Association of Age with Lower Urinary Tract Function in Adult Men Presenting for Urodynamics: A Database Analysis
Abstract
Introduction
Material and Methods
Results
Discussion
Conclusions
Conflicts of Interest
Abbreviations
| BCI | bladder contractility index |
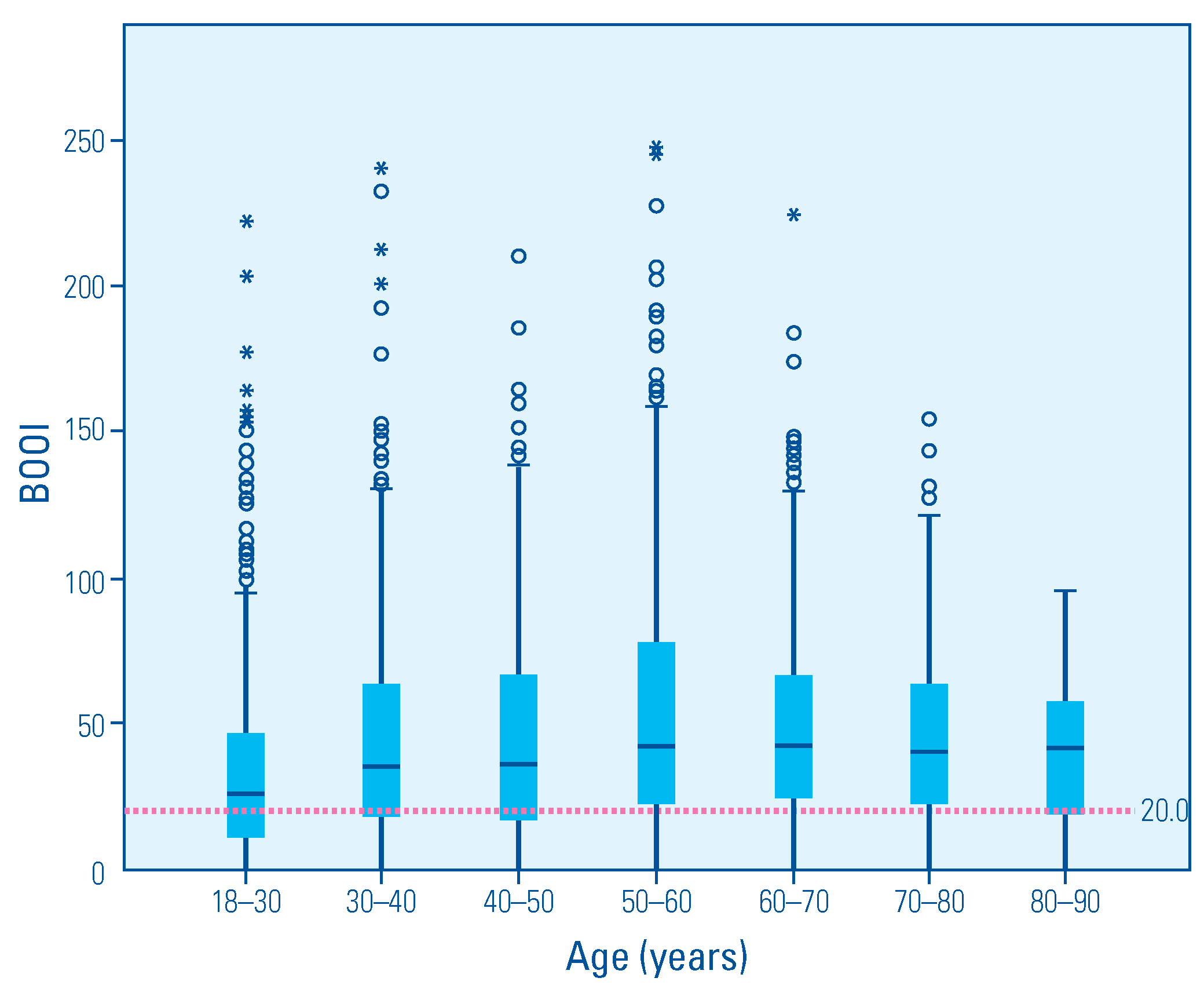
| BOOI | bladder outlet obstruction index |
| CI | confidence interval |
| IQR | interquartile range |
| OR | odds ratio |
| PVR | post-void residual |
References
- Vahabi, B.; Wagg, A.S.; Rosier, P.F.W.M.; Rademakers, K.L.J.; Denys, M.-A.; Pontari, M.; et al. Can we define and characterize the aging lower urinary tract?—ICI-RS 2015. Neurourol Urodyn. 2017, 36, 854–858. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zhong, P.; Zhao, Y.R.; Qiao, B.M.; Yang, F.-J.; Zhu, Y.; Yang, Z.-Q.; et al. Comparison of two numerical parameters to assess detrusor contractility in prognosing short-term outcome after transurethral resection of the prostate. Urol Int. 2020, 104, 361–366. [Google Scholar] [CrossRef] [PubMed]
- Antunes, A.A.; Iscaife, A.; Reis, S.T.; Albertini, A.; Nunes, M.A.; Lucon, A.M.; et al. Can we predict which patients will experience resolution of detrusor overactivity after transurethral resection of the prostate? J Urol. 2015, 193, 2028–2032. [Google Scholar] [CrossRef] [PubMed]
- Gravas, S.; Cornu, J.N.; Gacci, C.; Gratzke, C.; Herrmann, T.R.W.; Mamoulakis, C.; et al. Managment of non-neurogenic male lower urinary tract symptoms. European Association of Urology Guidelines, 2020. Available online: https://uroweb.org/guideline/treatment-of-non-neurogenic-male-luts (accessed on 15 December 2020).
- Rosier, P.F.W.M.; Schaefer, W.; Lose, G.; Goldman, H.B.; Guralnick, M.; Eustice, S.; et al. International continence society good urodynamic practices and terms 2016: Urodynamics, uroflowmetry, cystometry, and pressure-flow study. Neurourol Urodyn. 2017, 36, 1243–1260. [Google Scholar] [CrossRef] [PubMed]
- Abrams, P. Bladder outlet obstruction index, bladder contractility index and bladder voiding efficiency: Three simple indices to define bladder voiding function. BJU Int. 1999, 84, 14–15. [Google Scholar] [CrossRef] [PubMed]
- Jeong, S.J.; Lee, J.K.; Kim, K.M.; Kook, H.; Cho, S.Y.; Oh, S.-J. How do we diagnose detrusor underactivity? Comparison of diagnostic criteria based on an urodynamic measure. Investig Clin Urol. 2017, 58, 247–254. [Google Scholar] [CrossRef] [PubMed]
- Namitome, R.; Takei, M.; Takahashi, R.; Kikutake, C.; Yokomizo, A.; Yamaguchi, O.; et al. A prediction model of detrusor underactivity based on symptoms and noninvasive test parameters in men with lower urinary tract symptoms: An analysis of a large group of patients undergoing pressure-flow studies. J Urol. 2020, 203, 779–785. [Google Scholar] [CrossRef] [PubMed]
- Oelke, M.; Rademakers, K.L.J.; van Koeveringe, G.A. Unravelling detrusor underactivity: Development of a bladder outlet resistance—Bladder contractility nomogram for adult male patients with lower urinary tract symptoms. Neurourol Urodyn. 2016, 35, 980–986. [Google Scholar] [CrossRef]
- Jeong, S.J.; Kim, H.J.; Lee, Y.J.; Lee, J.K.; Lee, B.K.; Choo, Y.M.; et al. Prevalence and clinical features of detrusor underactivity among elderly with lower urinary tract symptoms: A comparison between men and women. Korean J Urol. 2012, 53, 342–348. [Google Scholar] [CrossRef]
- Beltrame, F.; Ferreira, F.T.; Lorenzetti, F.; Dambros, M.; Bisogni, S.; Dambros, M. Bladder function in obstructed men—Does age matter? Aging Male. 2015, 18, 143–148. [Google Scholar] [CrossRef]
- Rosier, P.F.W.M.; Ten Donkelaar, C.S.; de Kort, L.M.O. Clinical epidemiology: Detrusor voiding contraction maximum power, related to ageing. Urology. 2019, 124, 72–77. [Google Scholar] [CrossRef]
- Madersbacher, S.; Pycha, A.; Klingler, C.H.; Mian, C.; Djavan, B.; Stulnig, T.; et al. Interrelationships of bladder compliance with age, detrusor instability, and obstruction in elderly men with lower urinary tract symptoms. Neurourol Urodyn. 1999, 18, 3–15. [Google Scholar] [CrossRef]
- Bellucci, C.H.S.; Ribeiro, W.d.O.; de Bessa, J., Jr.; Antunes, A.A.; Leite, K.M.R.; et al. Increased detrusor collagen is associated with detrusor overactivity and decreased bladder compliance in men with benign prostatic obstruction. Prostate Int. 2017, 5, 70–74. [Google Scholar] [CrossRef]
- Oelke, M.; Baard, J.; Wijkstra, H.; de la Rosette, J.J.; Jonas, U.; Höfner, K. Age and bladder outlet obstruction are independently associated with detrusor overactivity in patients with benign prostatic hyperplasia. Eur Urol. 2008, 54, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Nitti, V.W.; Lefkowitz, G.; Ficazzola, M.; Dixon, C.M. Lower urinary tract symptoms in young men: Videourodynamic findings and correlation with noninvasive measures. J Urol. 2002, 168, 135–138. [Google Scholar] [CrossRef]
- Kaplan, S.A.; Ikeguchi, E.F.; Santarosa, R.P.; D’Alisera, P.M.; Hendricks, J.; Te, A.E.; et al. Etiology of voiding dysfunction in men less than 50 years of age. Urology. 1996, 47, 836–839. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.C.; Yang, S.S.D.; Chen, Y.T.; Hsieh, J.H. Videourodynamics identifies the causes of young men with lower urinary tract symptoms and low uroflow. Eur Urol. 2003, 43, 386–390. [Google Scholar] [CrossRef]
- Drake, M.J.; Lewis, A.L.; Young, G.J.; Abrams, P.; Blair, P.S.; Chapple, C.; et al. Diagnostic assessment of lower urinary tract symptoms in men considering prostate surgery: A noninferiority randomised controlled trial of urodynamics in 26 hospitals. Eur Urol. 2020, 78, 701–710. [Google Scholar] [CrossRef]
- Sinha, S.; Matai, L. Is isolated bladder outlet obstruction associated with hydronephrosis? A database analysis. Neurourol Urodyn. 2020, 39, 2361–2367. [Google Scholar] [CrossRef]
- Chen, S.F.; Lee, C.L.; Kuo, H.C. Change of detrusor contractility in patients with and without bladder outlet obstruction at ten or more years of follow-up. Sci Rep. 2019, 9. [Google Scholar] [CrossRef]
- Thomas, A.W.; Cannon, A.; Bartleh, E.; Ellis-Jones, J.; Abrams, P. The natural history of lower urinary tract dysfunction in men: Minimum 10-year urodynamic follow-up of untreated detrusor underactivity. BJU Int. 2005, 96, 1295–1300. [Google Scholar] [CrossRef] [PubMed]
- Ding, Y.Y.; Lieu, P.K.; Choo, P.W.J. Is the bladder “an unreliable witness ” in elderly males with persistent lower urinary tract symptoms? Geriatr Nephrol Urol. 1997, 7, 17–21. [Google Scholar] [CrossRef] [PubMed]
- Karami, H.; Valipour, R.; Lotfi, B.; Mokhtarpour, H.; Razi, A. Urodynamic findings in young men with chronic lower urinary tract symptoms. Neurourol Urodyn. 2011, 30, 1580–1585. [Google Scholar] [CrossRef]
- Jamzadeh, A.E.; Xie, D.; Laudano, M.; Seklehner, S.; Elterman, D.S.; Shtromvaser, L.; et al. Urodynamic characterization of lower urinary tract symptoms in men less than 40 years of age. World J Urol. 2014, 32, 469–473. [Google Scholar] [CrossRef] [PubMed]


 |
 |
This is an open access article under the terms of a license that permits non-commercial use, provided the original work is properly cited. © 2021 The Authors. Société Internationale d'Urologie Journal, published by the Société Internationale d'Urologie, Canada.
Share and Cite
Sinha, S.; Matai, L. Association of Age with Lower Urinary Tract Function in Adult Men Presenting for Urodynamics: A Database Analysis. Soc. Int. Urol. J. 2021, 2, 274-281. https://doi.org/10.48083/LQXF2741
Sinha S, Matai L. Association of Age with Lower Urinary Tract Function in Adult Men Presenting for Urodynamics: A Database Analysis. Société Internationale d’Urologie Journal. 2021; 2(5):274-281. https://doi.org/10.48083/LQXF2741
Chicago/Turabian StyleSinha, Sanjay, and Lavina Matai. 2021. "Association of Age with Lower Urinary Tract Function in Adult Men Presenting for Urodynamics: A Database Analysis" Société Internationale d’Urologie Journal 2, no. 5: 274-281. https://doi.org/10.48083/LQXF2741
APA StyleSinha, S., & Matai, L. (2021). Association of Age with Lower Urinary Tract Function in Adult Men Presenting for Urodynamics: A Database Analysis. Société Internationale d’Urologie Journal, 2(5), 274-281. https://doi.org/10.48083/LQXF2741




