Diagnostic Accuracy of Multiple D-Dimer Cutoff Thresholds and Other Clinically Applicable Biomarkers for the Detection and Radiographic Evaluation of Pulmonary Embolism
Abstract
:Highlights
- According to recent guidelines for the diagnosis and management of pulmonary embolism (PE), the conventional Dd cutoff (0.5 mg/L) has excellent sensitivity for the diagnosis of PE, although there is a marked decrease in specificity.
- Age-adjusted Dd cutoff thresholds for ruling out diagnoses of PE in emergency departments have significantly improved the performance of Dd testing, especially for the elderly, although little is known about the efficacy to reduce the number of CTPAs that could have been performed.
- The most interesting finding in our study was that the novel proposed Dd cutoff (0.74 mg/L) emerged with increased specificity and equal sensitivity compared with 0.5 mg/L and could have reduced the number of CTPAs that were performed in our institution by 17.2%.
- Ancillary CTPA insights of consolidation/atelectasis and unilateral pleural effusion were significantly associated with PE.
Abstract
1. Introduction
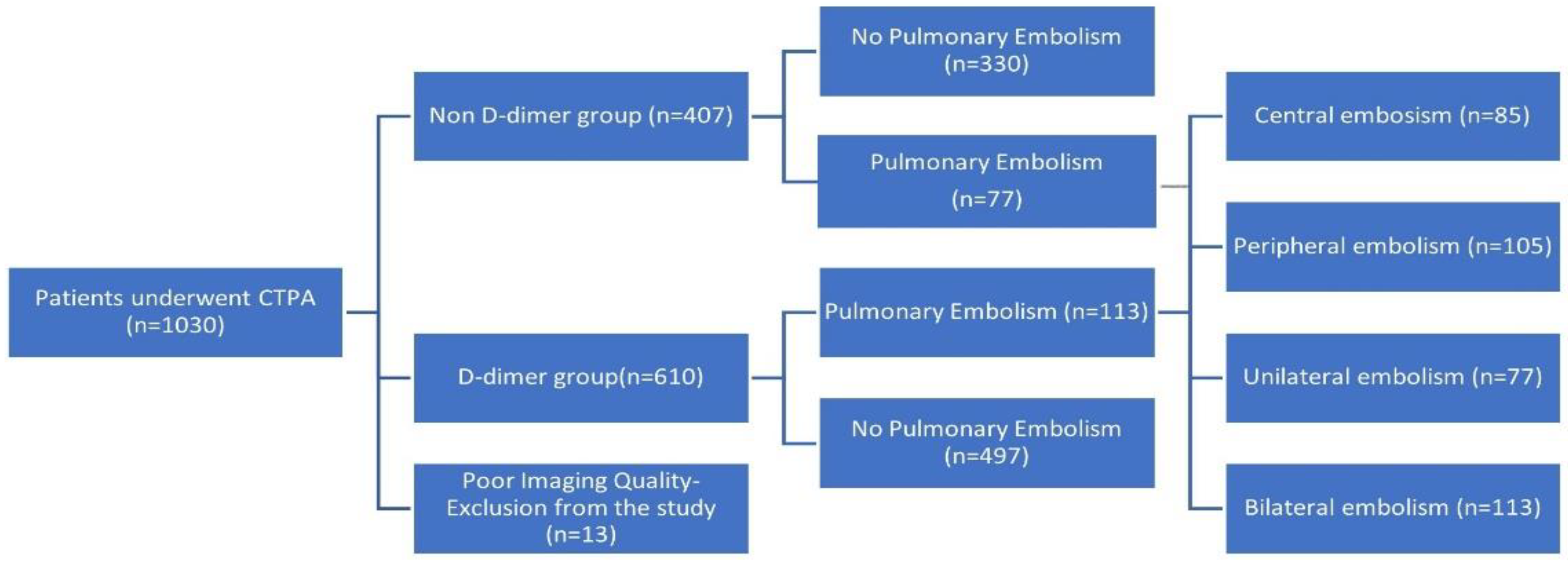
2. Material and Methods
2.1. CTPA Assessment
2.2. D-Dimer and RDW Assays
2.3. Statistical Analysis
3. Results
3.1. Patient Baseline Characteristics
3.2. Parenchymal and Pleural CTPA Findings in Patients with or without PE
3.3. Association of Dd and RDW with PE Location, CTPA Findings and Patient Outcome
3.4. Diagnostic Accuracy of Different Dd Cutoffs for Ruling out PE
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wendelboe, A.M.; Raskob, G.E. Global Burden of Thrombosis. Circ. Res. 2016, 118, 1340–1347. [Google Scholar] [CrossRef] [PubMed]
- Konstantinides, S.V.; Meyer, G.; Becattini, C.; Bueno, H.; Geersing, G.-J.; Harjola, V.-P.; Huisman, M.V.; Humbert, M.; Jennings, C.S.; Jiménez, D.; et al. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS): The Task Force for the diagnosis and management of acute pulmonary embolism of the European Society of Cardiology (ESC). Eur. Heart J. 2020, 41, 543–603. [Google Scholar]
- Lim, W.; Le Gal, G.; Bates, S.M.; Righini, M.; Haramati, L.B.; Lang, E.; Kline, J.A.; Chasteen, S.; Snyder, M.; Patel, P.; et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: Diagnosis of venous thromboembolism. Blood Adv. 2018, 2, 3226–3256. [Google Scholar] [CrossRef] [PubMed]
- Douma, R.A. Performance of 4 Clinical Decision Rules in the Diagnostic Management of Acute Pulmonary Embolism: A Prospective Cohort Study. Ann. Intern. Med. 2011, 154, 709. [Google Scholar] [CrossRef]
- Shen, J.-H.; Chen, H.-L.; Chen, J.-R.; Xing, J.-L.; Gu, P.; Zhu, B.-F. Comparison of the Wells score with the revised Geneva score for assessing suspected pulmonary embolism: A systematic review and meta-analysis. J. Thromb. Thrombolysis 2016, 41, 482–492. [Google Scholar] [CrossRef] [PubMed]
- Girardi, A.M.; Bettiol, R.S.; Garcia, T.S.; Ribeiro, G.L.H.; Rodrigues, É.M.; Gazzana, M.B.; Ribeiro, G.L.H.; Rodrigues, É.M.R.; Gazzana, M.B.; Rech, T.H. Wells and Geneva Scores Are Not Reliable Predictors of Pulmonary Embolism in Critically Ill Patients: A Retrospective Study. J. Intensive Care Med. 2020, 35, 1112–1117. [Google Scholar] [CrossRef] [PubMed]
- Fesmire, F.M.; Brown, M.D.; Espinosa, J.A.; Shih, R.D.; Silvers, S.M.; Wolf, S.J.; Decker, W.W. Critical Issues in the Evaluation and Management of Adult Patients Presenting to the Emergency Department with Suspected Pulmonary Embolism. Ann. Emerg. Med. 2011, 57, 628–652.e75. [Google Scholar] [CrossRef]
- Linkins, L.-A.; Lapner, S.T. Review of D-dimer testing: Good, Bad, and Ugly. Int. J. Lab. Hematol. 2017, 39 (Suppl. S1), 98–103. [Google Scholar] [CrossRef] [Green Version]
- Righini, M.; Van Es, J.; Den Exter, P.L.; Roy, P.-M.; Verschuren, F.; Ghuysen, A.; Rutschmann, O.T.; Sanchez, O.; Jaffrelot, M.; Trinh-Duc, A.; et al. Age-Adjusted D-Dimer Cutoff Levels to Rule Out Pulmonary Embolism: The ADJUST-PE Study. JAMA 2014, 311, 1117. [Google Scholar] [CrossRef]
- Parry, B.A.; Chang, A.M.; Schellong, S.M.; House, S.L.; Fermann, G.J.; Deadmon, E.K.; Giordano, N.J.; Chang, Y.; Cohen, J.; Robak, N.; et al. International, multicenter evaluation of a new D-dimer assay for the exclusion of venous thromboembolism using standard and age-adjusted cut-offs. Thromb. Res. 2018, 166, 63–70. [Google Scholar] [CrossRef]
- Reardon, P.M.; Patrick, S.; Taljaard, M.; Thavorn, K.; Nemnom, M.-J.; Mukarram, M.; Kim, S.-M.; Le Gal, G.; Huang, L.; Thiruganasambandamoorthy, V. Diagnostic Accuracy and Financial Implications of Age-Adjusted D-Dimer Strategies for the Diagnosis of Deep Venous Thrombosis in the Emergency Department. J. Emerg. Med. 2019, 56, 469–477. [Google Scholar] [CrossRef] [PubMed]
- Richman, P.B.; Courtney, D.M.; Friese, J.; Matthews, J.; Field, A.; Petri, R.; Kline, J.A. Prevalence and Significance of Nonthromboembolic Findings on Chest Computed Tomography Angiography Performed to Rule Out Pulmonary Embolism: A Multicenter Study of 1,025 Emergency Department Patients. Acad. Emerg. Med. 2004, 11, 642–647. [Google Scholar] [CrossRef]
- Hall, W.B.; Truitt, S.G.; Scheunemann, L.P.; Shah, S.A.; Rivera, M.P.; Parker, L.A.; Carson, S.C. The Prevalence of Clinically Relevant Incidental Findings on Chest Computed Tomographic Angiograms Ordered to Diagnose Pulmonary Embolism. Arch. Intern. Med. 2009, 169, 1961–1965. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stein, P.D.; Fowler, S.E.; Goodman, L.R.; Gottschalk, A.; Hales, C.A.; Hull, R.D.; Leeper, K.V., Jr.; Popovich, J., Jr.; Quinn, D.A.; Sos, T.A.; et al. Multidetector Computed Tomography for Acute Pulmonary Embolism. N. Engl. J. Med. 2006, 354, 2317–2327. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stein, P.D.; Woodard, P.K.; Weg, J.G.; Wakefield, T.W.; Tapson, V.F.; Sostman, H.D.; Sos, T.A.; Quinn, D.A.; Leeper, K.V., Jr.; Hull, R.D.; et al. Diagnostic Pathways in Acute Pulmonary Embolism: Recommendations of the PIOPED II Investigators. Radiology 2007, 242, 15–21. [Google Scholar] [CrossRef] [Green Version]
- Karampitsakos, T.; Dimakou, K.; Papaioannou, O.; Chrysikos, S.; Kaponi, M.; Bouros, D.; Tzouvelekis, A.; Hillas, G. The role of increased red cell distribution width as a negative prognostic marker in patients with COPD. Pulm. Pharmacol. Ther. 2020, 60, 101877. [Google Scholar] [CrossRef]
- Ozsu, S.; Abul, Y.; Gunaydin, S.; Orem, A.; Ozlu, T. Prognostic Value of Red Cell Distribution Width in Patients with Pulmonary Embolism. Clin. Appl. Thromb. 2014, 20, 365–370. [Google Scholar] [CrossRef]
- Karampitsakos, T.; Torrisi, S.; Antoniou, K.; Manali, E.; Korbila, I.; Papaioannou, O.; Sampsonas, F.; Katsaras, M.; Vasarmidi, E.; Papakosta, D.; et al. Increased monocyte count and red cell distribution width as prognostic biomarkers in patients with Idiopathic Pulmonary Fibrosis. Respir. Res. 2021, 22, 140. [Google Scholar] [CrossRef]
- Zorlu, A.; Bektasoglu, G.; Kukul Guven, F.M.; Dogan, O.T.; Gucuk, E.; Refiker Ege, M.; Altay, H.; Cinar, Z.; Tandogan, I.; Yilmaz, M.B. Usefulness of Admission Red Cell Distribution Width as a Predictor of Early Mortality in Patients with Acute Pulmonary Embolism. Am. J. Cardiol. 2012, 109, 128–134. [Google Scholar] [CrossRef]
- Fijałkowska, A.; Wiatr, E.; Kurzyna, M.; Kuca, P.; Burakowski, J.; Kober, J.; Szturmowicz, M.; Wawrzyńska, L.; Roszkowska-Śliż, B.; Tomkowski, W.; et al. Normal D-dimer concentration in hospitalized patients with lung diseases. Adv. Respir. Med. 2012, 80, 101–108. [Google Scholar] [CrossRef]
- Anagnostopoulos, I.; Lagou, S.; Spanorriga, M.K.; Tavernaraki, K.; Poulakou, G.; Syrigos, K.N.; Thanos, L. Epidemiology and diagnosis of pulmonary embolism in lung cancer patients: Is there a role for age adjusted D-dimers cutoff? J. Thromb. Thrombolysis 2020, 49, 572–577. [Google Scholar] [CrossRef] [PubMed]
- Fu, Z.; Zhuang, X.; He, Y.; Huang, H.; Guo, W. The diagnostic value of D-dimer with simplified Geneva score (SGS) pre-test in the diagnosis of pulmonary embolism (PE). J. Cardiothorac. Surg. 2020, 15, 176. [Google Scholar] [CrossRef]
- Kubak, M.P.; Lauritzen, P.M.; Borthne, A.; Ruud, E.A.; Ashraf, H. Elevated d-dimer cut-off values for computed tomography pulmonary angiography—d-dimer correlates with location of embolism. Ann. Transl. Med. 2016, 4, PMC4916352. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sikora-Skrabaka, M.; Skrabaka, D.; Ruggeri, P.; Caramori, G.; Skoczyński, S.; Barczyk, A. D-dimer value in the diagnosis of pulmonary embolism—May it exclude only? J. Thorac. Dis. 2019, 11, 664–672. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.A.; Davis, S.D.; Gamsu, G.; Intriere, L. Parenchymal and Pleural Findings in Patients with and Patients without Acute Pulmonary Embolism Detected at Spiral CT. Radiology 1999, 211, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Karabulut, N.; Kıroğlu, Y. Relationship of parenchymal and pleural abnormalities with acute pulmonary embolism: CT findings in patients with and without embolism. Diagn. Interv. Radiol. 2008, 14, 189–196. [Google Scholar]
- Coche, E.E.; Müller, N.L.; Kim, K.I.; Wiggs, B.R.; Mayo, J.R. Acute pulmonary embolism: Ancillary findings at spiral CT. Radiology 1998, 207, 753–758. [Google Scholar] [CrossRef]
- De Monyé, W.; Sanson, B.-J.; Mac Gillavry, M.R.; Pattynama, P.M.T.; Büller, H.R.; Van Den Berg-Huysmans, A.A.; Huisman, M.V. Embolus Location Affects the Sensitivity of a Rapid Quantitative d-dimer Assay in the Diagnosis of Pulmonary Embolism. Am. J. Respir. Crit. Care Med. 2002, 165, 345–348. [Google Scholar] [CrossRef]
- Yu, J.; Li, D.; Lei, D.; Yuan, F.; Pei, F.; Zhang, H.; Yu, A.; Wang, K.; Chen, H.; Chen, L.; et al. Tumor-Specific D-Dimer Concentration Ranges and Influencing Factors: A Cross-Sectional Study. PLoS ONE 2016, 11, e0165390. [Google Scholar] [CrossRef] [Green Version]
- Grau, E.; Tenías, J.M.; Soto, M.J.; Gutierrez, M.R.; Lecumberri, R.; Pérez, J.L.; Tiberio, G. D-dimer levels correlate with mortality in patients with acute pulmonary embolism: Findings from the RIETE registry. Crit. Care Med. 2007, 35, 1937–1941. [Google Scholar] [CrossRef]
- Polo Friz, H.; Buzzini, C.; Orenti, A.; Punzi, V.; Molteni, M.; Primitz, L.; Cavalieri d’Oro, L.; Arpaia, G.; Boracchi, P.; Cimminiello, C. Prognostic value of D-dimer in elderly patients with Pulmonary Embolism. J. Thromb. Thrombolysis 2016, 42, 386–392. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Presence of PE (n,%) | Absence of PE (n, %) | p Value |
|---|---|---|---|
| Number of patients | 190 (18.7) | 827 (81.3) | |
| Age, mean (SD) | 64.1 (16.1) | 63.6(16.5) | 0.703 |
| Gender | |||
| Males | 106 (55.8) | 443 (52.7) | 0.579 |
| Females | 84 (44.2) | 384 (45.7) | |
| D-dimer, median (IQR) | 3.16 (1.85–7.82) | 1.53 (0.83–2.87) | <0.001 |
| RDW median (IQR) 1 | 13.7 (12.5–15.2) | ||
| CTPA Findings | |||
| Normal pleuro-parenchymal findings | 34 (17.9) | 191 (23.1) | 0.119 |
| Consolidation/Atelectasis | 76 (40) | 255 (30.8) | 0.015 |
| Infiltrate/GGO/Wedge-shaped opacity | 37 (19.5) | 157 (19) | 0.877 |
| Nodule/Mass | 37 (19.5) | 133 (16) | 0.259 |
| Pulmonary fibrosis | 9 (4.7) | 46 (5.6) | 0.650 |
| Mosaic attenuation | 10 (5.3) | 34 (4.1) | 0.482 |
| Advanced emphysema | 12 (6.3) | 69 (8.3) | 0.352 |
| Advanced bronchiectasis | 13 (6.8) | 91 (11) | 0.088 |
| Pleural effusion | |||
| Unilateral | 55 (29) | 172 (20.8) | 0.043 |
| Bilateral | 23 (12.1) | 127 (15.3) | |
| Hospitalization (days), mean (SD) 1 | 13.2 (9.0) | ||
| Outcome 1 | |||
| Improvement | 142 (74.73) | ||
| Death | 16 (8.4) |
| Variates | D-Dimer Median (IQR) | p Value | RDW 1 Median (IQR) | p Value |
|---|---|---|---|---|
| PE | ||||
| Bilateral | 2.20 (1.40–3.58) | <0.001 | 13.56 (12.6–14.60) | 0.983 |
| Unilateral | 5.50 (3.04–11.89) | 13.7 (12.43–15.20) | ||
| PE | ||||
| Peripheral | 2.10 (1.21–3.42) | <0.001 | 13.60 (12.41–14.46) | 0.730 |
| Central | 5.93 (3.04–12.27) | 13.58 (12.59–15.40) | ||
| PE | ||||
| Single Embolus | 2.19 (1.56–3.16) | 0.013 | 13.67 (12.55–14.30) | 0.824 |
| Multiple Emboli | 3.60 (1.99–8.56) | 13.52 (12.43–15.23) | ||
| Normal pleuro-parenchymal findings | 1.05 (0.61–2.17) | <0.001 | 13.75 (12.43–15.20) | 0.787 |
| Any parenchymal abnormality | 1.97 (1.09–3.53) | 13.6 (12.59–14.60) | ||
| Consolidation/Atelectasis | ||||
| Present | 2.34 (1.29–4.22) | <0.001 | 12.95 (12.03–14.44) | 0.020 |
| Absent | 1.59 (0.81–2.96) | 13.75 (12.80–15.20) | ||
| Infiltrate/GGO/Wedge-shaped opacity | ||||
| Present | 1.85 (0.96–3.10) | 0.476 | 13.29 (12.59–14.44) | 0.435 |
| Absent | 1.74 (0.91–3.32) | 13.70 (12.43–15.23) | ||
| Nodule/Mass | ||||
| Present | 2.39 (1.45–4.45) | <0.001 | 13.87 (13.48–17.40) | 0.118 |
| Absent | 1.66 (0.84–3.12) | 13.51 (12.41–14.60) | ||
| Pulmonary Fibrosis | ||||
| Present | 1.22 (0.76–2.96) | 0.245 | 17.20 (15.60–18.80) | 0.059 |
| Absent | 1.8 (0.93–3.32) | 13.60 (12.43- 14.60) | ||
| Mosaic Attenuation | ||||
| Present | 1.97 (1.31–2.98) | 0.585 | 14.16 (12.65–18.6) | 0.249 |
| Absent | 1.73 (0.91–3.32) | 13.56 (12.43–14.6) | ||
| Advanced Emphysema | ||||
| Present | 1.18 (0.78–2.37) | 0.046 | 13.60 (12.43–16.40) | 0.837 |
| Absent | 1.80 (0.94–3.41) | 13.62 (12.47–14.85) | ||
| Advanced Bronchiectasis | ||||
| Present | 1.27 (0.83–2.11) | 0.004 | 14.23 (12.59–15.10) | 0.983 |
| Absent | 1.85 (0.94–3.49) | 13.60 (12.43–14.60) | ||
| Pleural effusion | ||||
| Unilateral | 2.41 (1.51–4.42) | <0.001 | 13.00 (12.24–13.70) | 0.085 |
| Bilateral | 2.56 (1.11–3.60) | 14.12 (13.34–16.03) | ||
| Outcome1 | ||||
| Improvement | 3.04 (1.78–8.04) | 0.474 | 13.48 (12.41–14.50) | 0.012 |
| Death | 3.95 (3.16–5.50) | 15.50 (14.04–16.50) |
| Conventional Cutoff Point (0.5 mg/L) | Age-Adjusted Cutoff Point | Cutoff Point (2.1 mg/L) with the Best Specificity Based on ROC. AUC (95% CI) 0.72 (0.67–0.77) | Proposed Cutoff Point (0.74 mg/L) | |
|---|---|---|---|---|
| Sensitivity % | 98.2 | 98.2 | 70.8 | 97.3 |
| (95% CI) | (93.8–99.8) | (93.8–99.8) | (61.5–79.0) | (92.7–99.1) |
| Specificity % | 7.9 | 13.1 | 64.4 | 20.5 |
| (95% CI) | (5,8–10,8) | (10.2–16.4) | (60–68.6) | (16.4–23.7) |
| PPV % | 19.5 | 20.4 | 31.1 | 21.8 |
| (95% CI) | (16.4–23.1) | (17.1–24.1) | (25.5–37.2) | (17.3–24.6) |
| NPV % | 95.2 | 97.0 | 90.7 | 97.1 |
| (95% CI) | (83.8–99.4) | (89.6–99.6) | (87.1–93) | (89.7–99.6) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chrysikos, S.; Papaioannou, O.; Karampitsakos, T.; Tavernaraki, K.; Thanou, I.; Filippousis, P.; Anyfanti, M.; Hillas, G.; Tzouvelekis, A.; Thanos, L.; et al. Diagnostic Accuracy of Multiple D-Dimer Cutoff Thresholds and Other Clinically Applicable Biomarkers for the Detection and Radiographic Evaluation of Pulmonary Embolism. Adv. Respir. Med. 2022, 90, 300-309. https://doi.org/10.3390/arm90040039
Chrysikos S, Papaioannou O, Karampitsakos T, Tavernaraki K, Thanou I, Filippousis P, Anyfanti M, Hillas G, Tzouvelekis A, Thanos L, et al. Diagnostic Accuracy of Multiple D-Dimer Cutoff Thresholds and Other Clinically Applicable Biomarkers for the Detection and Radiographic Evaluation of Pulmonary Embolism. Advances in Respiratory Medicine. 2022; 90(4):300-309. https://doi.org/10.3390/arm90040039
Chicago/Turabian StyleChrysikos, Serafeim, Ourania Papaioannou, Theodoros Karampitsakos, Kyriaki Tavernaraki, Ioanna Thanou, Petros Filippousis, Maria Anyfanti, Georgios Hillas, Argyrios Tzouvelekis, Loukas Thanos, and et al. 2022. "Diagnostic Accuracy of Multiple D-Dimer Cutoff Thresholds and Other Clinically Applicable Biomarkers for the Detection and Radiographic Evaluation of Pulmonary Embolism" Advances in Respiratory Medicine 90, no. 4: 300-309. https://doi.org/10.3390/arm90040039
APA StyleChrysikos, S., Papaioannou, O., Karampitsakos, T., Tavernaraki, K., Thanou, I., Filippousis, P., Anyfanti, M., Hillas, G., Tzouvelekis, A., Thanos, L., & Dimakou, K. (2022). Diagnostic Accuracy of Multiple D-Dimer Cutoff Thresholds and Other Clinically Applicable Biomarkers for the Detection and Radiographic Evaluation of Pulmonary Embolism. Advances in Respiratory Medicine, 90(4), 300-309. https://doi.org/10.3390/arm90040039






