Tissue-Based Immunohistochemical Markers for Diagnosis and Classification of Renal Cell Carcinoma
Abstract
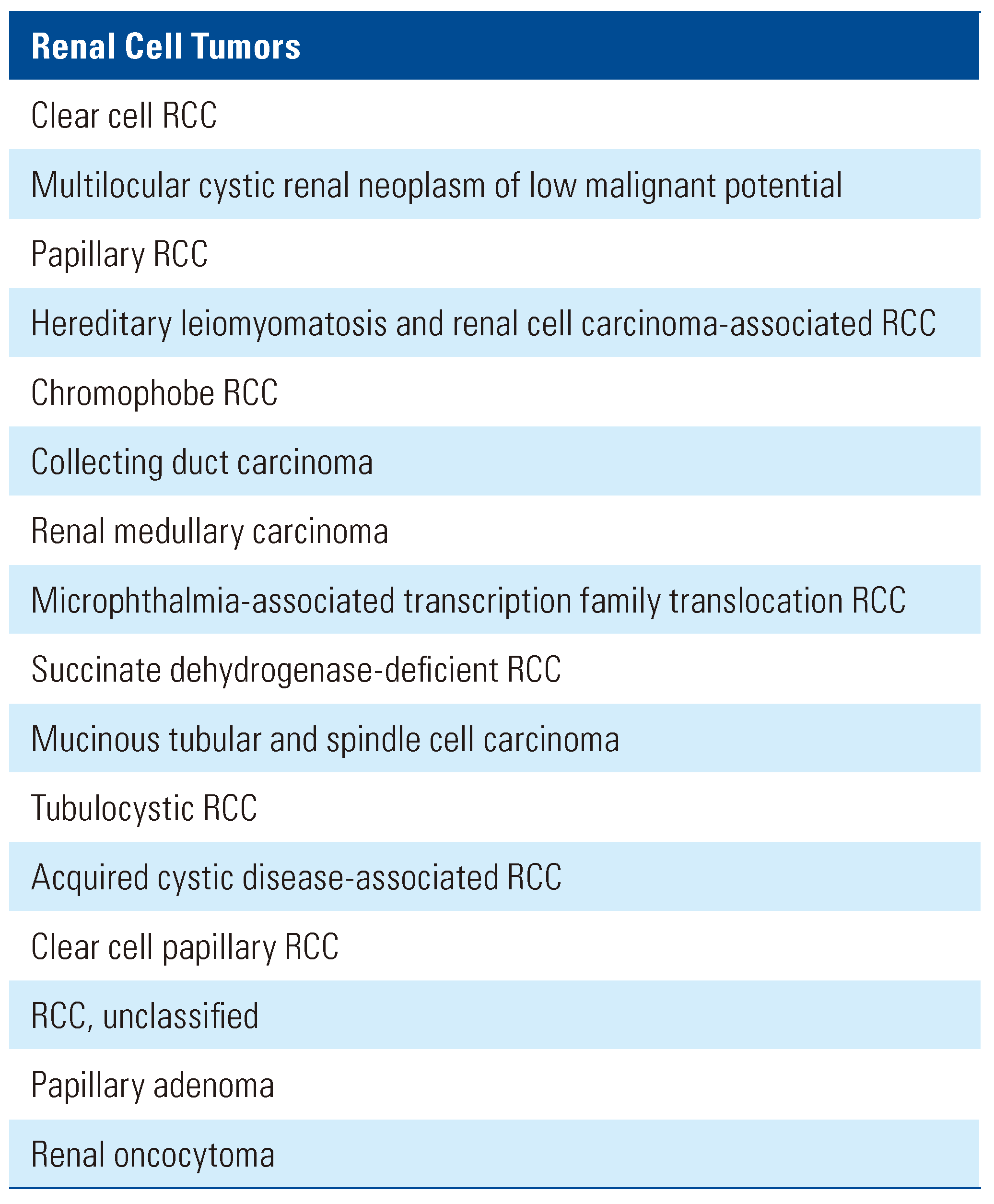
:Introduction
Clear Cell RCC
Papillary RCC
Chromophobe RCC
Renal Oncocytoma
Other RCC Subtypes
Other Tissue Markers
Conclusions
Conflicts of Interest
Abbreviations
| AMACR | alpha-methylacyl coenzyme A racemase |
| BAP1 | BRCA1-associated protein 1 |
| CAIX | carbonic anhydrase 9 |
| ccRCC | clear cell RCC |
| CD10 | cluster differential marker 10 |
| chRCC | chromophobe RCC |
| CK | cytokeratin |
| EMA | epithelial membrane antigen |
| hKIM-1 | human kidney injury molecule-1 |
| HMWCK | high molecular weight CK |
| IHC | immunohistochemical |
| MiT | microphthalmia-associated transcription |
| RCC | renal cell carcinoma |
| RCCM | RCC marker |
| RO | renal oncocytoma |
References
- Williamson, S.R.; Gill, A.J.; Argani, P.; et al. Report From the International Society of Urological Pathology (ISUP) Consultation Conference on Molecular Pathology of Urogenital Cancers: III: Molecular Pathology of Kidney Cancer. Am. J. Surg. Pathol. 2020, 44, e47–e65. [Google Scholar] [CrossRef] [PubMed]
- Srigley, J.R.; Delahunt, B.; Eble, J.N.; et al. The International Society of Urological Pathology (ISUP) Vancouver Classification of Renal Neoplasia. Am. J. Surg. Pathol. 2013, 37, 1469–1489. [Google Scholar] [CrossRef] [PubMed]
- Signoretti, S.; Flaifel, A.; Chen, Y.B.; Reuter, V.E. Renal Cell Carcinoma in the Era of Precision Medicine: From Molecular Pathology to Tissue- Based Biomarkers. J. Clin. Oncol. 2018, 36, 3553–3559. [Google Scholar] [CrossRef] [PubMed]
- Di Napoli, A.; Signoretti, S. Tissue biomarkers in renal cell carcinoma: Issues and solutions. Cancer 2009, 115 (Suppl. S10), 2290–2297. [Google Scholar] [CrossRef] [PubMed]
- Moch, H.; Cubilla, A.L.; Humphrey, P.A.; Reuter, V.E.; Ulbright, T.M. The 2016 WHO classification of tumours of the urinary system and male genital organs-Part A: Renal, penile, and testicular tumours. Eur. Urol. 2016, 70, 93–105. [Google Scholar] [CrossRef] [PubMed]
- Taylor, A.S.; Spratt, D.E.; Dhanasekaran, S.M.; Mehra, R. Contemporary renal tumor categorization with biomarker and translational updates: A practical review. Arch. Pathol. Lab. Med. 2019, 143, 1477–1491. [Google Scholar] [CrossRef]
- Reuter, V.E.; Tickoo, S.K. Differential diagnosis of renal tumours with clear cell histology. Pathology 2010, 42, 374–383. [Google Scholar] [CrossRef] [PubMed]
- Alshenawy, H.A. Immunohistochemical panel for differentiating renal cell carcinoma with clear and papillary features. Pathol. Oncol. Res. 2015, 21, 893–899. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Beltran, A.; Henriques, V.; Cimadamore, A.; et al. The Identification of immunological biomarkers in kidney cancers. Front. Oncol. 2018, 8, 456. [Google Scholar] [CrossRef] [PubMed]
- Mazal, P.R.; Exner, M.; Haitel, A.; et al. Expression of kidney-specific cadherin distinguishes chromophobe renal cell carcinoma from renal oncocytoma. Hum. Pathol. 2005, 36, 22–28. [Google Scholar] [CrossRef] [PubMed]
- Lin, F.; Zhang, P.L.; Yang, X.J.; et al. Human kidney injury molecule-1 (hKIM-1): A useful immunohistochemical marker for diagnosing renal cell carcinoma and ovarian clear cell carcinoma. Am. J. Surg. Pathol. 2007, 31, 371–381. [Google Scholar] [CrossRef] [PubMed]
- Chu, P.G.; Weiss, L.M. Cytokeratin 14 immunoreactivity distinguishes oncocytic tumour from its renal mimics: An immunohistochemical study of 63 cases. Histopathology 2001, 39, 455–462. [Google Scholar] [CrossRef] [PubMed]
- Langner, C.; Wegscheider, B.J.; Ratschek, M.; Schips, L.; Zigeuner, R. Keratin immunohistochemistry in renal cell carcinoma subtypes and renal oncocytomas: A systematic analysis of 233 tumors. Virchows Arch. 2004, 444, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Warren, A.Y.; Harrison, D. WHO/ISUP classification, grading and pathological staging of renal cell carcinoma: Standards and controversies. World J. Urol. 2018, 36, 1913–1926. [Google Scholar] [CrossRef] [PubMed]
- Skinnider, B.F.; Folpe, A.L.; Hennigar, R.A.; et al. Distribution of cytokeratins and vimentin in adult renal neoplasms and normal renal tissue: Potential utility of a cytokeratin antibody panel in the differential diagnosis of renal tumors. Am. J. Surg. Pathol. 2005, 29, 747–754. [Google Scholar] [CrossRef] [PubMed]
- Young, A.N.; de Oliveira Salles, P.G.; Lim, S.D.; et al. Beta defensin-1, parvalbumin, and vimentin: A panel of diagnostic immunohistochemical markers for renal tumors derived from gene expression profiling studies using cDNA microarrays. Am. J. Surg. Pathol. 2003, 27, 199–205. [Google Scholar] [CrossRef] [PubMed]
- Aboulhagag, N.A.; El-Deek, H.E.M.; Sherif, M.F. Expression of galectin-1 and galectin-3 in renal cell carcinoma; immunohistochemical study. Ann. Diagn. Pathol. 2018, 36, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Petit, A.; Castillo, M.; Santos, M.; Mellado, B.; Alcover, J.B.; Mallofre, C. KIT expression in chromophobe renal cell carcinoma: Comparative immunohistochemical analysis of KIT expression in different renal cell neoplasms. Am. J. Surg. Pathol. 2004, 28, 676–678. [Google Scholar] [CrossRef] [PubMed]
- Martignoni, G.; Pea, M.; Chilosi, M.; et al. Parvalbumin is constantly expressed in chromophobe renal carcinoma. Mod. Pathol. 2001, 14, 760–767. [Google Scholar] [CrossRef] [PubMed]
- Adley, B.P.; Gupta, A.; Lin, F.; Luan, C.; Teh, B.T.; Yang, X.J. Expression of kidney-specific cadherin in chromophobe renal cell carcinoma and renal oncocytoma. Am. J. Clin. Pathol. 2006, 126, 79–85. [Google Scholar] [CrossRef]
- Osunkoya, A.O.; Cohen, C.; Lawson, D.; Picken, M.M.; Amin, M.B.; Young, A.N. Claudin-7 and claudin-8: Immunohistochemical markers for the differential diagnosis of chromophobe renal cell carcinoma and renal oncocytoma. Hum. Pathol. 2009, 40, 206–210. [Google Scholar] [CrossRef] [PubMed]
- Langner, C.; Ratschek, M.; Rehak, P.; Schips, L.; Zigeuner, R. Expression of MUC1 (EMA) and E-cadherin in renal cell carcinoma: A systematic immunohistochemical analysis of 188 cases. Mod. Pathol. 2004, 17, 180–188. [Google Scholar] [CrossRef] [PubMed]
- Allory, Y.; Bazille, C.; Vieillefond, A.; et al. Profiling and classification tree applied to renal epithelial tumours. Histopathology 2008, 52, 158–166. [Google Scholar] [CrossRef] [PubMed]
- Wi, Y.C.; Moon, A.; Jung, M.J.; et al. Loss of nuclear BAP1 expression is associated with high WHO/ISUP grade in clear cell renal cell carcinoma. J. Pathol. Transl. Med. 2018, 52, 378. [Google Scholar] [CrossRef] [PubMed]
- McGregor, D.K.; Khurana, K.K.; Cao, C.; et al. Diagnosing primary and metastatic renal cell carcinoma: The use of the monoclonal antibody ‘Renal Cell Carcinoma Marker’. Am. J. Surg. Pathol. 2001, 25, 1485–1492. [Google Scholar] [CrossRef] [PubMed]
- Mentrikoski, M.J.; Wendroth, S.M.; Wick, M.R. Immunohistochemical distinction of renal cell carcinoma from other carcinomas with clear-cell histomorphology: Utility of CD10 and CA-125 in addition to PAX-2, PAX-8, RCCma, and adipophilin. Appl. Immunohistochem. Mol. Morphol. 2014, 22, 635–641. [Google Scholar] [CrossRef] [PubMed]
- Avery, A.K.; Beckstead, J.; Renshaw, A.A.; Corless, C.L. Use of antibodies to RCC and CD10 in the differential diagnosis of renal neoplasms. Am. J. Surg. Pathol. 2000, 24, 203–210. [Google Scholar] [CrossRef] [PubMed]
- Renshaw, A.A.; Zhang, H.; Corless, C.L.; Fletcher, J.A.; Pins, M.R. Solid variants of papillary (chromophil) renal cell carcinoma: Clinicopathologic and genetic features. Am. J. Surg. Pathol. 1997, 21, 1203–1209. [Google Scholar] [CrossRef] [PubMed]
- Molinie, V.; Balaton, A.; Rotman, S.; et al. Alpha-methyl CoA racemase expression in renal cell carcinomas. Hum. Pathol. 2006, 37, 698–703. [Google Scholar] [CrossRef] [PubMed]
- Shen, S.S.; Truong, L.D.; Scarpelli, M.; Lopez-Beltran, A. Role of immunohistochemistry in diagnosing renal neoplasms: When is it really useful? Arch. Pathol. Lab. Med. 2012, 136, 410–417. [Google Scholar] [CrossRef] [PubMed]
- Alexa, A.; Baderca, F.; Lighezan, R.; Zahoi, D.E.; Izvernariu, D. The diagnostic value of EMA expression in the renal parenchyma tumors. Rom. J. Morphol. Embryol. 2011, 52 (Suppl. S3), 1019–1025. [Google Scholar] [PubMed]
- Ahmed, E.A.; Youssif, M.E. Immunohistochemical study of c-KIT (CD117) expression in renal cell carcinoma. J. Egypt. Natl. Canc Inst. 2009, 21, 121–132. [Google Scholar] [PubMed]
- Hornsby, C.D.; Cohen, C.; Amin, M.B.; et al. Claudin-7 immunohistochemistry in renal tumors: A candidate marker for chromophobe renal cell carcinoma identified by gene expression profiling. Arch. Pathol. Lab. Med. 2007, 131, 1541–1546. [Google Scholar] [CrossRef] [PubMed]
- Lechpammer, M.; Resnick, M.B.; Sabo, E.; et al. The diagnostic and prognostic utility of claudin expression in renal cell neoplasms. Mod. Pathol. 2008, 21, 1320–1329. [Google Scholar] [CrossRef] [PubMed]
- Tickoo, S.K.; Reuter, V.E. Differential diagnosis of renal tumors with papillary architecture. Adv. Anat. Pathol. 2011, 18, 120–132. [Google Scholar] [CrossRef] [PubMed]
- Shen, S.S.; Krishna, B.; Chirala, R.; Amato, R.J.; Truong, L.D. Kidney-specific cadherin, a specific marker for the distal portion of the nephron and related renal neoplasms. Mod. Pathol. 2005, 18, 933–940. [Google Scholar] [CrossRef] [PubMed]
- Huo, L.; Sugimura, J.; Tretiakova, M.S.; et al. C-kit expression in renal oncocytomas and chromophobe renal cell carcinomas. Hum. Pathol. 2005, 36, 262–268. [Google Scholar] [CrossRef] [PubMed]
- Skala, S.L.; Wang, X.; Zhang, Y.; et al. Next-generation RNA sequencing– based biomarker characterization of chromophobe renal cell carcinoma and related oncocytic neoplasms. Eur. Urol. 2020, 78, 63–74. [Google Scholar] [CrossRef] [PubMed]
- El-Shorbagy, S.H.; Alshenawy, H.A. Diagnostic utility of vimentin, CD117, cytokeratin-7 and caveolin-1 in differentiation between clear cell renal cell carcinoma, chromophobe renal cell carcinoma and oncocytoma. J. Microsc. Ultrastruct. 2017, 5, 90–96. [Google Scholar] [PubMed]
- Stopyra, G.A.; Warhol, M.J.; Multhaupt, H.A. Cytokeratin 20 immunoreactivity in renal oncocytomas. J. Histochem. Cytochem. 2001, 49, 919–920. [Google Scholar] [CrossRef]
- Genega, E.M.; Ghebremichael, M.; Najarian, R.; et al. Carbonic anhydrase IX expression in renal neoplasms: Correlation with tumor type and grade. Am. J. Clin. Pathol. 2010, 134, 873–879. [Google Scholar] [CrossRef] [PubMed]
- Kuroda, N.; Kanomata, N.; Yamaguchi, T.; et al. Immunohistochemical application of S100A1 in renal oncocytoma, oncocytic papillary renal cell carcinoma, and two variants of chromophobe renal cell carcinoma. Med. Mol. Morphol. 2011, 44, 111–115. [Google Scholar] [CrossRef] [PubMed]
- Garcia, E.; Li, M. Caveolin-1 immunohistochemical analysis in differentiating chromophobe renal cell carcinoma from renal oncocytoma. Am. J. Clin. Pathol. 2006, 125, 392–398. [Google Scholar] [CrossRef] [PubMed]
- Tamaskar, I.; Choueiri, T.K.; Sercia, L.; Rini, B.; Bukowski, R.; Zhou, M. Differential expression of caveolin-1 in renal neoplasms. Cancer 2007, 110, 776–782. [Google Scholar] [CrossRef] [PubMed]
- Ng, K.L.; Ellis, R.J.; Samaratunga, H.; Morais, C.; Gobe, G.C.; Wood, S.T. Utility of cytokeratin 7, S100A1 and caveolin-1 as immunohistochemical biomarkers to differentiate chromophobe renal cell carcinoma from renal oncocytoma. Transl. Androl. Urol. 2019, 8 (Suppl. S2), S123–S137. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.; Roy, S.; Amin, M.; et al. Amylase alpha-1A (AMY1A): A novel immunohistochemical marker to differentiate chromophobe renal cell carcinoma from benign oncocytoma. Am. J. Surg. Pathol. 2013, 37, 1824–1830. [Google Scholar] [CrossRef] [PubMed]
- Rao, Q.; Liu, X.H.; Zhou, H.B.; Ma, H.H.; Lu, Z.F.; Zhou, X.J. Expression analysis of Wnt-5a in renal epithelial neoplasms: Distinguishing renal oncocytoma from a wide spectrum of renal cell carcinomas. Tumori. 2010, 96, 304–309. [Google Scholar] [CrossRef] [PubMed]
- Gaut, J.P.; Crimmins, D.L.; Lockwood, C.M.; McQuillan, J.J.; Ladenson, J.H. Expression of the Na+/K+-transporting ATPase gamma subunit FXYD2 in renal tumors. Mod. Pathol. 2013, 26, 716–724. [Google Scholar] [CrossRef] [PubMed]
- Shomori, K.; Nagashima, Y.; Kuroda, N.; et al. ARPP protein is selectively expressed in renal oncocytoma, but rarely in renal cell carcinomas. Mod. Pathol. 2007, 20, 199–207. [Google Scholar] [CrossRef] [PubMed]
- Mete, O.; Kilicaslan, I.; Gulluoglu, M.G.; Uysal, V. Can renal oncocytoma be differentiated from its renal mimics? The utility of anti- mitochondrial, caveolin 1, CD63 and cytokeratin 14 antibodies in the differential diagnosis. Virchows Arch. 2005, 447, 938–946. [Google Scholar] [CrossRef]
- Demirovic, A.; Cesarec, S.; Marusic, Z.; et al. TGF-beta1 expression in chromophobe renal cell carcinoma and renal oncocytoma. Eur. J. Histochem. 2014, 58, 2265. [Google Scholar] [CrossRef]
- Artas, G.; Kuloglu, T.; Dagli, A.F.; et al. A promising biomarker to distinguish benign and malignant renal tumors: ELABELA. Niger. J. Clin. Pract. 2019, 22, 386–392. [Google Scholar] [CrossRef] [PubMed]
- Kowalewski, A.; Szylberg, L.; Tyloch, J.; et al. Caspase 3 as a novel marker to distinguish chromophobe renal cell carcinoma from oncocytoma. Pathol. Oncol. Res. 2019, 25, 1519–1524. [Google Scholar] [CrossRef] [PubMed]
- Ng, K.L.; Del Vecchio, S.J.; Samaratunga, H.; et al. Leptin and its receptor: Can they help to differentiate chromophobe renal cell carcinoma from renal oncocytoma? Pathology 2018, 50, 504–510. [Google Scholar] [CrossRef] [PubMed]
- Sun, T.; Hutchinson, L.; Zhou, A.G.; et al. The utility of ERBB4 and RB1 immunohistochemistry in distinguishing chromophobe renal cell carcinoma from renal oncocytoma. Int. J. Surg. Pathol. 2020, 28, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Damayanti, N.P.; Budka, J.A.; Khella, H.W.Z.; et al. Therapeutic targeting of TFE3/IRS-1/PI3K/mTOR axis in translocation renal cell carcinoma. Clin. Cancer Res. 2018, 24, 5977–5989. [Google Scholar] [CrossRef] [PubMed]
- Green, W.M.; Yonescu, R.; Morsberger, L.; et al. Utilization of a TFE3 break-apart FISH assay in a renal tumor consultation service. Am. J. Surg. Pathol. 2013, 37, 1150–1163. [Google Scholar] [CrossRef] [PubMed]
- Davis, I.J.; Hsi, B.L.; Arroyo, J.D.; et al. Cloning of an Alpha-TFEB fusion in renal tumors harboring the t(6;11)(p21;q13) chromosome translocation. Proc. Natl. Acad. Sci. USA 2003, 100, 6051–6056. [Google Scholar] [CrossRef] [PubMed]
- Martignoni, G.; Bonetti, F.; Chilosi, M.; et al. Cathepsin K expression in the spectrum of perivascular epithelioid cell (PEC) lesions of the kidney. Mod. Pathol. 2012, 25, 100–111. [Google Scholar] [CrossRef]
- Martignoni, G.; Pea, M.; Gobbo, S.; et al. Cathepsin-K immunoreactivity distinguishes MiTF/TFE family renal translocation carcinomas from other renal carcinomas. Mod. Pathol. 2009, 22, 1016–1022. [Google Scholar] [CrossRef] [PubMed]
- Calio, A.; Segala, D.; Munari, E.; Brunelli, M.; Martignoni, G. MiT family translocation renal cell carcinoma: From the early descriptions to the current knowledge. Cancers 2019, 11, 1110. [Google Scholar] [CrossRef] [PubMed]
- Przybycin, C.G.; Harper, H.L.; Reynolds, J.P.; et al. Acquired cystic disease- associated renal cell carcinoma (ACD-RCC): A multiinstitutional study of 40 cases with clinical follow-up. Am. J. Surg. Pathol. 2018, 42, 1156–1165. [Google Scholar] [CrossRef] [PubMed]
- Foshat, M.; Eyzaguirre, E. Acquired cystic disease-associated renal cell carcinoma: Review of pathogenesis, morphology, ancillary tests, and clinical features. Arch. Pathol. Lab. Med. 2017, 141, 600–606. [Google Scholar] [CrossRef] [PubMed]
- Gill, A.J.; Hes, O.; Papathomas, T.; et al. Succinate dehydrogenase (SDH)-deficient renal carcinoma: A morphologically distinct entity: A clinicopathologic series of 36 tumors from 27 patients. Am. J. Surg. Pathol. 2014, 38, 1588–1602. [Google Scholar] [CrossRef] [PubMed]
- Williamson, S.R.; Eble, J.N.; Amin, M.B.; et al. Succinate dehydrogenase- deficient renal cell carcinoma: Detailed characterization of 11 tumors defining a unique subtype of renal cell carcinoma. Mod. Pathol. 2015, 28, 80–94. [Google Scholar] [CrossRef] [PubMed]
- Algaba, F.; Akaza, H.; Lopez-Beltran, A.; et al. Current pathology keys of renal cell carcinoma. Eur. Urol. 2011, 60, 634–643. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.J.; Sugimura, J.; Tretiakova, M.S.; et al. Gene expression profiling of renal medullary carcinoma: Potential clinical relevance. Cancer 2004, 100, 976–985. [Google Scholar] [CrossRef] [PubMed]
- Ohe, C.; Smith, S.C.; Sirohi, D.; et al. Reappraisal of morphologic differences between renal medullary carcinoma, collecting duct carcinoma, and fumarate hydratase-deficient renal cell carcinoma. Am. J. Surg. Pathol. 2018, 42, 279–292. [Google Scholar] [CrossRef] [PubMed]
- Rao, P.; Tannir, N.M.; Tamboli, P. Expression of OCT3/4 in renal medullary carcinoma represents a potential diagnostic pitfall. Am. J. Surg. Pathol. 2012, 36, 583–588. [Google Scholar] [CrossRef] [PubMed]
- Murshed, K.A.; Akhtar, M.; Ben-Gashir, M. Multilocular cystic renal neoplasm of low malignant potential extending into the perinephric adipose tissue. Hum. Pathol. 2019, 17, 200305. [Google Scholar] [CrossRef]
- Williamson, S.R.; Halat, S.; Eble, J.N.; et al. Multilocular cystic renal cell carcinoma: Similarities and differences in immunoprofile compared with clear cell renal cell carcinoma. Am. J. Surg. Pathol. 2012, 36, 1425–1433. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.B.; Brannon, A.R.; Toubaji, A.; et al. Hereditary leiomyomatosis and renal cell carcinoma syndrome-associated renal cancer: Recognition of the syndrome by pathologic features and the utility of detecting aberrant succination by immunohistochemistry. Am. J. Surg. Pathol. 2014, 38, 627–637. [Google Scholar] [CrossRef] [PubMed]
- Paner, G.P.; Srigley, J.R.; Radhakrishnan, A.; et al. Immunohistochemical analysis of mucinous tubular and spindle cell carcinoma and papillary renal cell carcinoma of the kidney: Significant immunophenotypic overlap warrants diagnostic caution. Am. J. Surg. Pathol. 2006, 30, 13–19. [Google Scholar] [CrossRef]
- Nathany, S.; Monappa, V. Mucinous tubular and spindle cell carcinoma: A review of histopathology and clinical and prognostic implications. Arch. Pathol. Lab. Med. 2020, 144, 115–118. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Zhang, Y.; Chen, Y.-B.; et al. VSTM2A overexpression is a sensitive and specific biomarker for mucinous tubular and spindle cell carcinoma (MTSCC) of the kidney. Am. J. Surg. Pathol. 2018, 42, 1571–1584. [Google Scholar] [CrossRef] [PubMed]
- Ozcan, A.; de la Roza, G.; Ro, J.Y.; Shen, S.S.; Truong, L.D. PAX2 and PAX8 expression in primary and metastatic renal tumors: A comprehensive comparison. Arch. Pathol. Lab. Med. 2012, 136, 1541–1551. [Google Scholar] [CrossRef] [PubMed]
- Albadine, R.; Schultz, L.; Illei, P.; et al. PAX8 (+)/p63 (-) immunostaining pattern in renal collecting duct carcinoma (CDC): A useful immunoprofile in the differential diagnosis of CDC versus urothelial carcinoma of upper urinary tract. Am. J. Surg. Pathol. 2010, 34, 965–969. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, K.H.; Siddiqui, M.T.; Cohen, C. GATA3 immunohistochemical expression in invasive urothelial carcinoma. Urol. Oncol. 2016, 34, 432.e9–e13. [Google Scholar] [CrossRef] [PubMed]
- Trpkov, K.; Abou-Ouf, H.; Hes, O.; et al. Eosinophilic solid and cystic renal cell carcinoma (ESC RCC): Further morphologic and molecular characterization of ESC RCC as a distinct entity. Am. J. Surg. Pathol. 2017, 41, 1299–1308. [Google Scholar] [CrossRef] [PubMed]
- de Velasco, G.; Wankowicz, S.A.; Madison, R.; et al. Targeted genomic landscape of metastases compared to primary tumours in clear cell metastatic renal cell carcinoma. Br. J. Cancer. 2018, 118, 1238–1242. [Google Scholar] [CrossRef]
- Durinck, S.; Stawiski, E.W.; Pavía-Jiménez, A.; et al. Spectrum of diverse genomic alterations define non–clear cell renal carcinoma subtypes. Nat. Genet. 2015, 47, 13. [Google Scholar] [CrossRef] [PubMed]
- Kaelin, W.G. Molecular basis of the VHL hereditary cancer syndrome. Nat. Rev. Cancer 2002, 2, 673–682. [Google Scholar] [CrossRef] [PubMed]
- Lin, F.; Shi, J.; Liu, H.; et al. Immunohistochemical detection of the von Hippel-Lindau gene product (pVHL) in human tissues and tumors: A useful marker for metastatic renal cell carcinoma and clear cell carcinoma of the ovary and uterus. Am. J. Clin. Pathol. 2008, 129, 592–605. [Google Scholar] [CrossRef] [PubMed]
- Pawłowski, R.; Mühl, S.M.; Sulser, T.; Krek, W.; Moch, H.; Schraml, P. Loss of PBRM1 expression is associated with renal cell carcinoma progression. Int. J. Cancer. 2013, 132, E11–E17. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Liu, L.; Qu, Y.; et al. Prognostic value of SETD2 expression in patients with metastatic renal cell carcinoma treated with tyrosine kinase inhibitors. J. Urol. 2016, 196, 1363–1370. [Google Scholar] [CrossRef] [PubMed]
 |
 |
This is an open access article under the terms of a license that permits non-commercial use, provided the original work is properly cited. © 2020 The Authors. Société Internationale d'Urologie Journal, published by the Société Internationale d'Urologie, Canada.
Share and Cite
Qu, L.; Thirugnanasundralingam, V.; Bolton, D.; Finelli, A.; Lawrentschuk, N. Tissue-Based Immunohistochemical Markers for Diagnosis and Classification of Renal Cell Carcinoma. Soc. Int. Urol. J. 2020, 1, 68-76. https://doi.org/10.48083/MQYE9599
Qu L, Thirugnanasundralingam V, Bolton D, Finelli A, Lawrentschuk N. Tissue-Based Immunohistochemical Markers for Diagnosis and Classification of Renal Cell Carcinoma. Société Internationale d’Urologie Journal. 2020; 1(1):68-76. https://doi.org/10.48083/MQYE9599
Chicago/Turabian StyleQu, Liang, Vaisnavi Thirugnanasundralingam, Damien Bolton, Antonio Finelli, and Nathan Lawrentschuk. 2020. "Tissue-Based Immunohistochemical Markers for Diagnosis and Classification of Renal Cell Carcinoma" Société Internationale d’Urologie Journal 1, no. 1: 68-76. https://doi.org/10.48083/MQYE9599
APA StyleQu, L., Thirugnanasundralingam, V., Bolton, D., Finelli, A., & Lawrentschuk, N. (2020). Tissue-Based Immunohistochemical Markers for Diagnosis and Classification of Renal Cell Carcinoma. Société Internationale d’Urologie Journal, 1(1), 68-76. https://doi.org/10.48083/MQYE9599




