Does Type 1 Diabetes Affect Male Infertility: Type 1 Diabetes Exchange Registry-Based Analysis
Abstract
:Introduction
Materials and Methods
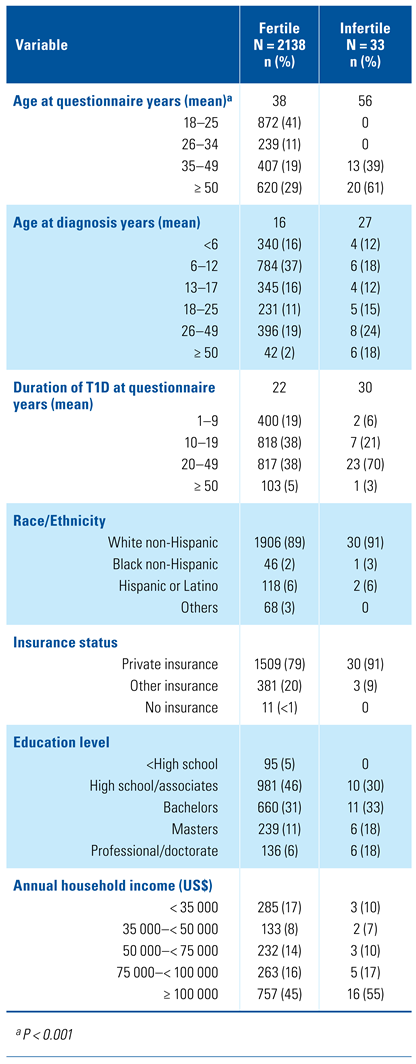
Study population and design
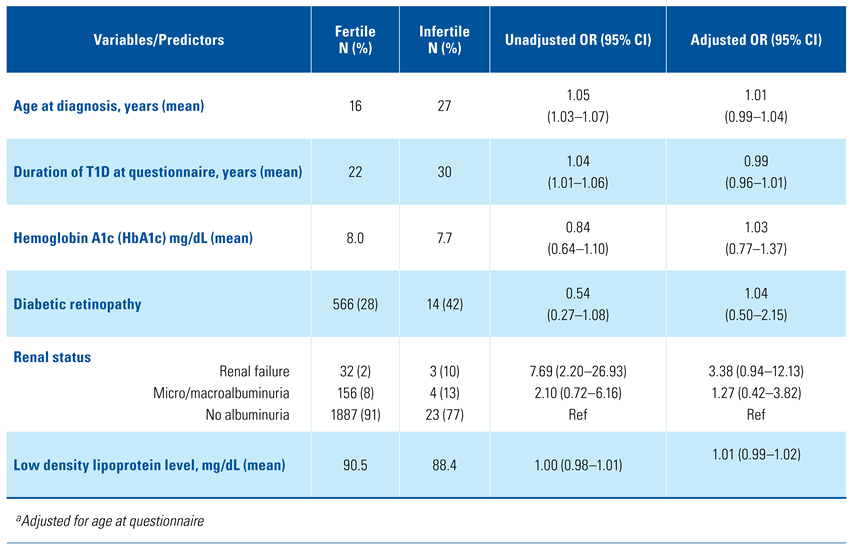
Statistical analysis
Results
Discussion
Conclusions
Conflicts of Interest
Appendix 1. Participating research centres

References
- Arora, R.; Koch, M.O.; Eble, J.N.; Ulbright, T.M.; Li, L.; Cheng, L.; Jangir, R.N.; Jain, G.C. Diabetes mellitus induced impairment of male reproductive functions: a review. Curr. Diabetes Rev. 2014, 10, 147–157. [Google Scholar]
- Kasturi, S.S.; Tannir, J.; Brannigan, R.E. The metabolic syndrome and male infertility. J. Androl. 2008, 29, 251–259. [Google Scholar] [CrossRef] [PubMed]
- Gu, K.; Cowie, C.C.; Harris, M.I. Mortality in adults with and without diabetes in a national cohort of the U.S. population, 1971–1993. Diabetes Care 1998, 21, 1138–1145. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association. Economic costs of diabetes in the U.S. in 2012. Diabetes Care 2013, 36, 1033–1046. [Google Scholar] [CrossRef] [PubMed]
- Monga, M.; Alexandrescu, B.; Katz, S.E.; Stein, M.; Ganiats, T. Impact of infertility on quality of life, marital adjustment, and sexual function. Urology 2004, 63, 126–130. [Google Scholar] [CrossRef] [PubMed]
- Walsh, T.J.; Schembri, M.; Turek, P.J.; Chan, J.M.; Carroll, P.R.; Smith, J.F.; et al. Increased risk of high-grade prostate cancer among infertile men. Cancer 2010, 116, 2140–2147. [Google Scholar] [CrossRef] [PubMed]
- Hotaling, J.M.; Walsh, T.J. Male infertility: a risk factor for testicular cancer. Nat. Rev. Urol. 2009, 6, 550–556. [Google Scholar] [CrossRef] [PubMed]
- Beck, R.W.; Tamborlane, W.V.; Bergenstal, R.M.; Miller, K.M.; DuBose, S.N.; Hall, C.A.; T1D Exchange Clinic Network. The T1D exchange clinic registry. J. Clin. Endocrinol. Metab. 2012, 97, 4383–4389. [Google Scholar] [CrossRef] [PubMed]
- Eisenberg, M.L.; Li, S.; Cullen, M.R.; Baker, L.C. Increased risk of incident chronic medical conditions in infertile men: analysis of United States claims data. Fertil. Steril. 2015, 105, 629–636. [Google Scholar] [CrossRef] [PubMed]
- Glazer, C.H.; Bonde, J.P.; Giwercman, A.; Vassard, D.; Pinborg, A.; Schmidt, L.; et al. Risk of diabetes according to male factor infertility: a register- based cohort study. Hum. Reprod. 2017, 32, 1474–1481. [Google Scholar] [CrossRef] [PubMed]
- Eisenberg, M.L.; Li, S.; Behr, B.; Pera, R.R.; Cullen, M.R. Relationship between semen production and medical comorbidity. Fertil. Steril. 2015, 103, 66–71. [Google Scholar] [CrossRef] [PubMed]
- Fedder, J.; Kaspersen, M.D.; Brandslund, I.; Hojgaard, A. Retrograde ejaculation and sexual dysfunction in men with diabetes mellitus: a prospective, controlled study. Andrology 2013, 1, 602–606. [Google Scholar] [CrossRef] [PubMed]
- Kasturi, S.S.; Tannir, J.; Brannigan, R.E. The metabolic syndrome and male infertility. J. Androl. 2008, 29, 251–259. [Google Scholar] [CrossRef] [PubMed]
- Sharma, R.; Agarwal, A.; Rohra, V.K.; Assidi, M.; Abu-Elmagd, M.; Turki, R.F. Effects of increased paternal age on sperm quality, reproductive outcome and associated epigenetic risks to offspring. Reprod. Biol. Endocrinol. 2015, 13, 35. [Google Scholar] [CrossRef] [PubMed]
- Ventimiglia, E.; Capogrosso, P.; Boeri, L.; Serino, A.; Colicchia, M.; Ippolito, S.; et al. Infertility as a proxy of general male health: results of a cross-sectional survey. Fertil. Steril. 2015, 104, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Salonia, A.; Matloob, R.; Gallina, A.; Abdollah, F.; Sacca, A.; Briganti, A.; et al. Are infertile men less healthy than fertile men? Results of a prospective case-control survey. Eur. Urol. 2009, 56, 1025–1031. [Google Scholar] [CrossRef] [PubMed]
- Biggs, M.L.; Mukamal, K.J.; Luchsinger, J.A.; Ix, J.H.; Carnethon, M.R.; Newman, A.B.; et al. Association between adiposity in midlife and older age and risk of diabetes in older adults. JAMA 2010, 303, 2504–2512. [Google Scholar] [CrossRef] [PubMed]
- Tarin, J.J.; Garcia-Perez, M.A.; Hamatani, T.; Cano, A. Infertility etiologies are genetically and clinically linked with other diseases in single meta-diseases. Reprod. Biol. Endocrinol. 2015, 13, 31. [Google Scholar] [CrossRef] [PubMed]
- Matzuk, M.M.; Lamb, D.J. The biology of infertility: research advances and clinical challenges. Nat. Med. 2008, 14, 1197–1213. [Google Scholar] [CrossRef] [PubMed]
This is an open access article under the terms of a license that permits non-commercial use, provided the original work is properly cited. © 2021 The Authors. Société Internationale d'Urologie Journal, published by the Société Internationale d'Urologie, Canada.
Share and Cite
Raheem, O.A.; Hehemann, M.C.; Rogers, M.J.; Fustok, J.N.; Hirsch, I.B.; Walsh, T.J. Does Type 1 Diabetes Affect Male Infertility: Type 1 Diabetes Exchange Registry-Based Analysis. Soc. Int. Urol. J. 2021, 2, 139-143. https://doi.org/10.48083/VVMV5977
Raheem OA, Hehemann MC, Rogers MJ, Fustok JN, Hirsch IB, Walsh TJ. Does Type 1 Diabetes Affect Male Infertility: Type 1 Diabetes Exchange Registry-Based Analysis. Société Internationale d’Urologie Journal. 2021; 2(3):139-143. https://doi.org/10.48083/VVMV5977
Chicago/Turabian StyleRaheem, Omer A., Marah C. Hehemann, Marc J. Rogers, Judy N. Fustok, Irl B. Hirsch, and Thomas J. Walsh. 2021. "Does Type 1 Diabetes Affect Male Infertility: Type 1 Diabetes Exchange Registry-Based Analysis" Société Internationale d’Urologie Journal 2, no. 3: 139-143. https://doi.org/10.48083/VVMV5977
APA StyleRaheem, O. A., Hehemann, M. C., Rogers, M. J., Fustok, J. N., Hirsch, I. B., & Walsh, T. J. (2021). Does Type 1 Diabetes Affect Male Infertility: Type 1 Diabetes Exchange Registry-Based Analysis. Société Internationale d’Urologie Journal, 2(3), 139-143. https://doi.org/10.48083/VVMV5977




