1. Introduction
Geriatric neurosurgery has its own challenges and unique characteristics, as it involves treating older patients who are more prone to stress [
1,
2]. This stress results from the combination of aging, immobility, acute illness, complications from hospitalization, and slower healing. These factors make elderly patients more vulnerable to complications, so a multidisciplinary team is usually brought together to improve their quality of life and help them maintain independence [
3].
TBI is a significant public health concern, particularly among individuals aged 65 and above, accounting for more than 80,000 emergency visits annually in the United Kingdom alone [
3,
4]. TBI outcomes in the elderly are generally poor, with mortality rates for severe TBI ranging from 30% to 80% in this age group. Among all types of traumatic injuries, TBI is a leading cause of disability and death. There have been a few studies exploring TBI cases across this aging group in the last few years [
5]. Some of these studies highlight that the most commonly seen presentation among geriatric TBI is subdural hematoma and also explore rates of neurosurgical interventions and ICU admissions [
6].
Several studies have identified factors that influence the prognosis of patients with TBI [
7,
8]. A one-year study conducted in India in 2004 highlighted the importance of early recognition, resuscitation, triage, prompt computed tomography (CT) scanning, and aggressive surgical management in improving outcomes. Similarly, a retrospective study on elderly TBI patients identified additional predictors of poor outcomes, including TBI severity, pupillary reactivity, coagulation status, the need for blood product transfusions, and acute bleeding.
There has been an ongoing debate about the best time to perform surgical interventions [
1,
9]. Studies suggest that surgeries performed in TBI cases during the day tend to have fewer medical errors and human factors that could affect the procedure and its outcome compared to surgeries performed during on-call times. At night, factors like staff exhaustion and limited resources increase the risk of complications during and after surgery, which can negatively impact the patient’s recovery [
1].
Additionally, the timing of surgery and the occurrence of postoperative complications depend on several factors, including the type of surgery, the patient’s age and general health, and any intraoperative events [
2]. For TBI, surgeries are often lifesaving, especially in emergencies like extradural hemorrhage or decompression. Some researchers believe that daytime surgeries, when all resources are available and proper preoperative preparation is in place, result in better outcomes and fewer complications than those performed at night. Surgery timing contributes to TBI post-operative outcomes.
This study aims to compare the types of surgical interventions (such as burr holes and craniotomies) and their effectiveness (including length of stay and complications) in TBI patients treated during the daytime versus those treated at on-call times. The definition of the geriatric age group in Oman and the region includes only those older than 65 years old.
3. Results
Based on the inclusion and exclusion criteria, our study includes twenty patients admitted during daytime and twenty-five patients admitted on-call between 2015 and 2019, as outlined in
Table 1. Due to a controlled sample size,
p-value interpretations would need some discretion. The average ages of the patients in the daytime and on-call groups were 76.40 and 77.60 years, respectively [
1]. Among the twenty daytime admissions, the male-to-female ratio was 4:1, whereas in the twenty-five on-call admissions, the ratio was 3.17:1 [
2]. Approximately 47.6% of the patients admitted during daytime were under 75 years old, while 41.7% were over 75 [
3].
Table 2 presents the types of admissions and GCS scores at the time of admission. Of note, 96% of on-call surgeries were emergencies, in contrast to one-third of daytime surgeries, which were emergencies [
4]. Five percent of patients were comatose upon daytime admission, compared to 28% among the on-call group [
12].
The diagnoses for the admissions included in our study are shown in
Table 3. Among daytime cases, the most common diagnosis was SDH during both periods.
Table 4 shows that the average length of stay (LOS) was 11.60 days for patients who underwent surgery during the daytime, compared to 29.44 days for those operated on during on-call hours. This illustrates a 2.5 times longer stay for on-call patients compared to daytime patients. For patients admitted to the ICU after surgery, there was a 9.9-fold increase in ICU stay for on-call patients compared to daytime.
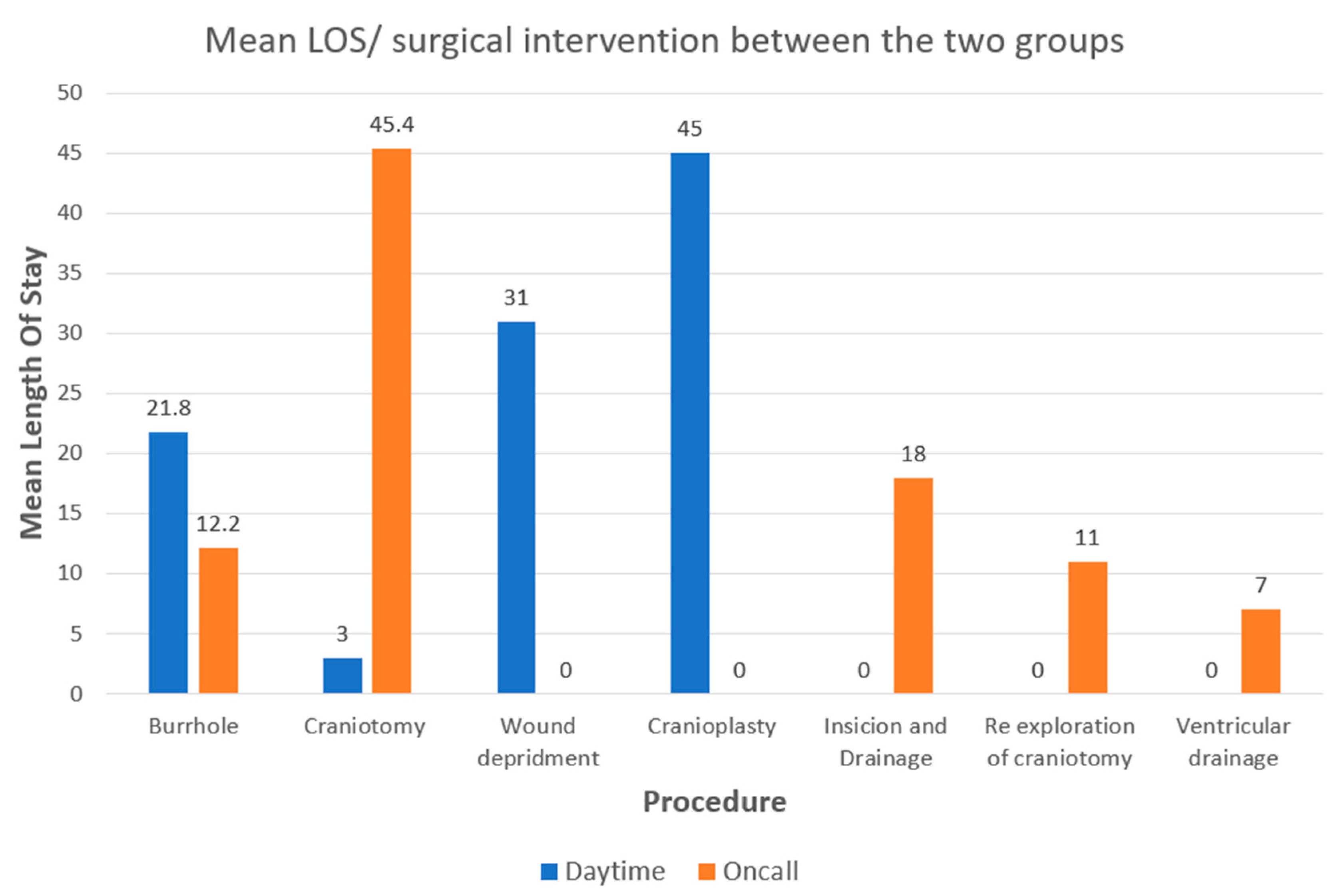
Table 5 outlines the types and frequencies of surgical interventions performed in our study. The most common procedure during the daytime was burr holes. During on-call, craniotomy was the most common procedure during on-call.
We also compared the GCS scores at discharge, as shown in
Table 6. Five percent of patients who underwent daytime surgery had low GCS scores upon discharge, whereas 44% of on-call patients had low GCS scores. The rate of patients who fell into a coma following surgery was 8.8 times higher in the daytime group compared to the on-call group.
Statistics in
Table 7 reveal that postoperative infections occurred four times more frequently in patients who underwent surgery during on-call hours than in those who had daytime surgery. Post-operative complications were 475% more common among on-call patients.
Figure 1 demonstrates that, on average, patients who had burr holes during daytime surgery stayed 78.69% longer in the hospital than those who had the procedure during on-call hours. The hospital stay following craniotomy was 94.2% longer for on-call patients compared to daytime patients.
During the daytime, no cases of deterioration were recorded. As a result, the graph shows only one line for the on-call.
4. Discussion
This is the first study to compare the outcomes of postoperative complications among geriatric patients with TBI [
10]. No conflicts of interest were reported.
Statistics reveal that the global population is steadily aging, and by 2060, 18% of people worldwide will be 65 years or older [
7]. In Oman, from 2013 to 2017, the population over 75 years of age grew by 15.4%, underscoring the need for effective healthcare for this aging demographic [
8].
Our study involved 45 patients admitted to KH between 2015 and 2019, with a majority of 35 patients being male. Notably, 58.3% of patients admitted during on-call hours and 41.7% of those admitted during the daytime were over 75 years old [
9]. The average age of all 45 patients in the study was 77.07 years [
10].
The majority of elective admissions, over 90%, occurred during daytime hours, while only about 6% took place during on-call hours. This significant difference, with a p-value of <0.05, underscores that more elective admissions happen during the day, likely because more healthcare providers are available to manage these cases during regular working hours.
In contrast, 82% of emergency admissions occurred during on-call hours, compared to just 17% during the daytime. The data was highly significant (95%), with a p-value of <0.05, indicating a strong trend. While emergency admissions can happen at any time, the likelihood of urgent TBI cases arising during on-call hours is nearly twice as high as during daytime hours. This is largely because the on-call period lasts longer, allowing for more potential emergencies. These data (p < 0.05) show an association between on-call hours and a higher frequency of urgent TBI cases, possibly due to the longer duration of on-call periods and the resulting increased opportunity for emergencies, but causality cannot be inferred.
However, there was no significant difference in the GCS scores between patients admitted during daytime and on-call hours (p-value = 0.059), with most patients presenting with GCS scores higher than 8, suggesting that most patients were not in a severely comatose state upon admission.
In terms of primary diagnosis, the types of TBI most commonly seen in our study were similar for both daytime and on-call admissions. For instance, 70% of patients admitted during the daytime had SDH, while 64% of on-call patients were also diagnosed with SDH [
6]. Other diagnoses included multi-compartmental bleeding, which was more common during daytime, and intracranial hemorrhage, which was more prevalent during on-call admissions.
The results of our study also showed that both the length of hospital stay and the duration of ICU stay were significantly longer for on-call admissions compared to daytime admissions, leading to delayed care and extended recovery. This likely reflects the fact that fewer medical personnel, diagnostic resources, and facilities are available during on-call hours, leading to less immediate attention and a longer recovery period for patients admitted during this time [
13].
Additionally, there were fewer minimally invasive procedures, such as burr holes, performed during on-call admissions compared to daytime-admitted TBI cases. On-call patients were 13 times more likely to undergo invasive procedures like craniotomies, suggesting that fewer specialists trained in performing burr holes were available during on-call hours.
In terms of patient outcomes, our study found that 5% of daytime surgery patients had low GCS scores post-operatively, while 44% of on-call patients had low GCS scores following surgery. This indicates that patients were 8.8 times more likely to fall into a coma after being treated at on-call time. This represents a dramatic increase in the likelihood of poorer post-operative outcomes for patients treated during on-call hours.
Post-operative infection rates were found to be four times higher among patients who underwent surgery during on-call hours compared to those who had surgery during the daytime. Additionally, there was a 475% increase in overall postoperative complications, such as surgical site infections, patient deterioration, reoperations, and hemodynamic instability, among on-call patients. While none of the patients in our study developed DVT after surgery, 25% of the on-call patients’ conditions deteriorated following surgical interventions, while none of the daytime patients showed similar complications.
The length of stay in the hospital was consistently longer for on-call patients, which may be attributed to the smaller number of available surgical interventions and medical resources during on-call time hours. Blood pressure levels recorded in on-call patients were more unstable compared to those admitted during the daytime, reflecting the additional challenges of managing these patients under limited staffing and equipment. These findings likely reflect fewer medical personnel, diagnostic resources, and specialists during on-call hours, leading to delayed care and extended recovery, though causality cannot be confirmed.
Potential biases include selection bias, as the single-center design and small sample may not represent the broader geriatric TBI population. Data recording bias may arise from inconsistent documentation during understaffed on-call hours. Unmeasured factors, like comorbidities or pre-hospital care, could also affect results. The lack of significant GCS score differences suggests initial injury severity may not fully explain outcome disparities, but further study is needed.
Prospective research is needed to confirm these findings in larger, multicenter studies with standardized data collection to reduce bias and account for factors like injury severity and comorbidities. Specific interventions include increasing neurosurgical and diagnostic resources during on-call hours for timely, minimally invasive procedures; implementing uniform TBI management protocols; strengthening postoperative monitoring during on-call periods to reduce complications; and providing regular training for on-call teams to improve expertise in complex TBI cases [
14].
Lastly, this study identifies significant associations between on-call admissions and poorer outcomes in geriatric TBI patients, including longer stays, higher complication rates, and worse postoperative GCS scores. However, causality cannot be confirmed due to potential biases. Prospective studies and targeted interventions are critical to improving care for this growing demographic.
Limitations
Our understanding comes from data collected on elderly TBI cases treated at KH over five years. This was a cross-sectional, retrospective study. Given the total population of the country and the moderate number of patients presenting to KH Neurosurgery, the overall patient pool was limited. Furthermore, the application of strict inclusion and exclusion criteria resulted in a relatively small final sample size of 45 cases.
Several factors may have affected the results, such as the number of trauma care staff and imaging machines available during on-call hours, how many hours into their shift the doctors and surgeons were when treating TBI cases, and the availability of ICU facilities.
In this study, we managed to explore the length of stay among modalities that examine the timing and sequencing of clinical events to evaluate quality of care, outcomes, and efficiency. However, data of certain modalities that could have been beneficial in understanding the quality of care, such as time-to-diagnosis, time-to-intervention, time-to-consult, etc., were not recorded and hence, not included in our study.
Several confounding factors were successfully addressed in our study. Moreover, at the same time, there were some factors we couldn’t account for. This included pupil reactivity, CT findings, the number of ORs, and ICU bed availability.
Future studies on this topic should be conducted to explore any improvements or declines, taking these factors into account.