Abstract
The miniaturisation of manual systems is reported in this paper. The whole system was based on microfluidic cartridge heated up by a unique contactless system. The presented device utilised fully passive cartridge with required reagents.
1. Introduction
Until today, various point-of-care systems (POCTs) for genetic testing have been introduced to the market, with some of them based on a microfluidic approach. Unfortunately, mainly due to the use of laboratory-grade PCR techniques, these systems do not meet several of the WHO’s ASSURED criteria for a POCT, which has limited their adoption [1,2,3]. A technical issue to be solved with such systems is providing a method for detecting nucleic acids (NAs) in a sample which will allow for the rapid detection of NAs, with the system being mobile, exhibiting low energy consumption and being inexpensive to manufacture while allowing for the storage of the cartridges at a room temperature. In order to allow for the widespread adoption of decentralised genetic-based testing while also reducing technical drawbacks of the current systems, we have developed simplified nucleic acid amplification technology (SNAAT®). It is a microfluidic-based NA isothermal amplification system driven by contactless optical heating and temperature detection coupled with fluorescence detection of amplified genetic material on an electrically passive microfluidic cartridge.
2. Materials and Methods
The system consists of 2 components: the analyser and microfluidic cartridge, which are presented in Figure 1. The basis of the heating system is the electromagnetic radiation to thermal conversion happening directly on defined and insulated areas of the cartridge made by injection moulding from cyclic olefin copolymer (COC). Each card contains both liquid and freeze-dried reagents needed in the sample processing from the extraction of NA to the amplification of genetic material in 6 spatially separated chambers on 3 thermally independent areas that enable multiplexing. Additionally, a plurality of valves and pump mechanism for fluid movement is present on the cartridge. The analyser operating the card is a handheld device that, beyond the display, actuators and other control elements, contains the heating and detection elements that utilise 2 heating units with 24 UV LEDs (400 nm) in total, with a temperature detector for each of the heating zones, as well as 6 fluorescence detectors coupled with optical filters. In that way, we can achieve precise temperature measurement of each of the heated areas, allowing for the best performance of assays present on the cartridge without embedding heaters or sensors within the card while allowing for lower energy consumption. The principle of operation of heating and detecting systems is presented in Figure 2.

Figure 1.
Overview of the analyser and microfluidics cartridge.
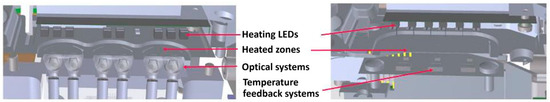
Figure 2.
The principle of operation of the heating and detecting systems.
3. Discussion
Thermally separated extraction chamber to enable the extraction of nucleic acids with an accuracy of ±2 °C. Three thermally separated the heating zones to provide the best thermal conditions for up to six LAMP assays with an accuracy of ±1 °C. The temperature ramps are presented in Figure 3 and the fluorescence readings are presented in Figure 4. These data show capability of the developed system to detect five pathogens within a max. of 30 min. That milestone, in combination with the whole system miniaturization, place it at the top of most efficient methods.
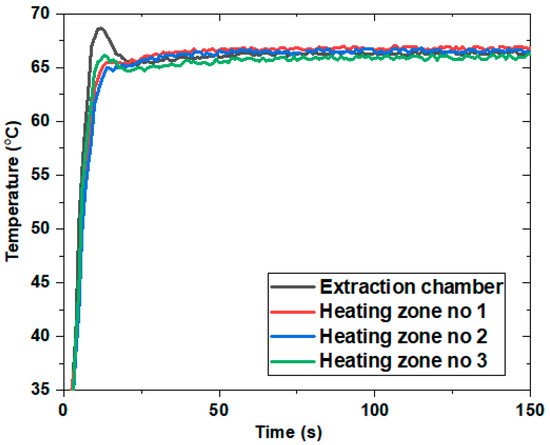
Figure 3.
Temperature ramps of four heating zones.
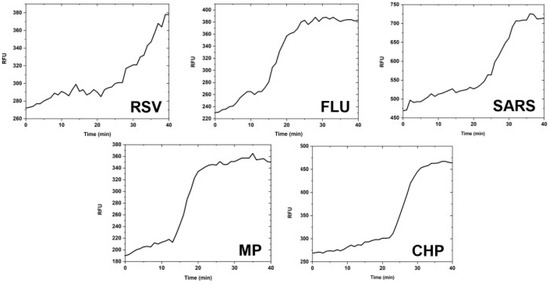
Figure 4.
Fluorescence readings for pathogen presence determination.
Author Contributions
Conceptualization, M.T., H.R. and M.M.-M.; methodology, T.M., H.R., A.D. and M.C.; validation, T.M., H.R. and A.D.; formal analysis, M.M.-M., M.C. and M.T.; writing—review and editing, T.M. and M.T.; project administration, M.T., M.M.-M. and H.R; software, A.D. and P.S. All authors have read and agreed to the published version of the manuscript.
Funding
Part of this research was funded by The National Centre for Research and Development (Poland).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Kiechle, F.L.; Holland, C.A. Point-of-Care Testing and Molecular Diagnostics: Miniaturization Required. Clin. Lab. Med. 2009, 29, 555–560. [Google Scholar] [CrossRef] [PubMed]
- Mori, Y.; Notomi, T. Loop-mediated isothermal amplification (LAMP): A rapid, accurate, and cost-effective diagnostic method for infectious diseases. J. Infect. Chemother. 2009, 15, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Xu, Y.; Fohlerova, Z.; Chang, H.; Iliescu, C.; Neuzil, P. LAMP-on-a-chip: Revising microfluidic platforms for loop-mediated DNA amplification. Trends Anal. Chem. 2019, 113, 44–53. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).