, M.; et al. European Association of Urology Guidelines Office Rapid Reaction Group: An Organisation-wide Collaborative Effort to Adapt the European Association of Urology Guidelines Recommendations to the Coronavirus Disease 2019 Era. Eur Urol. 2020, 78, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Topaktaş, R.; Tokuç, E.; Ali Kutluhan, M.; Akyüz, M.; Karabay, E.; Çalışkan, S. Clinical features and outcomes of COVID-19 patients with benign prostatic hyperplasia in ageing male: A retrospective study of 18 cases. Int. J. Clin. Pract. 2020, 74, e13574. [Google Scholar] [CrossRef]
- Desouky, E. Urological surgery in the COVID-19 era: Patient counselling and informed consent. Arab. J. Urol. 2020, 18, 62–64. [Google Scholar] [CrossRef] [PubMed]
- Jin, P.; Park, H.; Jung, S.; Kim, J. Challenges in urology during the COVID-19 Pandemic. Urol. Int. 2021, 163–164. [Google Scholar] [CrossRef] [PubMed]
- USANZ. Personal Protection Equipment (PPE) for Urologists During COVID-19 Pandemic Pol 021. 2020. Available online: https://usanz.org.au/publicassets/efe71965-b773-ea11-90fb-0050568796d8/Pol-021Guidelines---PPE-for-Urologists-During-COVID-19-FINAL-310320.pdf.
- Desouky, E. Impact of COVID-19 on urologists: Learning on the go. Eur. Urol. Focus. 2020, 1132–1134. [Google Scholar] [CrossRef]
- Feng, D.; Liu, S.; Bai, Y.; Tang, Y.; Han, P.; Wei, W. Management of urology during COVID-19 pandemic: A perspective from Sichuan Province, China. Int. J. Surg. 2020, 115–121. [Google Scholar] [CrossRef]
- Nicolle, L.E. Catheter associated urinary tract infections. Antimicrob. Resist. Infect. Control 2014, 3, 23. [Google Scholar] [CrossRef]
- Kang, M.S.; Lee, B.S.; Lee, H.J.; Hwang, S.W.; Han, Z.A. Prevalence of and risk factors for multidrug-resistant bacteria in urine cultures of spinal cord injury patients. Ann. Rehabil. Med. 2015, 39, 686–695. [Google Scholar] [CrossRef]
- NICE. The technology | UroShield for preventing catheter-associated urinary tract infections (MIB191). NICE, 2019. [Google Scholar]
- Bactiguard Holding. Health Canada provides COVID-19 Interim Order approval for Bactiguard’s TempSensor catheter [Internet]. Cision PR Newswire. 2021. Available online: https://www.prnewswire.com/news-releases/health-canada-provides-covid-19-interim-order-approval-for-bactiguards-tempsensor-catheter-301224598.html (accessed on 24 June 2021).
- Lederer, J.W.; Jarvis, W.R.; Thomas, L.; Ritter, J. Multicenter cohort study to assess the impact of a silver-alloy and hydrogel-coated urinary catheter on symptomatic catheter-associated urinary tract infections. J. Wound Ostomy Continence Nurs. 2014, 41, 473–480. [Google Scholar] [CrossRef] [PubMed]
- Park, S.; Ryu, J.M.; Lee, M. Quality of life in older adults with benign prostatic hyperplasia. Healthcare 2020, 8, 158. [Google Scholar] [CrossRef] [PubMed]
- Nepogodiev, D.; Omar, O.M.; Glasbey, J.C.; Li, E.; Simoes, J.F.F.; Abbott, T.E.F.; et al. Elective surgery cancellations due to the COVID-19 pandemic: Global predictive modelling to inform surgical recovery plans. Br. J. Surg. 2020, 107, 1440–1449. [Google Scholar]
- Li, Z.; Jiang, Y.; Yu, Y.; Kang, Q. Effect of covid-19 pandemic on diagnosis and treatment delays in urological disease: Single-institution experience. Risk Manag. Healthc. Policy 2021, 14, 895–900. [Google Scholar] [CrossRef]
- Buyungo, J.; Quraishi, M.K.; Ewen, N.; Garnett, S. 137 Early findings of ward to clinic based TWOC model in post TURP patients. A possible effective model in COVID era. 2020, pp. A52.1–A52. Available online: http:// bmjleader.bmj.com/ (accessed on 21 June 2021).
- NICE. UroLift for treating lower urinary tract symptoms of benign prostatic hyperplasia MTG 58. 2021. Available online: www.nice.org.uk/ guidance/mtg58 (accessed on 20 June 2021).
- Weber, R.E. State telemedicine rules relaxed during COVID-19 crisis. Urology Times. 29 April 2020. Available online: https://www.urologytimes. com/view/state-telemedicine-rules-relaxed-during-covid-19-crisis (accessed on 25 June 2021).
- Lacktman, N.; Acosta, J.; Levine, S. 50-State Survey of Telehealth Commercial Payer Statutes. Foley & Lardner LLP. 2019. Available online: https://www.foley.com/-/media/files/insights/health-care-lawtoday/19mc21486-50state-survey-of-telehealth-commercial.pdf.
- Clinical Trials Arena. Change in reimbursement policies increases telemedicine demand [Internet]. 2021. Available online: https://www. clinicaltrialsarena.com/surveys/change-in-reimbursement-policiesincreases-telemedicine-demand-in-europe-amid-covid-19/ (accessed on 25 June 2021).
- Benign Prostatic Hyperplasia (BPH) Treatment Devices and Equipment Global Market Report 2021: COVID-19 Impact And Recovery To 2030. Market Analysi. 2021. Available online: https://www.reportlinker.com/ p06097021/Benign-Prostatic-Hyperplasia-BPH-Treatment-DevicesAnd-Equipment-Global-Market-Report-COVID-19-Impact-AndRecovery-To.html?utm_source=GNW (accessed on 25 June 2021).
- Ahmed, M.E.; Andrews, J.R.; Joshi, V.B.; Mynderse, L.A.; Tollefson, M.K.; Karnes, R.J.; et al. Patient satisfaction of telemedicine visits in an advanced prostate cancer clinic during the COVID-19 pandemic. Mayo Clin. Proc. Innov. Qual. Outcomes 2021, 5, 689–692. [Google Scholar] [CrossRef]
- Chugtai, B.; Cutone, B.; Alshak, M.; Mafilios, M.; Battacharya, S.; Elterman, D. The impact of COVID-19 on the management of BPH: How do we manage the backlog? J. Qual. Healthcare Ecol. 2020, 3, e1–e3. [Google Scholar] [CrossRef]
- Dubin, J.M.; Wyant, W.A.; Balaji, N.C.; Ong, W.L.K.; Kettache, R.H.; Haffaf, M.; et al. Telemedicine usage among urologists during the COVID-19 pandemic: Cross-sectional study. J. Med. Internet Res. 2020, 22, e21875. [Google Scholar] [CrossRef] [PubMed]
- Novara, G.; Checcucci, E.; Crestani, A.; Abrate, A.; Esperto, F.; Pavan, N.; et al. Telehealth in urology: A systematic review of the literature. how much can telemedicine be useful during and after the COVID-19 Pandemic?”. Eur. Urol. 2020, 78, 786–811. [Google Scholar] [CrossRef]
- Hameed, B.Z.; Tanidir, Y.; Naik, N.; Teoh, J.Y.C.; Shah, M.; Wroclawski, M.L.; et al. Will “hybrid” meetings replace face-to-face meetings post COVID-19 era? Perceptions and views from the urological community. Urology 2021. [Google Scholar] [CrossRef]
- Rosen, G.H.; Murray, K.S.; Greene, K.L.; Pruthi, R.S.; Richstone, L.; Mirza, M. Effect of COVID-19 on urology residency training: A nationwide survey of program directors by the Society of Academic Urologists. J. Urol. 2020, 204, 1039–1045. [Google Scholar] [CrossRef] [PubMed]
- Fero, K.E.; Weinberger, J.M.; Lerman, S.; Bergman, J. Perceived impact of urologic surgery training program modifications due to COVID-19 in the United States. Urology 2020, 143, 62–67. [Google Scholar] [CrossRef] [PubMed]
- Smigelski, M.; Movassaghi, M.; Small, A. Urology virtual education programs during the COVID-19 pandemic. Curr. Urol. Rep. 2020, 21, 50. [Google Scholar] [CrossRef] [PubMed]
This is an open access article under the terms of a license that permits non-commercial use, provided the original work is properly cited. © 2021 The Authors. Société Internationale d'Urologie Journal, published by the Société Internationale d'Urologie, Canada.