B2B: Prostate Cancer Summary
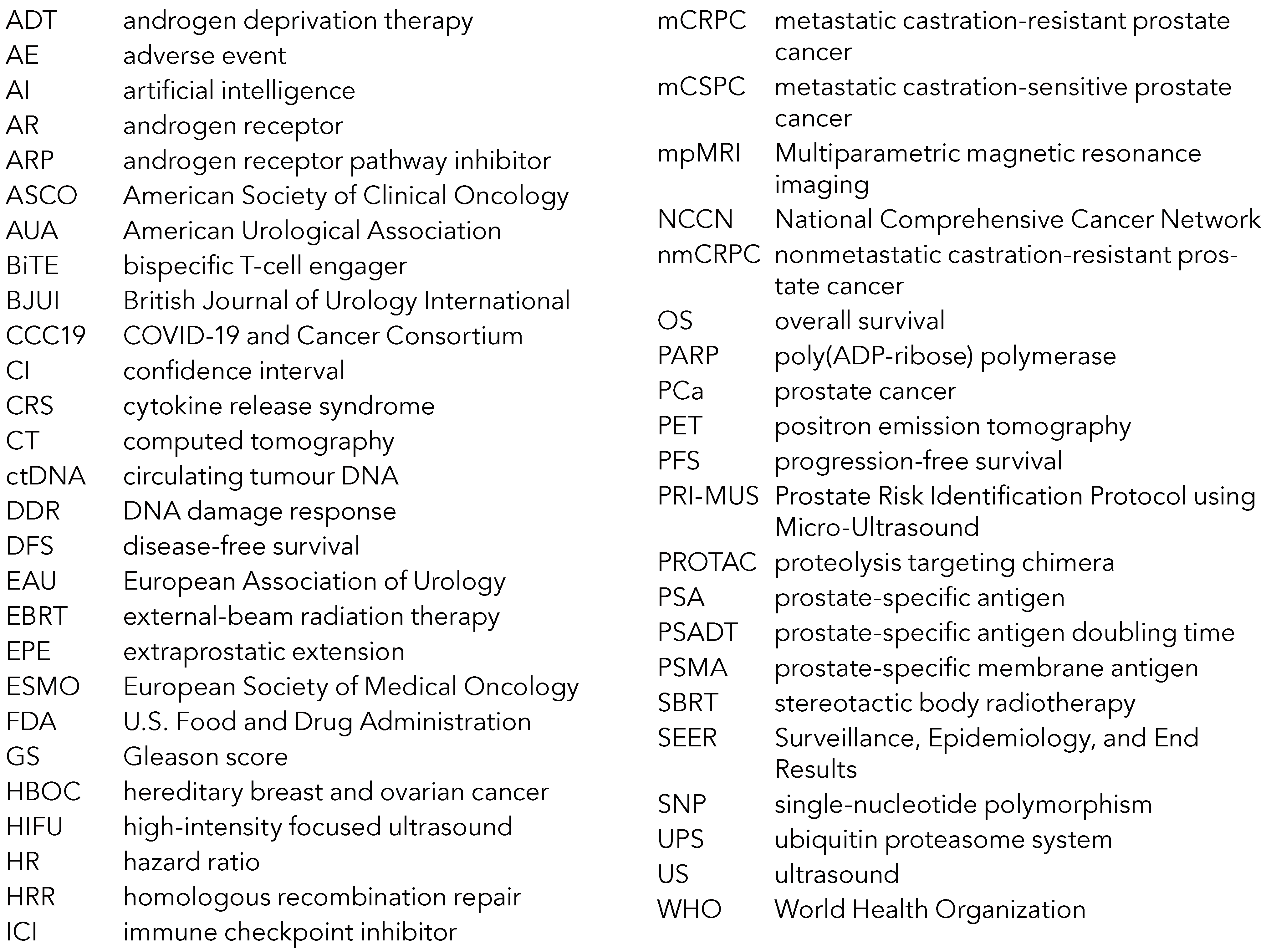
Abbreviations Used in the Text
References
- Vandekerkhove G, Wyatt A. Circulating tumour DNA as a biomarker source in metastatic prostate cancer. Société Internationale d’Urologie Journal 2020, 1, 39–48. [Google Scholar] [CrossRef]
- Annala M, Vandekerkhove G, Khalaf D, et al. Circulating tumor DNA genomics correlate with resistance to abiraterone and enzalutamide in prostate cancer. Cancer Discovery 2018, 8, 444–457. [Google Scholar] [CrossRef] [PubMed]
- Annala M, Fu S, Bacon JVW, et al. Cabazitaxel versus abiraterone or enzalutamide in poor prognosis metastatic castration-resistant prostate cancer: a multicentre, randomised, open-label, phase II trial. Annals of Oncology 2021, 32, 896–905. [Google Scholar] [CrossRef] [PubMed]
- Vandekerkhove G, Struss WJ, Annala M, et al. Circulating tumor DNA abundance and potential utility in de novo metastatic prostate cancer. European Urology 2019, 75, 667–675. [Google Scholar] [CrossRef] [PubMed]
- PROstate Cancer TReatment optimization via analysis of circulating tumour DNA. Accessed June 6, 2021. https://clinicaltrials.gov/ct2/show/NCT04015622.
- Wyatt AW, Annala M, Aggarwal R, et al. Concordance of circulating tumor DNA and matched metastatic tissue biopsy in prostate cancer. Journal of the National Cancer Institute 2017, 109, djx118. [Google Scholar] [CrossRef]
- Abida W, Campbell D, Shapiro J, et al. Clinical activity of rucaparib in patients with metastatic castration- resistant prostate cancer (mCRPC) and BRCA1 or BRCA2 mutation identified by FoundationOne® Liquid CDx (F1L CDx). In: 27th Annual PCF Scientific Retreat; 2020.
- Warner E, Herberts C, Fu S, et al. BRCA2, ATM, and CDK12 defects differentially shape prostate tumor driver genomics and clinical aggression. Clinical Cancer Research 2021, 27, 1650–1662. [Google Scholar] [CrossRef]
- Conteduca V, Jayaram A, Romero-Laorden N, et al. Plasma androgen receptor and docetaxel for metastatic castration-resistant prostate cancer. European Urology 2019, 75, 368–373. [Google Scholar] [CrossRef]
- Prostate cancer biomarker enrichment and treatment selection. Accessed June 6, 2021. https://clinicaltrials. gov/ct2/show/NCT03385655.
- Annala M, Taavitsainen S, Khalaf DJ, et al. Evolution of castration-resistant prostate cancer in ctDNA during sequential androgen receptor pathway inhibition. Clinical Cancer Research. Published online June 3, 2021:clincanres.CCR-21-1625-E.2021. [CrossRef]
- Mokdad AH, Dwyer-Lindgren L, Fitzmaurice C, et al. Trends and patterns of disparities in cancer mortality among US counties, 1980-2014. JAMA 2017, 317, 388–406. [Google Scholar] [CrossRef]
- U.S. Census Bureau QuickFacts: United States. Accessed June 3, 2021. https://www.census.gov/quickfacts/fact/table/US/RHI225219#RHI225219.
- Surveillance, Epidemiology, and End Results (SEER). Prostate Cancer; 2021. Accessed June 3, 2021. https://seer.cancer.gov/statfacts/html/prost.html.
- Kelly SP, Rosenberg PS, Anderson WF, et al. Trends in the incidence of fatal prostate cancer in the United States by race. European Urology 2017, 71, 195–201. [Google Scholar] [CrossRef]
- Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Cancer Journal for Clinicians 2018, 68, 394–424. [Google Scholar] [CrossRef]
- Tsodikov A, Gulati R, de Carvalho TM, et al. Is prostate cancer different in black men? Answers from 3 natural history models. Cancer 2017, 123, 2312–2319. [Google Scholar] [CrossRef] [PubMed]
- Disparities in health and health care: 5 key questions and answers. Accessed June 3, 2021. https://www. kff.org/racial-equity-and-health-policy/issue-brief/disparities-in-health-and-health-care-5-key-question- and-answers/.
- Disparities in health and health care: 5 key questions and answers. Accessed June 3, 2021. https://www. kff.org/racial-equity-and-health-policy/issue-brief/disparities-in-health-and-health-care-5-key-question- and-answers/. [CrossRef]
- Shoag JE, Nyame YA, Gulati R, et al. Reconsidering the trade-offs of prostate cancer screening. New England Journal of Medicine 2020, 382, 2465–2468. [Google Scholar] [CrossRef] [PubMed]
- Nyame YA, Gulati R, Heijnsdijk EAM, et al. The impact of intensifying prostate cancer screening in black men: a model-based analysis. Journal of the National Cancer Institute. Published online May 8, 2021. [CrossRef]
- Etzioni R, Nyame YA. Prostate cancer screening guidelines for black men: spotlight on an empty stage. Journal of the National Cancer Institute 2021, 113, 650–651. [Google Scholar] [CrossRef] [PubMed]
- Kensler KH, Pernar CH, Mahal BA, et al. Racial and ethnic variation in PSA testing and prostate cancer incidence following the 2012 USPSTF recommendation. Journal of the National Cancer Institute 2020, 113, 719–726. [Google Scholar] [CrossRef]
- Dess RT, Hartman HE, Mahal BA, et al. Association of Black race with prostate cancer–specific and other- cause mortality. JAMA Oncology 2019, 5, 975–983. [Google Scholar] [CrossRef] [PubMed]
- Wilkins LJ, Tosoian JJ, Reichard CA, et al. Oncologic outcomes among Black and White men with grade group 4 or 5 (Gleason score 8-10) prostate cancer treated primarily by radical prostatectomy. Cancer 2021, 127, 1425–1431. [Google Scholar] [CrossRef] [PubMed]
- Friedlander DF, Trinh Q-D, Krasnova A, et al. Racial disparity in delivering definitive therapy for intermediate/high-risk localized prostate cancer: the impact of facility features and socioeconomic characteristics. European Urology 2018, 73, 445–451. [Google Scholar] [CrossRef] [PubMed]
- Rencsok EM, Bazzi LA, McKay RR, et al. Diversity of enrollment in prostate cancer clinical trials: current status and future directions. Cancer Epidemiology Biomarkers & Prevention 2020, 29, 1374–1380. [Google Scholar] [CrossRef]
- Washington H. Medical Apartheid: The Dark History of Medical Experimentation on Black Americans from Colonial Times to the Present. Penguin Random House; 2007.
- PCORI Engagement Rubric; 2014. Accessed June 3, 2021. http://www.pcori.org/sites/default/files/Engagement-Rubric.pdf.
- Crona DJ, Whang YE. Androgen receptor-dependent and -independent mechanisms involved in prostate cancer therapy resistance. Cancers 2017, 9, 67. [Google Scholar] [CrossRef]
- Petrylak DP, Gao X, Vogelzang NJ, et al. First-in-human phase I study of ARV-110, an androgen receptor (AR) PROTAC degrader in patients (pts) with metastatic castrate-resistant prostate cancer (mCRPC) following enzalutamide (ENZ) and/or abiraterone (ABI). Journal of Clinical Oncology 2020, 38(15_suppl):3500. [CrossRef]
- Mei L, Zhang J, He K, et al. Ataxia telangiectasia and Rad3-related inhibitors and cancer therapy: where we stand. Journal of Hematology and Oncology 2019, 12, 1–8. [Google Scholar] [CrossRef]
- Duan R, Du W, Guo W. EZH2: a novel target for cancer treatment. Journal of Hematology and Oncology 2020, 13, 1–12. [Google Scholar] [CrossRef]
- de Bono JS, Sweeney C, Bracarda S, et al. PI3K/AKT pathway biomarkers analysis from the phase III IPATential150 trial of ipatasertib plus abiraterone in metastatic castration-resistant prostate cancer. Journal of Clinical Oncology 2021, 39(6_suppl):13. [CrossRef]
- Baeuerle PA, Reinhardt C. Bispecific T-cell engaging antibodies for cancer therapy. Cancer Research 2009, 69, 4941–4944. [Google Scholar] [CrossRef] [PubMed]
- Tran B, Horvath L, Dorff T, et al. Results from a phase I study of AMG 160, a half-life extended (HLE), PSMA- targeted, bispecific T-cell engager (BiTE®) immune therapy for metastatic castration-resistant prostate cancer (mCRPC). Annals of Oncology. [CrossRef]
- FDA approves first PSMA-targeted PET imaging drug for men with prostate cancer. Accessed June 6, 2021. https://www.fda.gov/news-events/press- announcements/fda-approves-first-psma-targeted- pet-imaging-drug-men-prostate-cancer.
- Morris MJ, Rowe SP, Gorin MA, et al. Diagnostic performance of 18 F-DCFPyL-PET/CT in men with biochemically recurrent prostate cancer: results from the CONDOR phase III, multicenter study. Clinical Cancer Research, 23 February 2021. [CrossRef]
- Pienta KJ, Gorin MA, Rowe SP, et al. A phase 2/3 prospective multicenter study of the diagnostic accuracy of prostate specific membrane antigen PET/CT with 18 F-DCFPyL in prostate cancer patients (OSPREY). Journal of Urology 2021, 206, 52–61. [Google Scholar] [CrossRef]
- Parker C, Nilsson S, Heinrich D, et al. Alpha emitter radium-223 and survival in metastatic prostate cancer. New England Journal of Medicine 2013, 369, 213–223. [Google Scholar] [CrossRef] [PubMed]
- Novartis announces positive result of phase III study with radioligand therapy 177Lu-PSMA-617 in patients with advanced prostate cancer | Novartis. Accessed June 6, 2021. https://www.novartis.com/news/media-releases/novartis-announces-positive-result- phase-iii-study-radioligand-therapy-177lu-psma-617- patients-advanced-prostate-cancer.
- Sartor AO, Morris MJ, Krause BJ, et al. VISION: an international, prospective, open-label, multicenter, randomized phase 3 study of 177 Lu-PSMA-617 in the treatment of patients with progressive PSMA-positive metastatic castration-resistant prostate cancer (mCRPC). Journal of Clinical Oncology 2019, 37(15_ suppl):TPS5099. [CrossRef]
- Asim M, Tarish F, Zecchini HI, et al. Synthetic lethality between androgen receptor signalling and the PARP pathway in prostate cancer. Nature Communications 2017, 8, 1–10. [Google Scholar] [CrossRef]
- Virtanen V, Paunu K, Ahlskog JK, et al. PARP inhibitors in prostate cancer—The preclinical rationale and current clinical development. Genes 2019, 10, 565. [Google Scholar] [CrossRef]
- Bossi A, Dearnaley D, McKenzie M, et al. ATLAS: a phase 3 trial evaluating the efficacy of apalutamide (ARN-509) in patients with high-risk localized or locally advanced prostate cancer receiving primary radiation therapy. Annals of Oncology 2016, 27:vi263. [CrossRef]
- Dalela D, Löppenberg B, Sood A, et al. Contemporary role of the Decipher® test in prostate cancer management: current practice and future perspectives. Reviews in Urology 2016, 18, 1–9. [Google Scholar]
- Kneebone A, Fraser-Browne C, Duchesne GM, et al. Adjuvant radiotherapy versus early salvage radiotherapy following radical prostatectomy ( TROG 08.03/ANZUP RAVES): a randomised, controlled, phase 3, non-inferiority trial. The Lancet Oncology 2020, 21, 1331–1340. [Google Scholar] [CrossRef]
- Sargos P, Chabaud S, Latorzeff I, et al. Adjuvant radiotherapy versus early salvage radiotherapy plus short-term androgen deprivation therapy in men with localised prostate cancer after radical prostatectomy (GETUG-AFU 17): a randomised, phase 3 trial. The Lancet Oncology 2020, 21, 1341–1352. [Google Scholar] [CrossRef]
- Parker CC, Clarke NW, Cook AD, et al. Timing of radiotherapy after radical prostatectomy (RADICALS- RT): a randomised, controlled phase 3 trial. The Lancet 2020, 396, 1413–1421. [Google Scholar] [CrossRef]
- Den RB, Yousefi K, Trabulsi EJ, et al. Genomic classifier identifies men with adverse pathology after radical prostatectomy who benefit from adjuvant radiation therapy. Journal of Clinical Oncology 2015, 33, 944–951. [Google Scholar] [CrossRef]
- Zhao SG, Chang SL, Spratt DE, et al. Development and validation of a 24-gene predictor of response to postoperative radiotherapy in prostate cancer: a matched, retrospective analysis. The Lancet Oncology 2016, 17, 1612–1620. [Google Scholar] [CrossRef] [PubMed]
- Vale CL, Fisher D, Kneebone A, et al. Adjuvant or early salvage radiotherapy for the treatment of localised and locally advanced prostate cancer: a prospectively planned systematic review and meta-analysis of aggregate data. The Lancet 2020, 396, 1422–1431. [Google Scholar] [CrossRef]
- Loeb S, Giri VN. Clinical implications of germline testing in newly diagnosed prostate cancer. European Urology Oncology 2021, 4, 1–9. [Google Scholar] [CrossRef]
- Giri VN, Knudsen KE, Kelly WK, et al. Implementation of germline testing for prostate cancer: Philadelphia Prostate Cancer Consensus Conference 2019. Journal of Clinical Oncology 2020, 38, 2798–2811. [Google Scholar] [CrossRef]
- Abida W, Patnaik A, Campbell D, et al. Rucaparib in men with metastatic castration-resistant prostate cancer harboring a BRCA1 or BRCA2 gene alteration. Journal of Clinical Oncology 2020, 38, 3763–3772. [Google Scholar] [CrossRef]
- de Bono J, Mateo J, Fizazi K, et al. Olaparib for metastatic castration-resistant prostate cancer. New England Journal of Medicine 2020, 382, 2091–2102. [Google Scholar] [CrossRef] [PubMed]
- Antonarakis ES, Gomella LG, Petrylak DP. When and how to use PARP inhibitors in prostate cancer: a systematic review of the literature with an update on on-going trials. European Urology Oncology 2020, 3, 594–611. [Google Scholar] [CrossRef] [PubMed]
- Carter HB, Helfand B, Mamawala M, et al. Germline mutations in ATM and BRCA1/2 are associated with grade reclassification in men on active surveillance for prostate cancer. European Urology 2019, 75, 743–749. [Google Scholar] [CrossRef]
- Ribal MJ, Cornford P, Briganti A, et al. European Association of Urology guidelines office rapid reaction group: an organisation-wide collaborative effort to adapt the European Association of Urology guidelines recommendations to the coronavirus disease 2019 era. European Urology 2020, 78, 21–28. [Google Scholar] [CrossRef]
- Hanna TP, King WD, Thibodeau S, et al. Mortality due to cancer treatment delay: systematic review and meta- analysis. BMJ (Clinical Research Ed) 2020, 371:m4087. [CrossRef]
- Glasbey JC, Nepogodiev D, Simoes JFF, et al. Elective cancer surgery in COVID-19-free surgical pathways during the SARS-CoV-2 pandemic: an international, multicenter, comparative cohort study. Journal of Clinical Oncology 2021, 39, 66–78. [Google Scholar] [CrossRef]
- COVIDSurg Collaborative, GlobalSurg Collaborative. Timing of surgery following SARS-CoV-2 infection: an international prospective cohort study. Anaesthesia 2021, 76, 748–758. [Google Scholar] [CrossRef] [PubMed]
- Lee LYW, Cazier JB, Angelis V, et al. COVID-19 mortality in patients with cancer on chemotherapy or other anticancer treatments: a prospective cohort study. The Lancet 2020, 395, 1919–1926. [Google Scholar] [CrossRef] [PubMed]
- COVID-19 and Cancer Consortium Registry. Accessed June 6, 2021. https://clinicaltrials.gov/ct2/show/NCT04354701.
- ASCO Survey on COVID-19 in Oncology (ASCO) Registry. Accessed June 6, 2021. https://clinicaltrials.gov/ct2/show/NCT04659135?term=NCT04659135&draw= 2&rank=1.
- ESMO-CoCARE Registry. Accessed June 6, 2021. ht tps://w w w. esmo. org/covid-19 - and- c ancer/registries-studies-and-surveys/esmo-cocare-registry.
- COVID-19 vaccination in cancer patients: ESMO statements. Accessed June 6, 2021. https://www.esmo. org/covid-19-and-cancer/covid-19-vaccination.
- ASCO. COVID-19 vaccines & patients with cancer. Accessed June 6, 2021. https://www.asco.org/asco- coronavirus-resourcescovid-19-vaccines-patients- cancer.
- Vaccination Advisory Committee: Recommendations of the NCCN COVID-19. Accessed June 6, 2021. https://www.nccn.org/covid-19.
- COVIDSurg Collaborative, GlobalSurg Collaborative. SARS-CoV-2 vaccination modelling for safe surgery to save lives: data from an international prospective cohort study. British Journal of Surgery. Published online 2021:1-8. [CrossRef]
- Rodriguez Socarrás M, Loeb S, Teoh JYC, et al. Telemedicine and smart working: recommendations of the European Association of Urology. European Urology 2020, 78, 812–819. [Google Scholar] [CrossRef]
- Rodler S, Apfelbeck M, Schulz GB, et al. Telehealth in uro-oncology beyond the pandemic: toll or lifesaver? European Urology Focus 2020, 6, 1097–1103. [Google Scholar] [CrossRef]
- Wallis CJD, Catto JWF, Finelli A, et al. The impact of the COVID-19 pandemic on genitourinary cancer care: re-envisioning the future. European Urology 2020, 78, 731–742. [Google Scholar] [CrossRef]
- Hlubocky FJ, Symington BE, McFarland DC, et al. Impact of the COVID-19 pandemic on oncologist burnout, emotional well-being, and moral distress: considerations for the cancer organization’s response for readiness, mitigation, and resilience. JCO Oncology Practice. Published online February 8, 2021:1-11. [CrossRef]
- Maringe C, Spicer J, Morris M, et al. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. The Lancet Oncology 2020, 21, 1023–1034. [Google Scholar] [CrossRef] [PubMed]
- Oderda M, Roupret M, Marra G, et al. The impact of COVID-19 outbreak on uro-oncological practice across Europe: which burden of activity are we facing ahead? European Urology 2020, 78, 124–126. [Google Scholar] [CrossRef]
- Lughezzani G, Saita A, Lazzeri M, et al. Comparison of the diagnostic accuracy of micro-ultrasound and magnetic resonance imaging/ultrasound fusion targeted biopsies for the diagnosis of clinically significant prostate cancer. European Urology Oncology 2019, 2, 329–332. [Google Scholar] [CrossRef]
- Ghai S, Eure G, Fradet V, et al. Assessing cancer risk on novel 29 MHz micro-ultrasound images of the prostate: creation of the micro-ultrasound protocol for prostate risk identification. Journal of Urology 2016, 196, 562–569. [Google Scholar] [CrossRef]
- Abouassaly R, Klein EA, El-Shefai A, et al. Impact of using 29 MHz high-resolution micro-ultrasound in real- time targeting of transrectal prostate biopsies: initial experience. World Journal of Urology 2020, 38, 1201–1206. [Google Scholar] [CrossRef]
- Lughezzani G, Maffei D, Saita A, et al. Diagnostic accuracy of microultrasound in patients with a suspicion of prostate cancer at magnetic resonance imaging: a single-institutional prospective study. European Urology Focus 2020, S2405-4569, 30272-30278. [CrossRef]
- Klotz L, Lughezzani G, Maffei D, et al. Comparison of micro-ultrasound and multiparametric magnetic resonance imaging for prostate cancer: a multicenter, prospective analysis. Canadian Urological Association Journal 2020, 15, E11–E16. [Google Scholar] [CrossRef]
- Cornud F, Lefevre A, Flam T, et al. MRI-directed high- frequency (29MhZ) TRUS-guided biopsies: initial results of a single-center study. European Radiology 2020, 30, 4838–4846. [Google Scholar] [CrossRef] [PubMed]
- Claros OR, Tourinho-Barbosa RR, Fregeville A, et al. Comparison of initial experience with transrectal magnetic resonance imaging cognitive guided micro- ultrasound biopsies versus established transperineal robotic ultrasound magnetic resonance imaging fusion biopsies for prostate cancer. The Journal of Urology 2020, 203, 918–925. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez Socarrás ME, Gomez Rivas J, Cuadros Rivera V, et al. Prostate mapping for cancer diagnosis: the Madrid protocol. Transperineal prostate biopsies using multiparametric magnetic resonance imaging fusion and micro-ultrasound guided biopsies. The Journal of Urology 2020, 204, 726–733. [Google Scholar] [CrossRef] [PubMed]
- Wiemer L, Hollenbach M, Heckmann R, et al. Evolution of targeted prostate biopsy by adding microultrasound to the magnetic resonance imaging pathway. European Urology Focus 2020, S2405-4569(20)30188-7. [CrossRef]
- Regis F, Casale P, Persico F, et al. Use of 29-MHz micro-ultrasound for local staging of prostate cancer in patients scheduled for radical prostatectomy: a feasibility study. European Urology Open Science 2020, 19:20-23. [CrossRef]
- Stabile A, Orczyk C, Hosking-Jervis F, et al. Medium- term oncological outcomes in a large cohort of men treated with either focal or hemi-ablation using high- intensity focused ultrasonography for primary localized prostate cancer. BJU International 2019, 124, 431–440. [Google Scholar] [CrossRef]
- Donaldson IA, Alonzi R, Barratt D, et al. Focal therapy: patients, interventions, and outcomes - a report from a consensus meeting. European Urology 2015, 67, 771–777. [Google Scholar] [CrossRef]
- Rastinehad AR, Anastos H, Wajswol E, et al. Gold nanoshell-localized photothermal ablation of prostate tumors in a clinical pilot device study. Proceedings of the National Academy of Sciences of the United States of America 2019, 116, 18590–18596. [Google Scholar] [CrossRef]
- Maruf M, George A, Canfield S, et al. Phase II clinical trial: short-term oncologic outcomes of nanoparticle- directed focal photothermal laser ablation. Journal of Urology 2020, 203(Supplement 4):e373-e374. [CrossRef]
- Turkbey B, Pinto PA, Mani H, et al. Prostate cancer: value of multiparametric MR imaging at 3 T for detection - histopathologic correlation. Radiology 2010, 255, 89–99. [Google Scholar] [CrossRef]
- Valerio M, Cerantola Y, Eggener SE, et al. New and established technology in focal ablation of the prostate: a systematic review. European Urology 2017, 71, 17–34. [Google Scholar] [CrossRef]
- Mottet N, van den Bergh RCN, Briers E, et al. EAU-EANM-ESTRO-ESUR-SIOG guidelines on prostate cancer—2020 update. Part 1: screening, diagnosis, and local treatment with curative intent. European Urology 2021, 79, 243–262. [Google Scholar] [CrossRef] [PubMed]
- Kishan AU, Park SJ, King CR, et al. Dosimetric benefits of hemigland stereotactic body radiotherapy for prostate cancer: implications for focal therapy. British Journal of Radiology 2015, 88, 20150658. [Google Scholar] [CrossRef] [PubMed]
- Prada PJ, Cardenal J, García Blanco A, et al. Focal high-dose-rate brachytherapy for localized prostate cancer: toxicity and preliminary biochemical results. Strahlentherapie und Onkologie 2020, 196, 222–228. [Google Scholar] [CrossRef] [PubMed]
- Brand DH, Tree AC, Ostler P, et al. Intensity-modulated fractionated radiotherapy versus stereotactic body radiotherapy for prostate cancer (PACE-B): acute toxicity findings from an international, randomised, open-label, phase 3, non-inferiority trial. The Lancet Oncology 2019, 20 (11):1531-1543. [CrossRef]
- Tocco BR, Kishan AU, Ma TM, et al. MR-guided radiotherapy for prostate cancer. Frontiers in Oncology 2020, 10:2763. [CrossRef]
- Kerkmeijer LGW, Groen VH, Pos FJ, et al. Focal boost to the intraprostatic tumor in external beam radiotherapy for patients with localized prostate cancer: results from the FLAME randomized phase III trial. Journal of Clinical Oncology 2021, 39, 787–796. [Google Scholar] [CrossRef] [PubMed]
- Draulans C, van der Heide UA, Haustermans K, et al. Primary endpoint analysis of the multicentre phase II hypo-FLAME trial for intermediate and high risk prostate cancer. Radiotherapy and Oncology 2020, 147:92-98. [CrossRef]
- Connor MJ, Shah TT, Smigielska K, et al. Additional treatments to the local tumour for metastatic prostate cancer-assessment of novel treatment algorithms (IP2-ATLANTA): protocol for a multicentre, phase II randomised controlled trial. BMJ Open 2021, 11, 42953. [Google Scholar] [CrossRef]
- Fendler WP, Weber M, Iravani A, et al. Prostate- specific membrane antigen ligand positron emission tomography in men with nonmetastatic castration- resistant prostate cancer. Clinical Cancer Research 2019, 25, 7448–7454. [Google Scholar] [CrossRef] [PubMed]
- Howard LE, Moreira DM, de Hoedt A, et al. Thresholds for PSA doubling time in men with non-metastatic castration-resistant prostate cancer. BJU International 2017, 120(5B):E80-E86. [CrossRef]
- Fizazi K, Shore N, Tammela TL, et al. Darolutamide in nonmetastatic, castration-resistant prostate cancer. New England Journal of Medicine 2019, 380, 1235–1246. [Google Scholar] [CrossRef]
- Hussain M, Fizazi K, Saad F, et al. Enzalutamide in men with nonmetastatic, castration-resistant prostate cancer. New England Journal of Medicine 2018, 378, 2465–2474. [Google Scholar] [CrossRef]
- Smith MR, Saad F, Chowdhury S, et al. Apalutamide treatment and metastasis-free survival in prostate cancer. New England Journal of Medicine 2018, 378, 1408–1418. [Google Scholar] [CrossRef]
- Beauval J-B, Loriot Y, Hennequin C, et al. Loco- regional treatment for castration-resistant prostate cancer: is there any rationale? A critical review from the AFU-GETUG. Critical Reviews in Oncology/Hematology 2018, 122:144-149. [CrossRef]
- Parker C, Castro E, Fizazi K, et al. Prostate cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Annals of Oncology 2020, 31, 1119–1134. [Google Scholar] [CrossRef]
- Wyatt AW, Azad AA, Volik S v. , et al. Genomic alterations in cell-free DNA and enzalutamide resistance in castration-resistant prostate cancer. JAMA Oncology 2016, 2, 1598–1606. [Google Scholar] [CrossRef] [PubMed]
- Lallous N, Volik S v. , Awrey S, et al. Functional analysis of androgen receptor mutations that confer anti-androgen resistance identified in circulating cell-free DNA from prostate cancer patients. Genome Biology 2016, 17, 10. [Google Scholar] [CrossRef]
- Annala M, Struss WJ, Warner EW, et al. Treatment outcomes and tumor loss of heterozygosity in germline DNA repair–deficient prostate cancer. European Urology 2017, 72, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Hussain M, Mateo J, Fizazi K, et al. Survival with olaparib in metastatic castration-resistant prostate cancer. New England Journal of Medicine 2020, 383, 2345–2357. [Google Scholar] [CrossRef] [PubMed]
- de Wit R, de Bono J, Sternberg CN, et al. Cabazitaxel versus abiraterone or enzalutamide in metastatic prostate cancer. New England Journal of Medicine 2019, 381, 2506–2518. [CrossRef]
- Hofman MS, Emmett L, Sandhu S, et al. [177Lu] Lu-PSMA-617 versus cabazitaxel in patients with metastatic castration-resistant prostate cancer (TheraP): a randomised, open-label, phase 2 trial. The Lancet 2021, 397, 797–804. [CrossRef]
- Digital trends 2021. Accessed June 7, 2021. https://www. hootsuite.com/pages/digital-trends-2021.
- Statista. Where health app usage is most common. Accessed June 7, 2021. https://www.statista.com/chart/23161/health-app-usage-country-comparison/.
- Pereira-Azevedo N, Osório L, Fraga A, et al. Rotterdam Prostate Cancer Risk Calculator: development and usability testing of the mobile phone app. JMIR Cancer 2017, 3, e1. [Google Scholar] [CrossRef] [PubMed]
- National Cancer Grid. Virtual tumour board. Accessed June 7, 2021. https://tmc.gov.in/ncg/index.php/activities-ncg/vrtual-tumor-board.
- Gudaru K, Blanco LT, Castellani D, et al. Connecting the urological community: the #UroSoMe experience. Journal of Endoluminal Endourology 2019, 2, e21–e29. [Google Scholar] [CrossRef]
- Bhatt NR, Czarniecki SW, Borgmann H, et al. A systematic review of the use of social media for dissemination of clinical practice guidelines. European Urology Focus 2020, S2405 - 4569, 30292-30293. [CrossRef]
- Loeb S, Roupret M, van Oort I, et al. Novel use of Twitter to disseminate and evaluate adherence to clinical guidelines by the European Association of Urology. BJU International 2017, 119, 820–822. [Google Scholar] [CrossRef]
- Dubin JM, Wyant WA, Balaji NC, et al. Telemedicine usage among urologists during the COVID-19 pandemic: cross-sectional study. Journal of Medical Internet Research 2020, 22, e21875. [Google Scholar] [CrossRef]
- Rivas JG, Socarras MR, Patruno G, et al. Perceived role of social media in urologic knowledge acquisition among young urologists: a European survey. European Urology Focus 2018, 4, 768–773. [Google Scholar] [CrossRef] [PubMed]
- Dubin JM, Greer AB, Patel P, et al. Global survey of the roles and attitudes toward social media platforms amongst urology trainees. Urology 2021, 147:64-67. [CrossRef]
- Junwen S, Rongjiang W. The efficacy of the WeChat app combined with pelvic floor muscle exercise for the urinary incontinence after radical prostatectomy. BioMed Research International 2020, 2020:6947839. [CrossRef]
- Belarmino A, Walsh R, Alshak M, et al. Feasibility of a mobile health application to monitor recovery and patient-reported outcomes after robot-assisted radical prostatectomy. European Urology Oncology 2019, 2, 425–428. [Google Scholar] [CrossRef] [PubMed]
- Gebbia V, Piazza D, Valerio MR, et al. Patients with cancer and COVID-19: a WhatsApp messenger-based survey of patients’ queries, needs, fears, and actions taken. JCO Global Oncology 2020, (6). [CrossRef]
- Loeb S, Mihalcea R, Perez-Rosas V, et al. Leveraging social media as a thermometer to gauge patient and caregiver concerns: COVID-19 and prostate cancer. European Urology Open Science. [CrossRef]
- Alsyouf M, Stokes P, Hur D, et al. ‘Fake news’ in urology: evaluating the accuracy of articles shared on social media in genitourinary malignancies. BJU International 2019, 124, 701–706. [Google Scholar] [CrossRef] [PubMed]
- Loeb S, Reines K, Abu-Salha Y, et al. Quality of bladder cancer information on YouTube. European Urology 2021, 79, 56–59. [Google Scholar] [CrossRef] [PubMed]
- Loeb S, Sengupta S, Butaney M, et al. Dissemination of misinformative and biased information about prostate cancer on YouTube. European Urology 2019, 75, 564–567. [Google Scholar] [CrossRef] [PubMed]
- Xu AJ, Taylor J, Gao T, et al. TikTok and prostate cancer: misinformation and quality of information using validated questionnaires. BJU International. Published online April 2, 2021. [CrossRef]
- Charnock D, Shepperd S, Needham G, et al. DISCERN: an instrument for judging the quality of written consumer health information on treatment choices. Journal of Epidemiology and Community Health 1999, 53, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Pantanowitz L, Quiroga-Garza GM, Bien L, et al. An artificial intelligence algorithm for prostate cancer diagnosis in whole slide images of core needle biopsies: a blinded clinical validation and deployment study. The Lancet Digital Health 2020, 2, e407–e416. [Google Scholar] [CrossRef] [PubMed]
- PIONEER - European network of excellence for big data in prostate cancer. Accessed June 8, 2021. https://prostate-pioneer.eu/.
- Hoffer-Hawlik MA, Moran AE, Burka D, et al. Leveraging telemedicine for chronic disease management in low- and middle-income countries during Covid-19. Global Heart 2020, 15, 63. [Google Scholar] [CrossRef]
- Veneziano D, Tafuri A, Rivas JG, et al. Is remote live urologic surgery a reality? Evidences from a systematic review of the literature. World Journal of Urology 2020, 38, 2367–2376. [Google Scholar] [CrossRef]
This is an open access article under the terms of a license that permits non-commercial use, provided the original work is properly cited. © 2021 The Authors. Société Internationale d'Urologie Journal, published by the Société Internationale d'Urologie, Canada.
Share and Cite
Loeb, S.; Black, P.C.; Wyatt, A.W.; Nyame, Y.A.; Shore, N.; Tilki, D.; Castro, E.; Cooperberg, M.; Giri, V.; Ribal, M.J.; et al. B2B: Prostate Cancer Summary. Soc. Int. Urol. J. 2021, 2, 29-50. https://doi.org/10.48083/ZJLZ6285
Loeb S, Black PC, Wyatt AW, Nyame YA, Shore N, Tilki D, Castro E, Cooperberg M, Giri V, Ribal MJ, et al. B2B: Prostate Cancer Summary. Société Internationale d’Urologie Journal. 2021; 2(4):29-50. https://doi.org/10.48083/ZJLZ6285
Chicago/Turabian StyleLoeb, Stacy, Peter C. Black, Alexander W. Wyatt, Yaw A. Nyame, Neal Shore, Derya Tilki, Elena Castro, Matthew Cooperberg, Veda Giri, Maria J. Ribal, and et al. 2021. "B2B: Prostate Cancer Summary" Société Internationale d’Urologie Journal 2, no. 4: 29-50. https://doi.org/10.48083/ZJLZ6285
APA StyleLoeb, S., Black, P. C., Wyatt, A. W., Nyame, Y. A., Shore, N., Tilki, D., Castro, E., Cooperberg, M., Giri, V., Ribal, M. J., Lughezzani, G., Sánchez-Salas, R., Moore, C. M., Rastinehad, A., Kerkmeijer, L., Ahmed, H. U., Akamatsu, S., Taille, A. d. l., Gleave, M., & Tanguay, S. (2021). B2B: Prostate Cancer Summary. Société Internationale d’Urologie Journal, 2(4), 29-50. https://doi.org/10.48083/ZJLZ6285



