1. Introduction
In the field of orthotics, mass customization using additive manufacturing (or 3D printing—3DP) is required since upper limb orthoses or insoles must be properly tailored to each patient’s unique anatomical features. This personalization is mandatory to achieve successful healing, provide optimal support and control to the affected body part, ensure comfort, promote adherence to usage, and relieve pain [
1]. When it comes to insoles, the advantages extend beyond the intrinsic and customized design provided by 3DP. Customization also makes it feasible to manufacture insoles with varying stiffness levels that match different peak plantar pressures zones through adjustments of infill density and pattern [
2]. In the case of insoles, thermoplastic polyurethane (TPU) is the preferred filament material, while for wrist-hand orthoses, polylactic acid (PLA), polyamide, and acrylonitrile butadiene styrene (ABS) are commonly used [
3]. An observed negative reaction associated with these rigid materials is the development of pressure sores or skin redness [
4]. However, effective clinical outcomes and patient preference for an aesthetically pleasing design and lightweight construction achieved through the incorporation of open pockets of varied shapes and dimensions have been reported [
5,
6]. These features also contribute to enhanced hygiene and ventilation and facilitate the observation of the skin’s status [
4,
5,
6]. For ensuring customization, the 3D-printed orthoses’ design process starts by reverse engineering patient upper limb anatomy, usually using 3D scanning [
7,
8]. Scan data processing is followed by the orthosis design, and different approaches to automate this process have been proposed [
9,
10]. More recently, another concept has emerged involving the thermoforming of a flat shape of a PLA orthosis with dimensions tailored to the patient’s forearm [
9,
11]. PLA thermoforming ability at temperatures around 50–60 °C allows a safe molding to the patient hand. This approach seeks to minimize printing time and overall costs, while eliminating the need for the 3D scanning of the upper limb and the associated data processing. A similar perspective, centered on the concept of flatly 3D printing orthoses, was investigated by Badini et al. using PCL (poly-ε-caprolactone), which conforms to the patient’s hand and returns to its initial shape after removal [
12]. Furthermore, for improving comfort, the idea of adding a thin layer of silicone [
9] or other soft material (such as TPU) has emerged.
In this context of needing improvements in the orthotics field, the purpose of the research was to investigate a novel material, varioShore TPU (ColorFabb, Belfeld, The Netherlands), for its application in the production of customized 3D-printed wrist-hand orthoses. The advantage offered by varioShore TPU in this application lies in its capability to be customized for variable stiffness through process settings [
13]. Specifically intended for conservative management treatment in conditions such as carpal tunnel syndrome or arthritis, the goal was to enhance comfort on contact with the patient’s skin while meeting criteria such as effective immobilization, reduced printing time, and cost efficiency. The hypothesis was that varioShore TPU allows for improved comfort, tailored to different zones of the hand and forearm. The conditions and necessary process parameter settings for TPU and hybrid TPU-PLA orthoses manufacturing using the material extrusion process (MEX) were also addressed in this research. Furthermore, the flat design of the orthoses was customized using an app specifically developed for this purpose.
Three-dimensional printing with both soft and rigid polymers is currently employed in various applications such as soft grippers to take advantage of the flexible configurations facilitated by elastomers in association with the rigid conductive polymers [
14], or origami structures where PLA panels are enveloped by a TPU skin to create a flat combination of a stiff section and a flexible hinge [
15]. However, it is important to note that in many of these studies, the manufacturing process is complex and not conducted on low-cost 3D printers with a single extrusion nozzle. This criterion was a key consideration in our research to ensure widespread accessibility to the application in the orthotics field. The combination of TPU and rigid polymers is documented for the manufacturing of 3D-printed wrist-hand orthoses in a two-step process, aimed at enhancing patient skin comfort [
8]. In the literature, another proposed approach was to produce a bi-material hand splint by overmolding a soft material (silicone) onto 3D-printed PLA layers in a flat configuration, connected through mechanical bonding [
9]. However, this requires the use of a mold and injecting the soft material into channels within the rigid component. A recent study investigates the adhesion between TPU and PLA using chemical bonding [
16], which is not suitable when the product in used in contact with human skin. Also, Sorimpuk et al. studied the interfacial surface bonding of TPU/PLA when thermoformed at temperatures between 60 °C and 90 °C [
17]. However, no data on the type of TPU were provided, and only the specimens’ behavior was investigated.
Advancements in materials science, particularly in thermoplastic polyurethane filament like Colorfabb’s varioShore TPU (92A shore hardness before 3D printing) that integrates foaming agents, can simplify the production of orthoses. With varioShore TPU, it is possible to achieve varying hardness levels using a single 3D printer and one extrusion nozzle by adjusting the printing temperature [
13]—to better understand this, scanning electron microscopy (SEM) investigations were conducted on varioShore specimens which were 3D-printed at various temperatures. Furthermore, these orthoses can take advantage of variable infill density in different regions because they are 3D-printed in a flat configuration, which is not possible when produced directly in their functional shape based on 3D scanning data. The literature review revealed no similar research. In this context, various designs of 3D-printed wrist-hand orthoses were designed, produced, and tested via a trial-and-error approach, assessing them against multiple criteria. The orthoses underwent evaluation by a healthy user, assessing the maximum flexion angle (as indicative of the immobilization rigidity), and considering criteria associated with comfort and perceived wrist stability, as well as printing time and cost.
This research presents several novelties. Firstly, it explores the use of TPU for producing flat orthoses directly fitted onto the patient’s hand—an idea not documented in the existing literature. Another innovative approach involves combining PLA layers with TPU layers in a flat orthosis configuration, followed by its thermoforming. Additionally, the development of a specialized app designed to customize the flat design of orthoses based on patient hand measurements is another contribution to the field.
2. Materials and Methods
2.1. Three-Dimensional Printing of Samples
The 3DP process took place after the careful calibration of the Prusa MK3s+ 3D printer equipped with an E3D Revo extruder. This calibration aimed to achieve better control over the quality and accuracy of the 3D printing process by establishing a correlation between printing temperature and the flow rate, particularly for larger parts [
13].
The method of manufacturing is based on setting different extrusion temperatures for varioShore layers (a modification in G-code is made, namely, M104 S220; M221 S48), as well as on various infill densities. Prior research [
13] addressed the influence of several process parameters such as printing temperature, infill density, and infill pattern on the hardness of TPU 3D-printed parts. The hardness of the orthotic device plays a significant role in evaluating the general comfort at the specific point where it interfaces with the user’s body.
The main common printing parameters for the orthoses produced in this research are presented in
Table 1 for green varioShore TPU and purple PLA. The difference in nuances of green in orthoses’ lateral views (
Table 2) is due to the layers’ different printing temperature inducing different foaming levels/stiffness. Details on process parameters for each analyzed orthosis, including thickness and other design information, are presented below, as well as in the
Supplementary Material. The volar orthoses were tailored to the anatomical morphology of a single healthy user using a web app [
18] (described in
Section 2.2) dedicated to this purpose; samples 4–5 are modified versions with pockets for Velcro strips fixation.
The full varioShore TPU wrist-hand orthoses consisted of layers 3D-printed at 190 °C (unfoamed) with a 100% infill density, as well as layers 3D-printed at 220 °C (fully foamed), with different combinations of infill densities while aiming to keep stiffer the zones around the wrist. A single extruder 3D printer was used in this research, with sample 5 in
Table 3 illustrating the integration of 100% infill density PLA inserts into the varioShore orthosis. The intention behind this approach was to improve wrist flexion rigidity while maintaining the comfort provided by the soft TPU against the skin.
Table 2 presents the specific parameters used in producing the different samples from varioShore, as well as images of their design or images from the manufacturing stage, while
Table 3 provides the equivalent information for hybrid TPU-PLA orthoses. After the layers of PLA were extruded at 210 °C, the 3D printer executed a change filament command switching to TPU extruded at 220 °C with the purpose of obtaining better TPU-PLA layer adhesion.
The hybrid TPU-PLA orthoses were made starting from a standard PLA profile, with the values mentioned in
Table 1. This ensured good inter-bonding between the two materials. Several commands were added to the g-code (see
Supplementary Material): material change, temperature change, and flow change. The advantage of using a PLA profile is that the temperature shift is gradual, as it goes from 210 °C to 220 °C. And another important aspect in the adhesion of the two materials was represented by the 100% TPU density layer at a height of 2 mm, which served as foundation for the lower density layers. Modifier bodies were used to create all the other features such as printing speed, the number of perimeters, density, and pattern.
The
Supplementary Material details the design of each sample to better show how the samples are different by presenting images from Prusa Slicer, and also includes the g-codes for manufacturing the samples.
2.2. SEM Investigations of varioShore Sample Foaming Behavior at Different Printing Temperature
Increasing the softness of the orthoses’ interior surface to improve comfort was based on the foaming characteristics of the varioShore TPU material. Research data on foaming behavior and its dependence on process parameter settings is scarce [
13], and to the best of the authors’ knowledge, the foaming mechanism has not been studied to understand the changes at the microstructure level. To bridge this gap and gather data on the influence of printing temperature on the hardness of the samples, microscopy examinations were performed utilizing the Phenom ProX (Phenom-World B.V., Eindhoven, The Netherlands) scanning electron microscope (SEM). Given the nonconductive nature of these materials, a charge reduction sample holder was used during these investigations.
Cuboid samples, 3D-printed at 190 °C, 220 °C, and 240 °C with 100% infill density, and their cross-sections were analyzed.
2.3. Web App for Designing Customized Wrist-Hand Orthosis
An improved version of the web app described in [
9] was developed to assist the hand therapists in generating the 3D model, and the STL file, of a flat-shaped orthosis based on the patient’s forearm and hand [
18]. Subsequently, thermoforming the flat 3D-printed orthosis allows the practitioner to obtain a good fit onto the patient’s upper limb. Moreover, by 2D printing and applying the paper version of the orthosis (a PDF file generated by the app) as a wrap before the 3D printing process, the need for new prints with adjustments can be further reduced. The application mirrors the approach followed by practitioners when using thermoplastic casts [
19].
Figure 1 shows images from the application and the explanations for some of the parameters used. Here, it should be noted that the external shape of the orthosis in
Figure 1a can be different for different set values of the parameters.
The web-based application was developed to allow its capabilities to be expanded to encompass a wider range of orthotic types and patterns. The current online version (V2) includes two types of orthoses and two ventilation open pocket shapes (elliptical and hexagonal).
The technologies employed were as follows:
FreeCAD (Version 0.21.2) as a computer aided-design package for the 3D solid modeling of the flat orthosis. Two files were generated, according to each type of orthosis. FreeCAD is a platform-independent software package that runs either on Windows, mac or *nix-like operating systems and it seamlessly integrates with Python programming language.
Pyhton programming language was used to develop the backend of the application. FreeCAD can be loaded and used without a graphical user interface with Python which makes the use of the designing software package low on resources consumed and faster in performing different types of operations such as extrusions, rectangular and circular patterns, and Boolean operations.
ReactJs—Javascript library was used to create the frontend of the application. The primary rationale behind selecting this library was its efficiency, offering an open-source solution for constructing rapid and scalable web application frontends.
Nginx with gunicorn. Nginx is a lightweight web server which handles static pages and SSL implementations easily, and gunicorn is the WSGI server which can run a Python application.
Figure 2 shows the dataflow in this application.
As noted earlier, samples 4–5 were created using the V1 web-app, but modifications were made manually to the solid model by adding pockets to accommodate the Velcro strips. This aspect will be solved in the V3 version of the app in order to make it automatic. Meanwhile, the remaining orthoses, varying in thickness, were designed using the app (V1), featuring elliptical holes used for ventilation, reduced weight, as well as for inserting the three strips which secure the orthosis on the hand.
The workflow using FoRTE app [
18] is conceptually based on customizing the design of the orthosis by measuring several key parameters of the hand and forearm, additionally defining the geometry of the pockets, their dimensions and numbers—as parameters input by the hand therapist into the application. The patient’s hand contour is drawn on a paper based on the shape of a volar splint (illustrated with the dark blue contour in
Figure 1a). This approach aligns with the one currently used for manufacturing with thermoplastic casting [
19]. Subsequently, the dimensions are measured on the drawn contour with a ruler, and input in the corresponding fields in the web app.
Figure 3 is a screenshot from the application with the specific parameters related to the geometry of the pockets and the distances between them for the orthosis with elliptical holes. This pattern is repeated horizontally and vertically based on the dimensions input by the user.
For the flat orthosis with an elliptical pocket design, the dimensions of the pockets are illustrated in
Figure 3. The major axis value is 18 mm (parameter: major_axis), the minor axis value is 10 mm (parameter: minor_axis), and the distance between ellipses on both the vertical and horizontal dimensions is 4 mm (parameter: wall thickness). The elliptical shape for the thumb is defined by the following parameters: t_major_axis (50 mm), t_minor_axis (30 mm), and t_angle (180°), while the position of its center is described using different formulas embedding hand therapist knowledge, such as the value of i parameter (
Figure 1a) which is recommended to be over 20 mm so that the orthosis molds around the forearm. By changing the parameters and the formulas, including the shape of the external orthosis contour or the position of the pockets (for instance, the elliptical pockets to be distributed at a certain angle and not vertically and horizontally), different designs can be obtained. However, users cannot make these changes directly; rather, the app administrator must modify the corresponding sketches in FreeCAD.
2.4. Assessment of User’s Comfort and Satisfaction with the Wrist-Hand Orthoses
Patient satisfaction with the use of an orthotic device is subjective as it depends on different factors such as the patient’s expectations of the device, past experiences in similar circumstances, the device’s attractive design, the ease of use for daily tasks, etc.
Orthosis material biocompatibility is an important aspect to consider. In this research, natural varioShore TPU was used. However, the findings are also applicable to the new varioShore TPU filaments dedicated to prosthetics and orthotics applications [
20].
Literature reviews of patient satisfaction with orthoses [
21,
22] have shown several assessment instruments available, mainly based on questionnaires with varying scales, the results being interpreted using a variety of statistical means. Besides the functional features related mainly to the immobilization strength, it is also important to evaluate the wear satisfaction, as this is correlated with the patient’s willingness to adhere to the prescribed usage of the device for the recommended duration. This has a significant impact on the overall effectiveness of the treatment.
Different criteria are used to compare 3D-printed orthoses/splints with traditional ones such as production time and users’ satisfaction [
23], clinical effectiveness [
5], or functionality and comfort [
24]. Reduced production time is reported in [
23], according to an analysis performed on a series of ten clinical cases showing a mean of 112 min for 3D-printed orthoses in comparison to 239 min for traditional casting, while the satisfaction scores (based on QUEST 2.0 assessment) were similar for both production methods. In our research, the production time is longer as 3D printing TPU is a slower process than for PLA, for instance. Damiao et al. investigated 3D-printed and traditional orthoses using Jebsen–Taylor Hand Function Test (JHFT) and Patient-Rated Wrist Evaluation (PWRE) [
24], and concluding that users preferred the 3D-printed versions, but due to a small sample size, the results were not statistically analyzed.
Thus, acknowledging the material’s flexibility alongside the imperative for stability (measured quantitatively using the maximum flexion angle, see
Section 2.4), our study has investigated two subjective aspects: perceived stability (rated from 1—very unstable to 5—very stable) and comfort (rated from 1—very uncomfortable to 5—very comfortable).
2.5. Measuring ROM (Range of Movement) in Flexion
The functional aspect analyzed in this study was measuring the value of the maximum flexion angles while wearing the orthoses, as in Aranceta-Garza et al. [
22]. Several tools can be used for this purpose, including a manual goniometer or smartphones [
25]. The approach adopted involved capturing photos of the hand and subsequently analyzing those using ImageJ (1.46r, National Institutes of Health, Bethesda, MD, USA) measuring tools, similar to the technique employed by Ge et al. [
26]. ROM (range of motion) in flexion was assessed from a lateral view by measuring across the exterior surface of the palm from the second metacarpal and a horizontal line. In the literature, different landmarks were used. In [
27], for instance, the patient’s hand had no orthosis placed on it and more anatomical landmarks were available. In this research, the idea was to assess the orthoses’ stiffness by measuring a similar angle for all (
Figure 4). Attention was paid to maintaining the same position of the smartphone camera, hand position, and orientation on the table.
3. Results and Discussion
3.1. Colorfabb varioShore Sample SEM Results
The analysis of SEM images showed that at the printing temperatures of 220 °C and 240 °C, the foaming agent is activated and the particles within the component undergo expansion (
Figure 5). This phenomenon is not visible at 190 °C (
Figure 5a) wherein the triangular or diamond voids intrinsic to filament deposition are present. These voids can also be seen in the sample which was 3D-printed at 220 °C (
Figure 5b), but not in the sample 3D-printed at 240 °C (
Figure 5c).
In the case of the sample which was 3D-printed at 220 °C, the formerly well-defined pores lose their clarity and demarcation, suggesting that the expansion of the foaming agent results in the printing material infiltrating and filling these cavities(see the highlighted red zones in
Figure 5).
Concerning the pore size influenced by the foaming agent, in the sample 3D-printed at 190 °C, the expansion was minimal or inexistent, with only negligible changes and small void dimensions. The pores in the 240 °C sample were smaller compared to those in the 220 °C sample, and their morphology exhibited subtle variations. Specifically, while in the sample 3D-printed at 220 °C, pores assumed a spherical shape, those in the 240 °C sample exhibited an oval or flattened configuration. Consequently, the measurement of these pores becomes imperative for a comprehensive understanding of their characteristics, and constitutes the topic of a further research study.
At 220 °C, the extent of foaming seems to be optimal with well-defined, spherical, undistorted pores, and for this reason, the varioShore TPU layers in contact with the skin were manufactured at this printing temperature.
3.2. Results on Orthoses’ Flexion Angles and Thermoforming Defects
Figure 6 displays the varioShore wrist-hand volar orthoses in lateral plane and their corresponding maximum flexion angle. Each orthosis was similarly securely attached to the forearm of a healthy user using three Velcro strips corresponding to the palm, wrist, and forearm zones. Attention was paid to ensuring similar tightness by placing marks on the Velcro strips.
For fully TPU wrist-hand orthoses (samples 1–3), as it can be noted in
Figure 6a–c, the stiffness around the wrist was not suitable for the application, while for sample 4 (
Figure 6d), also completely made from varioShore with layers of different printing temperatures, the rigidity was substantially improved, at the cost of a larger weight and bulky aspect.
The flexion angle for samples 1–3 (all having the same design and 3 mm thickness) was not largely different (129–133°) (
Figure 6a–c), despite using different infill densities (100% vs. 80%/40% vs. 60%/30%). It is important to mention that two of the authors measured the angles (inter-observer variability) and the error was ±1.15°. For sample 4, the value of the flexion angle value was around 158° (
Figure 6d).
The design of sample 5 included 2 mm thick PLA all over the surface (between the TPU layers). This resulted in the orthosis being extremely rigid, eliminating the need to check the flexion angle from this standpoint. As its weight was considered too large, sample 6, with larger pockets and inserts of PLA instead of whole surface, was designed (
Figure 6e). Sample 6 exhibited an increased rigidity of the PLA inserts’ regions, better conforming to the shape of the wrist and palm, with the flexion angle measuring around 148°.
At this stage of the study, it became evident that the use of PLA and its thermoforming abilities would more effectively meet the functional demand for rigidity, while maintaining a lightweight structure. Therefore, two more designs were produced (samples 7 and 8), with the exterior layers made of PLA of different thickness (2.2 mm vs. 2.6 mm, see
Supplementary Material) and the interior made of varioShore for a soft contact between the orthoses and the user’s skin. Their stiffness was according to specification as can be seen in
Figure 7 for sample 8—best rated by the user.
It is noteworthy that samples 6 and 7 underwent shrinkage during the thermoforming process. This aspect should be considered when designing the orthosis’ flat model and inputting parameters into the web-based design application.
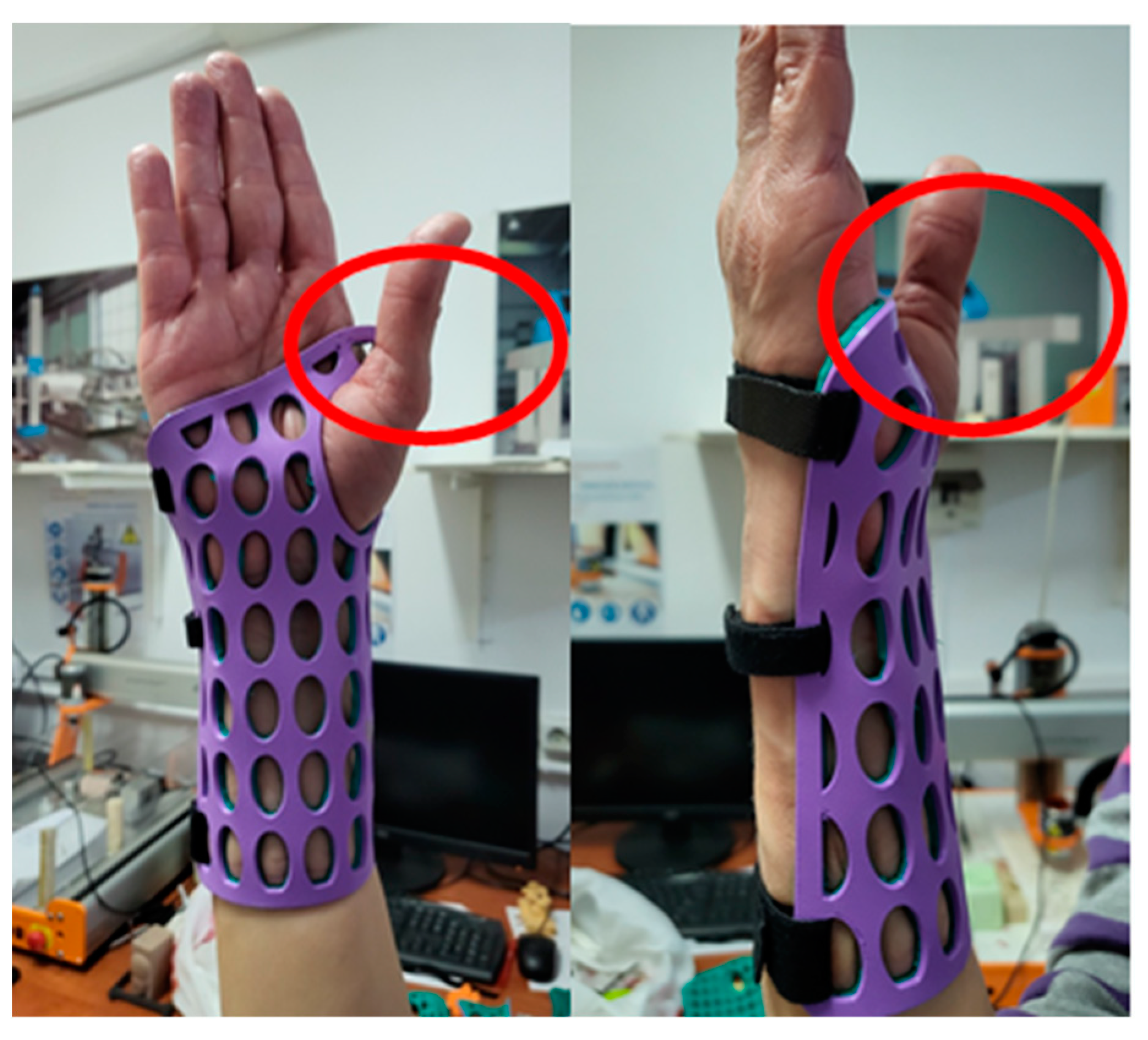
Defects occurred for two of the samples, in both cases caused by thermoforming. In
Figure 8a the detachment of varioShore layers (green) from the PLA layers (sample 6) after several flexion movements is visible. The thermoforming of this sample was performed by placing the TPU-PLA on the printing bed set at 70 °C. When hot water was used for sample 6, thermoforming and conformity were appropriate, but the TPU layers detached from the PLA insert (sample 6 was the only one thermoformed using hot water).
Figure 8b displays a different defect, this time found on the PLA layers, resulting from the thermoforming process intended to shape the palm area and from the reduced thickness of the PLA layers (sample 7).
3.3. User’s Assessment of 3D-Printed Orthoses
Information on comfort assessments, and the perceived immobilization strength, printing time, and cost for each orthosis is presented in
Table 4, alongside a very brief comment from the person testing the orthoses.
Orthoses 1–3 follow a shared design, while sample 4, with its smaller holes and increased thickness, enhanced the rigidity but also the bulkiness. Nonetheless, it did not fit the user’s wrist properly, leading to a sense of wrist looseness within the orthosis walls (scoring only 3 points on the Likert scale for perceived wrist stability criteria). Samples 1–3 folded or wrinkled in the wrist area during flexion, being rated 3 for comfort whereas their lightness and softness was appreciated by the user.
In sample 4, the user particularly favored the softness of the Archimedean Chord pattern on the surface in contact with the hand, density 40%.
Introducing 2 mm thick PLA into a varioShore skin (sample 5) facilitated thermoforming to better conform to the user’s anatomical structure, achieving an improved fit in the palm and wrist areas. Both perceived stability and stiffness notably increased, but the bulkiness and larger weight made the user rate the comfort with 2 points on the Likert scale in comparison with 3 for the first four samples.
Samples 6–8, incorporating larger pockets (lighter design) and layers of PLA, led to improved stiffness and a better fit on the hand, resulting in higher ratings. However, some defects were recorded as shown in
Figure 8, caused by thermoforming. The optimal orthosis, from the user’s perspective, was sample 8.
In terms of cost (
Table 4), the orthoses made fully of varioShore are cost-effective, and the hybrid (varioShore/PLA) orthoses also have a low price, though their printing time was nearly doubled.
4. Conclusions and Further Research
This study explored the integration of varioShore TPU in the manufacturing process of customized flat 3D-printed wrist-hand orthoses. The material used in the MEX process involves an active foaming agent, enabling the adjustment of hardness through alterations in printing temperature settings. SEM investigations conducted in this research highlighted how varying the printing temperatures affected the foaming behavior. This understanding facilitated the optimization of manufacturing parameters and the refinement of orthotic designs so as to create a stiff wrist section and a soft surface in contact with the hand for patient comfort. In other words, this new TPU material allows the production of orthoses with different stiffness levels within one printing process, on an affordable 3D printer using a direct drive extruder and a single nozzle, balancing immobilization and skin comfort. Additionally, a flat 3D-printed orthosis, coupled with a custom web app that uses patient hand measurements to generate a custom design, replaces traditional 3D scanning and modeling techniques, for an easier implementation in 3D printing points-of-care.
This research assessed diverse designs and parameter settings, with the evaluation criteria including printing time, cost, flexibility, comfort, and perceived wrist stability. The orthoses with a slim design solely made from varioShore TPU were cost-effective, but they lacked stiffness in specific areas. Bulkier TPU orthoses improved stiffness at the cost of increased weight and bulkiness. Integrating PLA addressed these issues offering enhanced conformity and stiffness, while maintaining a lighter weight. Thus, this study proved the effectiveness of bi-material orthoses incorporating PLA to enhance wrist stiffness and conformity to hand shape using thermoforming. It also showed the advantages in terms of comfort provided by the studied TPU material.
Further research will address the mechanical strength of these hybrid orthoses when subjected to flexural fatigue corresponding to flexion/extension and ulnar/radial wrist movements. Of particular interest is the analysis of potential failures and delaminations occurring at the interface between the two materials, PLA and TPU, under conditions of fatigue. Additionally, the app will also be updated so as to allow the definition of rectangular pockets to accommodate the Velcro strips, as well as models for left and right forearm.
A limitation of this approach is the effect of water on the bonding of PLA and TPU as presented in the defect analysis. SEM investigations revealed that the pores in varioShore TPU are not connected, indicating that the issue is not attributable to either of the materials but rather to their interface. Consequently, using these hybrid orthoses during activities like showers is not recommended. Therefore, their suggested use is primarily within conservative treatment plans. For example, employing volar splints for carpal tunnel syndrome can effectively support the wrist by maintaining a neutral or slightly extended position, relieving pressure on the median nerve within the carpal tunnel.