Comparing the Long-Term Stability of Titanium Clip Partial Prostheses with Other Titanium Partial and Total Ossicular Reconstruction Prostheses
Abstract
1. Introduction
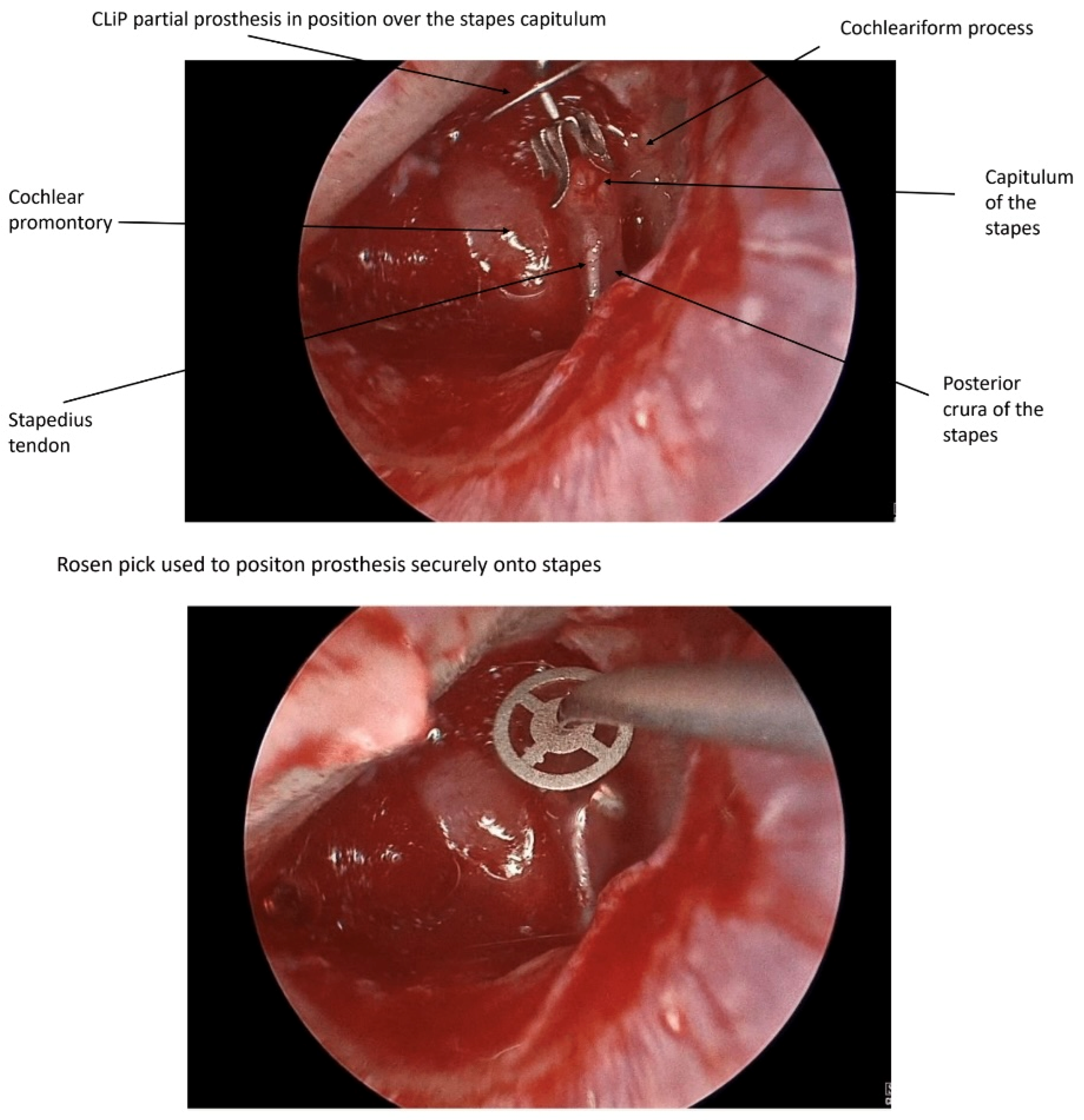
2. Methods
2.1. Study Design
2.2. Statistical Analysis
3. Results
3.1. Demographics
3.2. Preoperative and Surgical Information
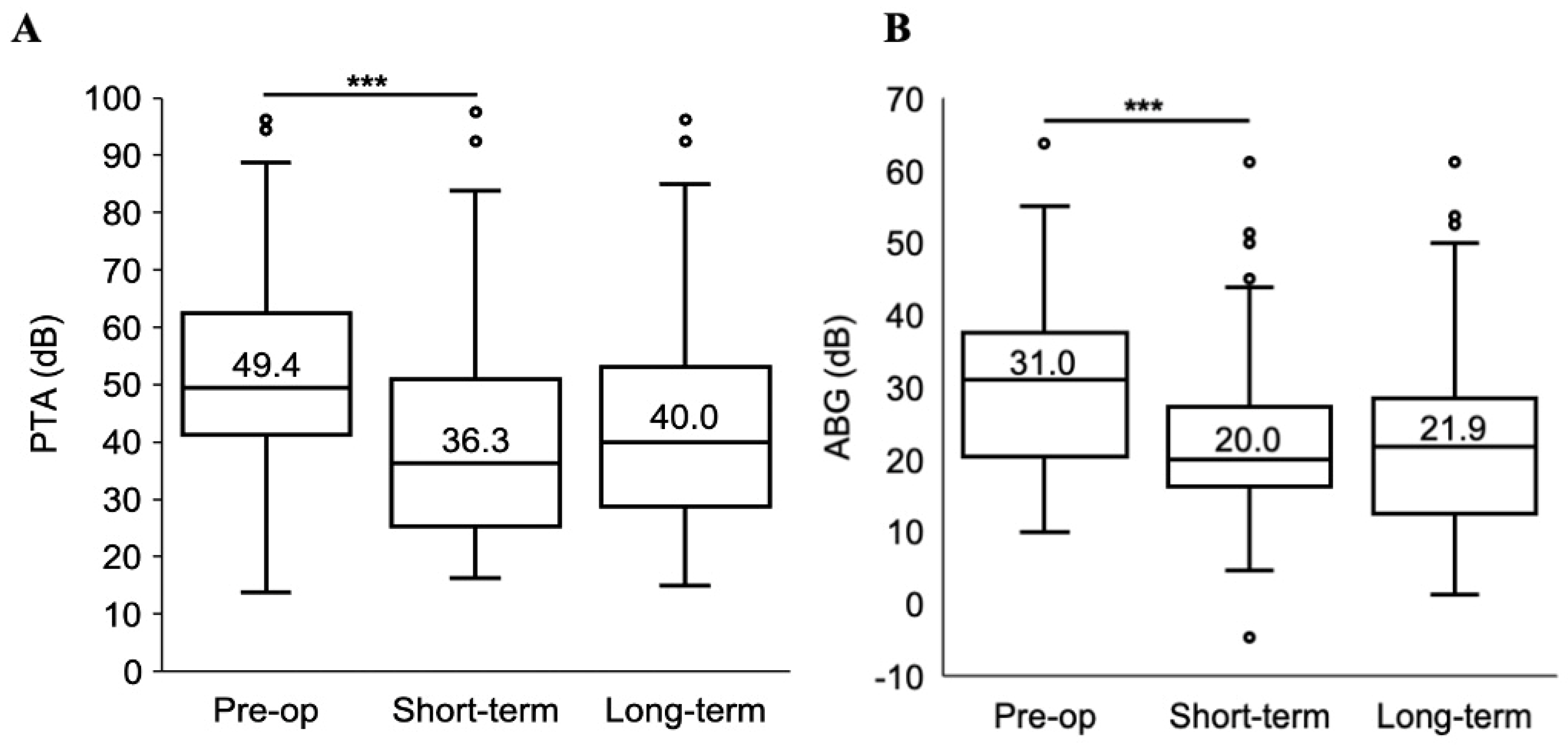
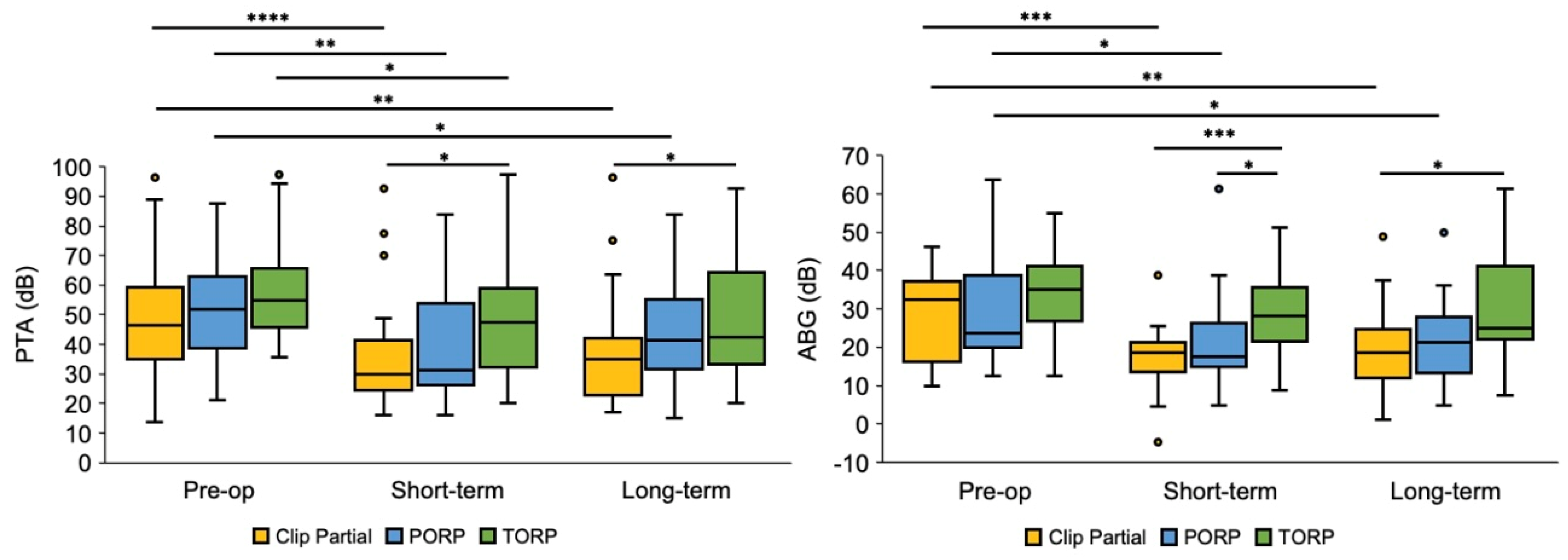
3.3. Short-Term Follow-Up
3.4. Long-Term Follow-Up
3.5. Stability Analysis
3.6. Cholesteatoma Patients
3.7. Revision Cases
3.8. Perioperative Complications
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Blom, E.F.; Gunning, M.N.; Kleinrensink, N.J.; Lokin, A.S.H.J.; Bruijnzeel, H.; Smit, A.L.; Grolman, W. Influence of Ossicular Chain Damage on Hearing After Chronic Otitis Media and Cholesteatoma Surgery: A Systematic Review and Meta-analysis. JAMA Otolaryngol. Head Neck Surg. 2015, 141, 974–982. [Google Scholar] [CrossRef] [PubMed]
- Kortebein, S.; Russomando, A.C.; Greda, D.; Cooper, M.; Ledbetter, L.; Kaylie, D. Ossicular Chain Reconstruction with Titanium Prostheses: A Systematic Review and Meta-Analysis. Otol. Neurotol. 2023, 44, 107–114. [Google Scholar] [CrossRef] [PubMed]
- Shah, K.D.; Bradoo, R.A.; Joshi, A.A.; Sapkale, D.D. The efficiency of titanium middle ear prosthesis in ossicular chain reconstruction: Our experience. Indian J. Otolaryngol. Head Neck Surg. 2013, 65, 298–301. [Google Scholar] [CrossRef] [PubMed]
- Govil, N.; Kaffenberger, T.M.; Shaffer, A.D.; Chi, D.H. Factors influencing hearing outcomes in pediatric patients undergoing ossicular chain reconstruction. Int. J. Pediatr. Otorhinolaryngol. 2017, 99, 60–65. [Google Scholar] [CrossRef] [PubMed]
- Yawn, R.J.; Hunter, J.B.; O’connell, B.P.; Wanna, G.B.; Killeen, D.E.; Wick, C.C.; Isaacson, B.; Rivas, A. Audiometric Outcomes Following Endoscopic Ossicular Chain Reconstruction. Otol. Neurotol. 2017, 38, 1296–1300. [Google Scholar] [CrossRef] [PubMed]
- Erden, B.; Doblan, A. Evaluation of Outcomes Related to Hearing and Tinnitus After Ossicular Chain Reconstruction. J. Craniofacial Surg. 2020, 31, 2250–2255. [Google Scholar] [CrossRef] [PubMed]
- Hüttenbrink, K.-B.; Zahnert, T.; Wüstenberg, E.G.; Hofmann, G. Titanium Clip Prosthesis. Otol. Neurotol. 2004, 25, 436–442. [Google Scholar] [CrossRef] [PubMed]
- Kahue, C.N.; O’connnell, B.P.; Dedmon, M.M.; Haynes, D.S.; Rivas, A. Short and Long-Term Outcomes of Titanium Clip Ossiculoplasty. Otol. Neurotol. 2018, 39, e453–e460. [Google Scholar] [CrossRef] [PubMed]
- Stuermer, K.J.; Hüttenbrink, K.-B.; Luers, J.C. The Titanium Angular Clip Prosthesis for Ossicular Chain Reconstruction: Long-Term Results. Otol. Neurotol. 2020, 41, 806–809. [Google Scholar] [CrossRef] [PubMed]
- Gostian, A.-O.; Kouame, J.-M.; Bremke, M.; Ortmann, M.; Hüttenbrink, K.B.; Beutner, D. Long term results of the titanium clip prosthesis. Eur. Arch. Otorhinolaryngol. 2016, 273, 4257–4266. [Google Scholar] [CrossRef] [PubMed]
- Omar, M.; McCoy, J.L.; Kitsko, D.J.; Chi, D.H. PORP vs. TORP in children: A systematic review and meta-analysis. Am. J. Otolaryngol. 2023, 44, 103658. [Google Scholar] [CrossRef] [PubMed]
- O’connell, B.P.; Rizk, H.G.; Hutchinson, T.; Nguyen, S.A.; Lambert, P.R. Long-term Outcomes of Titanium Ossiculoplasty in Chronic Otitis Media. Otolaryngol. Neck Surg. 2016, 154, 1084–1092. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.; He, Y.; Ni, Y.; Wang, Y.; Lu, N.; Li, H. PORP vs. TORP: A meta-analysis. Eur. Arch. Oto-Rhino-Laryngology 2013, 270, 3005–3017. [Google Scholar] [CrossRef] [PubMed]
- Yung, M. Long-term results of ossiculoplasty: Reasons for surgical failure. Otol. Neurotol. 2006, 27, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Adriaansens, C.; Bekkers, S.; Aarts, M.C.J. Determinants influencing cholesteatoma recurrence in daily practice: A retrospective analysis. J. Laryngol. Otol. 2022, 136, 119–124. [Google Scholar] [CrossRef] [PubMed]
- Weiss, N.M.; Do, H.V.; Großmann, W.; Oberhoffner, T.; Schraven, S.P.; Mlynski, R.A. Comparison of total and partial ossicular replacement prostheses in patients with an intact stapes suprastructure. Laryngoscope 2020, 130, 768–775. [Google Scholar] [CrossRef] [PubMed]
- Baker, A.B.; O’connell, B.P.; Nguyen, S.A.; Lambert, P.R. Ossiculoplasty With Titanium Prostheses in Patients with Intact Stapes: Comparison of TORP Versus PORP. Otol. Neurotol. 2015, 36, 1676–1682. [Google Scholar] [CrossRef] [PubMed]
- Neo, W.L.; Yuen, H.W. TORP ossiculoplasty in the presence of an intact stapes superstructure. Am. J. Otolaryngol. 2021, 42, 102831. [Google Scholar] [CrossRef] [PubMed]
- Faramarzi, M.; Roosta, S.; Faramarzi, A.; Kherad, M. Comparison of partial vs. total ossicular chain reconstruction using titanium prosthesis: A retrospective cohort study. Eur. Arch. Oto-Rhino-Laryngology 2023, 280, 3567–3575. [Google Scholar] [CrossRef] [PubMed]
| Age, Median (Range), Years | 47 (19–74) |
|---|---|
| Sex, n (%) | |
| Male | 41, 45% |
| Female | 51, 55% |
| Ethnicity, n (%) | |
| Caucasian | 29, 32% |
| African American | 5, 5% |
| Hispanic | 4, 4% |
| Asian | 6, 7% |
| Other | 47, 51% |
| Missing | 1, 1% |
| Ear, n (%) | |
| Left | 40, 43% |
| Right | 52, 57% |
| Preoperative diagnosis, n (%) | |
| Cholesteatoma | 54, 64% |
| Tympanic membrane perforation | 46, 54% |
| Malpositioned or extruded prosthesis | 6, 7% |
| Otitis media | 16, 19% |
| Tympanosclerosis | 3, 4% |
| Encephalocele | 1, 1% |
| Congenital aural atresia | 1, 1% |
| Preoperative ossicle status per imaging, n (%) | |
| Malleus erosion | 26, 29% |
| Incus erosion | 52, 57% |
| Stapes erosion | 16, 18% |
| Surgery, n (%) | |
|---|---|
| Primary surgery | 67, 73% |
| Planned second-look | 5, 5% |
| Revision (prior surgery at same institution) | 5, 5% |
| Revision (prior surgery outside of institution) | 15, 16% |
| CWU | 59, 64% |
| CWD | 3, 3% |
| Tympanoplasty | 26, 28% |
| Prosthesis type, n (%) | |
| PORP | 29, 32% |
| TORP | 26, 28% |
| Clip partial | 37, 40% |
| Prosthesis length, mode (range), mm | 2 (0.75–5.5) |
| Clip Partial (n = 37) | PORP (n = 31) | TORP (n = 24) | ||||
|---|---|---|---|---|---|---|
| PTA ≤ 25 dB | ABG ≤ 20 dB | PTA ≤ 25 dB | ABG ≤ 20 dB | PTA ≤ 25 dB | ABG ≤ 20 dB | |
| Short-term follow-up | 12 (32.4%) | 23 (62.2%) | 6 (19.4%) | 15 (48.4%) | 3 (12.5%) | 5 (20.8%) |
| Long-term follow-up | 9 (24.3%) | 20 (54.1%) | 5 (16.1%) | 14 (45.2%) | 3 (12.5%) | 4 (16.7%) |
| Clip Partial (n = 37) | PORP (n = 31) | TORP (n = 24) | Kruskal-Wallis p-Value | |||||
|---|---|---|---|---|---|---|---|---|
| PTA (dB) | ABG (dB) | PTA (dB) | ABG (dB) | PTA (dB) | ABG | ΔPTA | ΔABG | |
| Preop | 46.3 | 32.5 | 50.0 | 23.8 | 55.0 | 35.7 | 0.09 | 0.16 |
| (13.8–96.3) | (10.0–46.3) | (21.3–87.5) | (12.5–63.8) | (35.6–97.5) | (12.5–55.0) | |||
| Short-term follow-up | 30.0 | 18.8 | 33.8 | 18.8 | 47.5 | 27.5 | 0.01 * | <0.01 ** |
| (16.3–92.5) | (−4.6–38.8) | (16.3–83.8) | (5.0–61.3) | (20.0–97.5) | (8.8–51.3) | |||
| Long-term follow-up | 35.0 | 18.8 | 41.3 | 21.3 | 42.5 | 23.8 | 0.06 | 0.03 *** |
| (17.0–96.3) | (1.3–48.8) | (15.0–83.8) | (5.0–50.0) | (20.0–92.5) | (7.5–61.3) | |||
| Stability (Δ LT-ST) | +2.50 | +1.25 | 1.88 | 0 | 0 | −1.25 | 0.77 | 0.70 |
| (−16.3–16.3) | (−11.7–15.0) | (−20.0–36.3) | (−25.0–40.0) | (−47.5, 17.5) | (−26.9, 23.8) | |||
| p-value | 0.57 | 0.87 | 0.24 | 0.67 | 1.00 | 0.70 | - | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leahy, J.; Yang, A.; Wong, K.; Perez, E.R.; Wanna, G.B.; Cosetti, M.K. Comparing the Long-Term Stability of Titanium Clip Partial Prostheses with Other Titanium Partial and Total Ossicular Reconstruction Prostheses. J. Otorhinolaryngol. Hear. Balance Med. 2025, 6, 7. https://doi.org/10.3390/ohbm6010007
Leahy J, Yang A, Wong K, Perez ER, Wanna GB, Cosetti MK. Comparing the Long-Term Stability of Titanium Clip Partial Prostheses with Other Titanium Partial and Total Ossicular Reconstruction Prostheses. Journal of Otorhinolaryngology, Hearing and Balance Medicine. 2025; 6(1):7. https://doi.org/10.3390/ohbm6010007
Chicago/Turabian StyleLeahy, Jasmine, Alicia Yang, Kevin Wong, Enrique R. Perez, George B. Wanna, and Maura K. Cosetti. 2025. "Comparing the Long-Term Stability of Titanium Clip Partial Prostheses with Other Titanium Partial and Total Ossicular Reconstruction Prostheses" Journal of Otorhinolaryngology, Hearing and Balance Medicine 6, no. 1: 7. https://doi.org/10.3390/ohbm6010007
APA StyleLeahy, J., Yang, A., Wong, K., Perez, E. R., Wanna, G. B., & Cosetti, M. K. (2025). Comparing the Long-Term Stability of Titanium Clip Partial Prostheses with Other Titanium Partial and Total Ossicular Reconstruction Prostheses. Journal of Otorhinolaryngology, Hearing and Balance Medicine, 6(1), 7. https://doi.org/10.3390/ohbm6010007






