ComPAIN—Communication of Pain in Patients with Headache
Abstract
1. Introduction
1.1. Primary Headaches According to ICHD-3
1.2. Sex Differences in Pain Perception and Communication
2. Materials and Methods
3. Statistical Analysis
4. Results
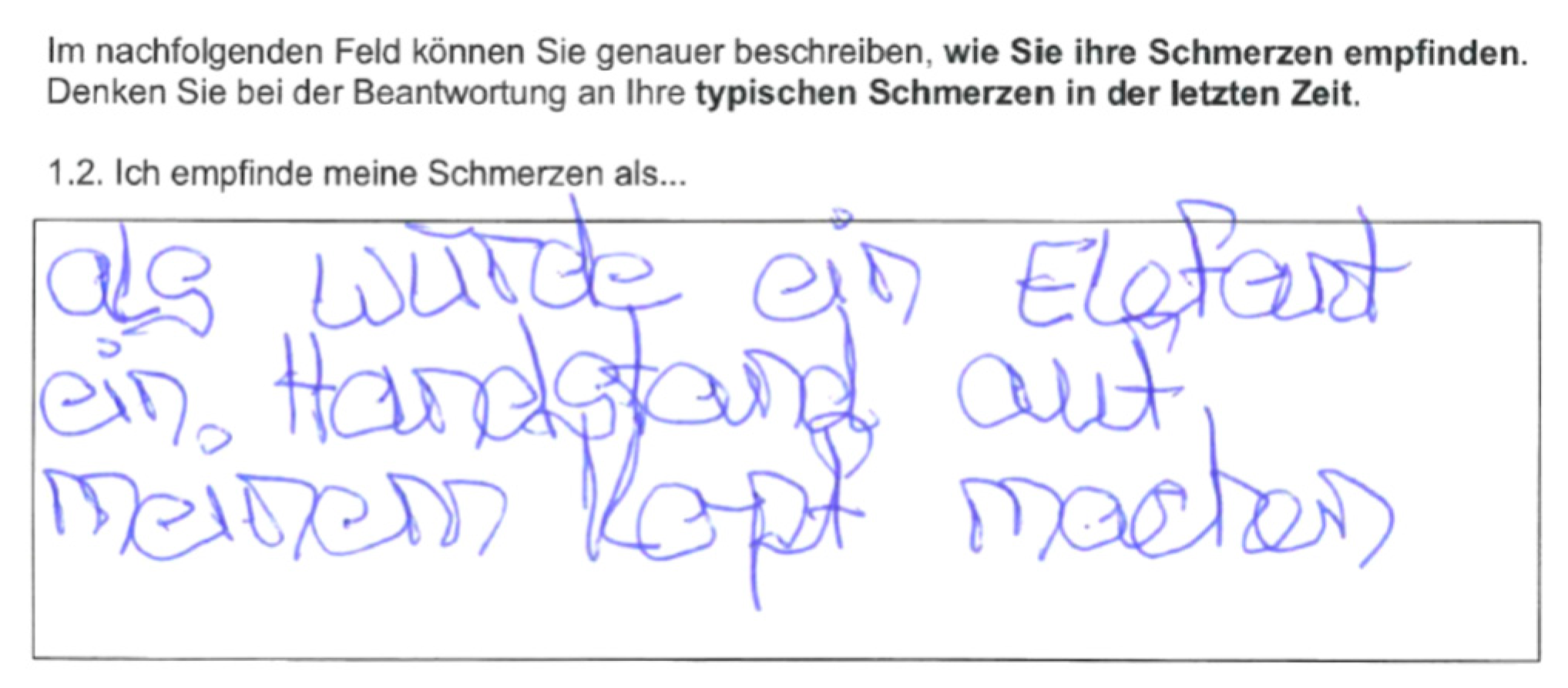
4.1. Results from Questionnaire Q1
4.2. Results from Pain Description (Task Q1) and Final Medical Report
“Dumpf und pulsierend gleichzeitig. So lange ich mich gar nicht bewege, kein Augenzwinkern, rein gar nichts, und sich auch meine Unterlage (Bett) nicht bewegt, ist es einigermassen auszuhalten. Aber fast schon ein Atemzug von jemand im Zimmer oder einer Fingerrührung meinerseits, kann meinen Kopf bei sehr starker Migräne fast zum Platzen bringen”.
- Citation 1: Description of pain. Free description of a patient’s headache in the Q1. Example of a first-person narrative’s use, placing oneself as the subject. This patient was diagnosed with a migraine. (Translation: «Dull and pulsating at the same time. As long as I don’t move at all, don’t blink my eyes, nothing at all, and my mattress doesn’t move either, it is quite bearable. But almost a breath from someone in the room or a finger movement from my part, can almost make my head burst with very severe migraines».)
“Im Alltag einschränkend. Die Schmerzen sind meist pulsierend mit einem gewissen Druck. Oftmals treten diese mit starken Nacken- und Oberrückenschmerzen auf. Manchmal sind die Schmerzen beidseitig und manchmal einseitig”.
- Citation 2: Description of pain. Free description of a patient’s headache in the questionnaire Q1. Example of third-person narrative and objectification of the pain. This patient was diagnosed with a mixed form of migraine and TTH. (Translation: «Restrictive in everyday life. The pain is usually pulsating with some pressure. It often occurs with severe neck and upper back pain. Sometimes the pain is bilateral and sometimes unilateral».)
4.3. Results from Questionnaire Q2
5. Discussion
6. Limitations
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A


References
- Robbins, M.S.; Lipton, R.B. The Epidemiology of Primary Headache Disorders. Semin. Neurol. 2010, 30, 107–119. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Chen, X.; Fan, Y. Biomarkers in migraine beyond diagnosis. Front. Neurol. 2022, 13, 1096531. [Google Scholar] [CrossRef] [PubMed]
- Lipton, R.B.; Stewart, W.F.; Celentano, D.D.; Reed, M.L. Undiagnosed migraine headaches: A comparison of symptom-based and reported physician diagnosis. Arch. Intern. Med. 1992, 152, 1273–1278. [Google Scholar] [CrossRef] [PubMed]
- Arnold, M. Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition. Cephalalgia 2018, 38, 1–211. [Google Scholar]
- Friedman, B.W.; Hochberg, M.L.; Esses, D.; Grosberg, B.; Corbo, J.; Toosi, B.; Meyer, R.H.; Bijur, P.E.; Lipton, R.B.; Gallagher, E.J. Applying the International Classification of Headache Disorders to the emergency department: An assessment of reproducibility and the frequency with which a unique diagnosis can be assigned to every acute headache presentation. Ann. Emerg. Med. 2007, 49, 409–419.e9. [Google Scholar] [CrossRef] [PubMed]
- Kalitzkus, V.; Matthiessen, P.F. Narrative-based medicine: Potential, pitfalls, and practice. Perm. J. 2009, 13, 80. [Google Scholar] [CrossRef] [PubMed]
- Vos, T.; Abajobir, A.A.; Abate, K.H.; Abbafati, C.; Abbas, K.M.; Abd-Allah, F.; Abdulkader, R.S.; Abdulle, A.M.; Abebo, T.A.; Abera, S.F.; et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1211–1259. [Google Scholar] [CrossRef] [PubMed]
- Mier, R.W.; Dhadwal, S. Primary headaches. Dent. Clin. 2018, 62, 611–628. [Google Scholar] [CrossRef] [PubMed]
- Bartley, E.J.; Fillingim, R.B. Sex differences in pain: A brief review of clinical and experimental findings. BJA Br. J. Anaesth. 2013, 111, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Wiesenfeld-Hallin, Z. Sex differences in pain perception. Gend. Med. 2005, 2, 137–145. [Google Scholar] [CrossRef]
- Kim, J.A.; Bosma, R.L.; Hemington, K.S.; Rogachov, A.; Osborne, N.R.; Cheng, J.C.; Dunkley, B.T.; Davis, K.D. Sex-differences in network level brain dynamics associated with pain sensitivity and pain interference. Hum. Brain Mapp. 2021, 42, 598–614. [Google Scholar] [CrossRef] [PubMed]
- Alabas, O.A.; Tashani, O.A.; Tabasam, G.; Johnson, M.I. Gender role affects experimental pain responses: A systematic review with meta-analysis. Eur. J. Pain 2012, 16, 1211–1223. [Google Scholar] [CrossRef] [PubMed]
- Riecher-Rössler, A.; Butler, S.; Kulkarni, J. Sex and gender differences in schizophrenic psychoses—A critical review. Arch. Women’s Ment. Health 2018, 21, 627–648. [Google Scholar] [CrossRef] [PubMed]
- Neumeier, M.S.; Pohl, H.; Sandor, P.S.; Gut, H.; Merki-Feld, G.S.; Andrée, C. Dealing with Headache: Sex Differences in the Burden of Migraine-and Tension-Type Headache. Brain Sci. 2021, 11, 1323. [Google Scholar] [CrossRef] [PubMed]
- Krone-Germann, I. Part-Time Employment in Switzerland; PIE-Peter Lang SA: Ixelles, Belgium, 2011. [Google Scholar]
- Hall, J.A.; Dornan, M.C. Patient sociodemographic characteristics as predictors of satisfaction with medical care: A meta-analysis. Soc. Sci. Med. 1990, 30, 811–818. [Google Scholar] [CrossRef] [PubMed]
- Elston, D.M. Confirmation bias in medical decision-making. J. Am. Acad. Dermatol. 2020, 82, 572. [Google Scholar] [CrossRef] [PubMed]
| All n = 35 | Male n = 13 | Female n = 22 | p-Value | |
|---|---|---|---|---|
| Demographic data | ||||
| Age, y (range) | 29 (18–61) | 39 (19–53) | 25 (18–61) | 0.085 |
| Headache Type | ||||
| Migraine, n (%) | 21 (60.00%) | 5 (38.46%) | 16 (72.73%) | 0.030 |
| TTH, n (%) | 5 (14.29%) | 4 (30.77%) | 1 (04.55%) | |
| Migraine & TTH, n (%) | 7 (20.00%) | 2 (15.38%) | 5 (22.73%) | |
| TAC, n (%) | 1 (02.86%) | 1 (07.69%) | 0 (00.00%) | |
| Other, n (%) | 1 (02.86%) | 1 (07.69%) | 0 (00.00%) | |
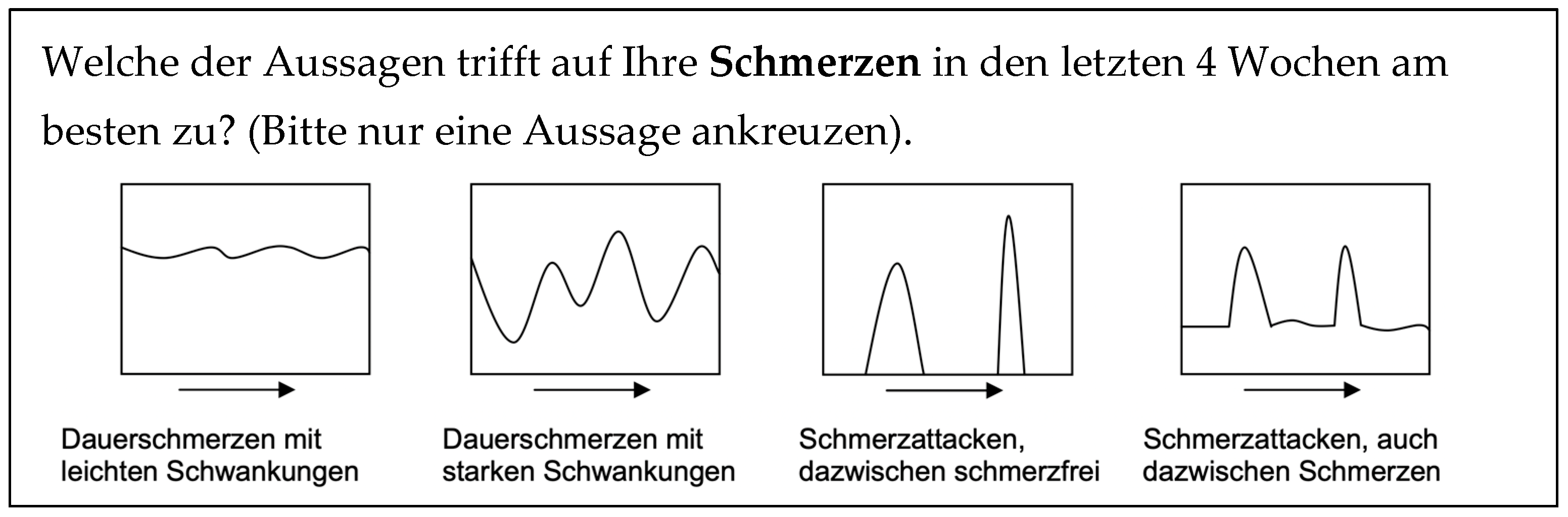
| Temporal trend | ||||
| Constant pain with light fluctuations, n (%) (participants) | 9 (26.47%) (34/35) | 5 (38.46%) (13/13) | 4 (19.05%) (21/22) | 0.742 |
| Constant pain with severe fluctuations, n (%) (participants) | 9 (26.47%) (34/35) | 4 (30.77%) (13/13) | 5 (23.81%) (21/22) | |
| Pain attacks, in between pain-free, n (%) (participants) | 12 (35.29%) (34/35) | 3 (23.08%) (13/13) | 9 (42.86%) (21/22) | |
| Pain attacks, with pain in between, n (%) (participants) | 6 (17.65%) (34/35) | 2 (15.38%) (13/13) | 4 (19.05%) (21/22) | |
| Loss of days/3 months | ||||
| No. of workdays a, n (range) (participants) | 3 (0–45) (30/35) | 0 (0–45) (13/13) | 3 (0–30) (17/22) | 0.229 |
| Less 50% workdays a, n (range) (participants) | 8 (0–90) (30/35) | 5 (0–90) (13/13) | 10 (0–40) (17/22) | 0.509 |
| No. of household days a, n (range) (participants) | 3 (0–67.5) (31/35) | 0 (0–67.5) (13/13) | 5 (0–50) (18/22) | 0.106 |
| Less than 50% household days a, n (range) (participants) | 5 (0–90) (31/35) | 2 (0–90) (12/13) | 6 (0–35) (19/22) | 0.535 |
| No. of social days a, n (range) (participants) | 5 (0–70) (33/35) | 4 (0–45) (13/13) | 7 (0–70) (20/22) | 0.030 |
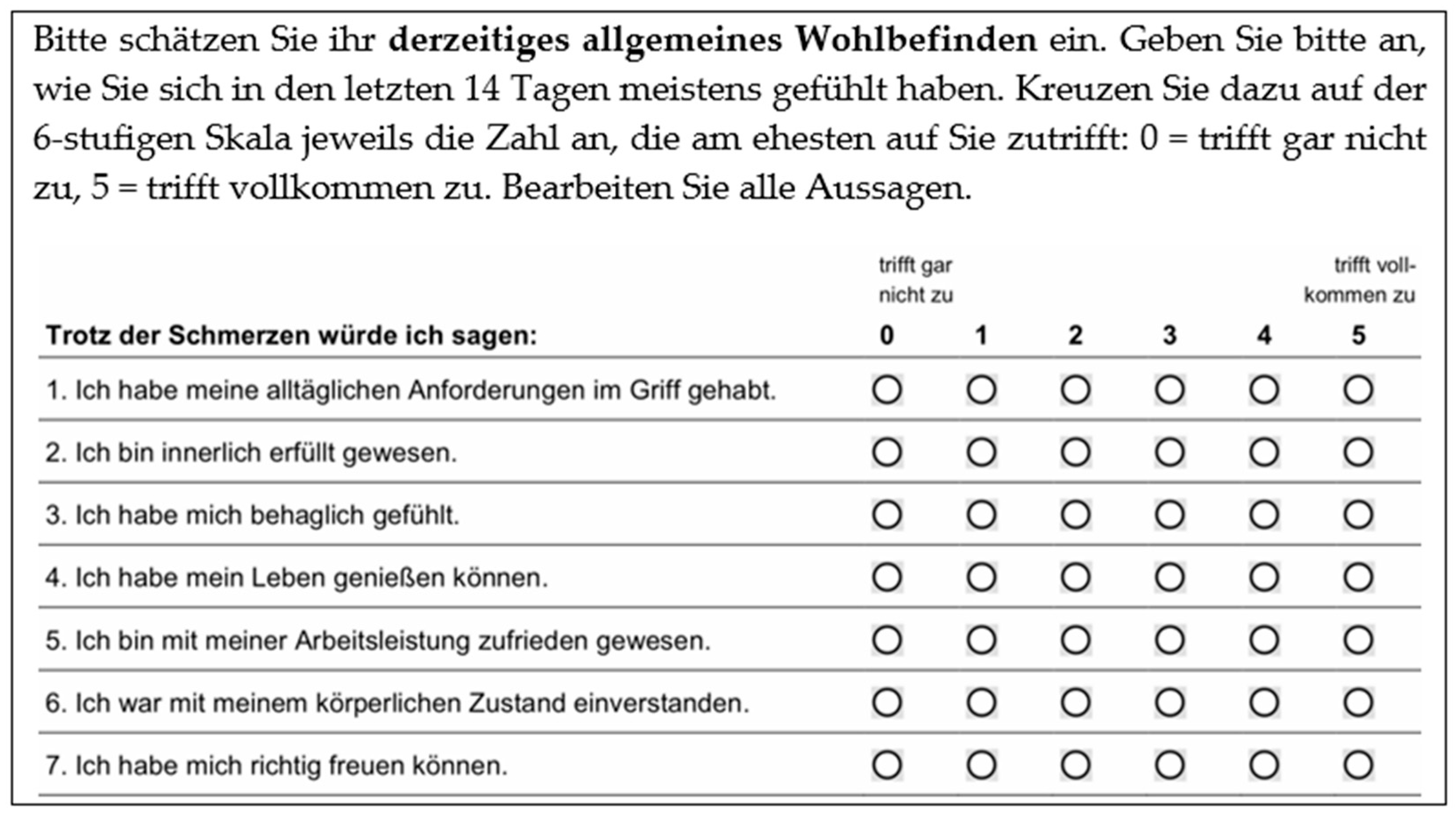
| Well-being | ||||
| General well-being (points) b (participants) | 21 (6–29) (31/35) | 22.5 (6–29) (12/13) | 21 (6–25) (19/22) | 0.412 |
| All n = 35 | Male n = 13 | Female n = 22 | p-Value | |
|---|---|---|---|---|
| Pain Communication | ||||
| Number of words for pain description, n (range) (participants) | 11 (01–92) (33/35) | 11 (01–25) (13/13) | 12 (03–92) (20/22) | 0.870 |
| First-person narrative, n (%) (participants) | 8 (24.24%) (33/35) | 2 (15.38%) (13/13) | 6 (30.00%) (20/22) | 0.431 |
| All n = 35 | Migraine n = 21 | No Migraine n = 14 | p-Value | |
|---|---|---|---|---|
| Adjective defining migraine according to ICHD-3 | ||||
| Pulsating/“pulsierend”, n (%) (participants) | 9 (27.27%) (33/35) | 4 (20.00%) (20/21) | 5 (38.46%) (13/14) | 0.424 |
| Adjective defining TTH according to ICHD-3 | ||||
| Tightening/“beengend”, n (%) (participants) | 1 (03.03%) (33/35) | 1 (25.00%) (20/21) | 0 (00.00%) (13/14) | 1.000 |
| Pressing/“drückend”, n (%) (participants) | 18 (54.55%) (33/35) | 14 (70.00%) (20/21) | 4 (30.77%) (13/14) | 0.038 |
| Patient ID | Pulsating (Pulsierend) | Constricting (Beengend) | Pressing (Drückend) | Stabbing (Stechend) | Dull (Dumpf) | Dragging (Ziehend) | Burning (Brennend) | % Concordance a | Sex |
|---|---|---|---|---|---|---|---|---|---|
| 9 | XX | 100.00 | female | ||||||
| 17 | XX | XX | XX | 100.00 | female | ||||
| 19 | XX | 100.00 | female | ||||||
| 20 | XX | XX | 100.00 | male | |||||
| 21 | XX | XX | 100.00 | female | |||||
| 25 | XX | 100.00 | female | ||||||
| 1 | X | XX | 50.00 | female | |||||
| 8 | XX | X | 50.00 | female | |||||
| 16 | X | XX | 50.00 | male | |||||
| 27 | X | XX | 50.00 | male | |||||
| 29 | XX | X | 50.00 | male | |||||
| 31 | X | XX | 50.00 | female | |||||
| 34 | X | XX | 50.00 | female | |||||
| 22 | X | X | XX | X | XX | 40.00 | female | ||
| 12 | X | X | XX | 33.33 | female | ||||
| 28 | XX | XX | X | 33.33 | female | ||||
| 24 | X | X | XX | X | 25.00 | female | |||
| 4 b | X | 00.00 | female | ||||||
| 5 b | X | 00.00 | female | ||||||
| 11 b | X | 00.00 | male | ||||||
| 33 b | X | 00.00 | female |
| All n = 35 | Male n = 13 | Female n = 22 | p-Value | |
|---|---|---|---|---|
| Satisfaction with consultation, points a, (range) (participants) | 26 (10–28) (31/35) | 24 (10–28) (13/13) | 27 (22–28) (18/22) | 0.028 |
| Regression Model Satisfaction a | Variable | Regression Coefficient | 95% Confidence Interval | p-Value |
| Age Sex Headache | 0.442 12.497 1.403 | 0.301–0.583 8.460–16.533 −0.744–3.549 | <0.001 <0.001 0.191 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Eicher, E.; Räz, S.; Stucki, P.; Röthlin, C.; Stattmann, M.; Grossenbacher, B.; Neumann, E.; Pohl, H.; Ilg, Y.; Maatz, A.; et al. ComPAIN—Communication of Pain in Patients with Headache. Clin. Transl. Neurosci. 2023, 7, 14. https://doi.org/10.3390/ctn7020014
Eicher E, Räz S, Stucki P, Röthlin C, Stattmann M, Grossenbacher B, Neumann E, Pohl H, Ilg Y, Maatz A, et al. ComPAIN—Communication of Pain in Patients with Headache. Clinical and Translational Neuroscience. 2023; 7(2):14. https://doi.org/10.3390/ctn7020014
Chicago/Turabian StyleEicher, Emma, Sabina Räz, Pascale Stucki, Cinzia Röthlin, Miranda Stattmann, Bettina Grossenbacher, Eileen Neumann, Heiko Pohl, Yvonne Ilg, Anke Maatz, and et al. 2023. "ComPAIN—Communication of Pain in Patients with Headache" Clinical and Translational Neuroscience 7, no. 2: 14. https://doi.org/10.3390/ctn7020014
APA StyleEicher, E., Räz, S., Stucki, P., Röthlin, C., Stattmann, M., Grossenbacher, B., Neumann, E., Pohl, H., Ilg, Y., Maatz, A., & Wegener, S. (2023). ComPAIN—Communication of Pain in Patients with Headache. Clinical and Translational Neuroscience, 7(2), 14. https://doi.org/10.3390/ctn7020014







