1. Introduction
Advancement in the healthcare technology domain is generally known to improve patient outcomes and enhance healthcare services. The healthcare industry also helps reputable healthcare providers to offer high-quality services with great reliability to the public. Data play a significant role in ensuring that the available healthcare facilities can be improved to meet public needs and expectations. For instance, at the Ulsan University Hospital (UUH) in South Korea, a patient’s medical records are transferred either via paper or phone when a patient is referred to another hospital [
1]. Unfortunately, traditional paper and phone methods may lack reliability. Likewise, for patients who are sent to the emergency department, it can be difficult to know the patient’s medical history, particularly in cases when the elderly cannot recall prior illnesses or the types of medication previously consumed. Therefore, the electronic medical records (EMR) management system plays a vital role in ensuring patients can be diagnosed accurately and treated without further delay. Hence, this paper aims to assess significant challenges and barriers related to EMRs using a mobile application platform.
Although hospitals were first hesitant to adopt the EMR approach in the early 21st century, the use of this approach has grown significantly since the year 2009. Published articles contributed to this trend by reporting the advantages of the EMR approach, such as big data analytics and the ability to incorporate the Internet of Things into a real-time mobile health records management (MHRM) system. As a result, adopting the EMR approach has granted healthcare practitioners easy access to their patients’ data, which further enables them to quickly make decisions regarding their patients’ wellbeing. For instance, a 3D print on a liver may be required for treatment planning if a cancer lesion is found at a complex location. With the help of EMR, clinical practitioners can swiftly review previous notes and any complex clinical issues previously addressed regardless of how dated or where those issues were first addressed. Additionally, instead of relying on a third-party vendor to develop the 3D print, hospitals may choose to establish an in-house 3D printing facility, which will enhance the turnaround time (TAT) and eventually improve patient management. Furthermore, implementation of a mobile approach is timely for those in a medical environment, as healthcare personnel require a system that allows them to be mobile and provide appropriate patient care. With MHRM, healthcare practitioners can access their patients’ data quickly and with ease. Nevertheless, despite the benefits accrued from this platform, the adoption process does not take place without its own set of challenges and obstacles. Therefore, this review paper aims to identify the challenges and obstacles present in the use of the MHRM approach to help the healthcare industry implement the system effectively. Through an examination of the body of literature related to MHRM use, this review investigates the issues affecting the platform’s implementation to answer the following questions: (i) What are the challenges of trusted elements affecting MHRM implementation? (ii) What are the obstacles of trusted elements affecting MHRM implementation?
2. Methods
In this review, the discussion will commence by first presenting the challenges of trusted elements in the MHRM system followed by the obstacles of trusted elements in the MHRM system. Then, the final bulk of this review article will focus on how the issues presented can be addressed to ease the implementation of the platform and data migration. During the research process, several keywords including medical records and challenges of MHRM were used for database search purposes; online databases (PubMed and Scopus) were used to obtain literature related to the topic. The studies reviewed were selected based on four pre-determined criteria: (i) empirical studies on medical records management; (ii) review studies analyzing medical data migration and adoption; (iii) studies on mobile health and health information technology; and (iv) studies investigating medical records’ trustworthiness. A systematic search of research articles was conducted from the period of 2016 to 2020, and 35 articles were deemed relevant to the investigated topics. The review was conducted qualitatively based on issues highlighted in the selected articles. Later, the findings were categorized under two general themes: Challenges of Trusted Elements for MHRM, and Obstacles of Trusted Elements for MHRM.
Table 1 and
Table 2 are discussed in depth in the following sections.
3. Results and Discussion
The greatest challenge in implementing the MHRM system is trust. For the EMR management system to successfully convert into the mobile platform, a practical assessment must be conducted to identify any underlying drawbacks. This assessment is important to identify limitations of the healthcare system and function as a resource to inform the process of formulating mitigation strategies prior to large-scale integration of the system within the existing infrastructure [
30]. According to [
31], early identification of the issues can help reduce the outcomes of misdiagnosis that affect patients’ treatment plans while safeguarding healthcare providers’ reputations. The authors in [
32] reported that a long-term study conducted in multiple countries including Malaysia revealed that 50% of physicians aged 30 to 45 years old display intentions to adopt the EMR system. In this context, well-known vendors offering quality EMR systems include Epic, Cerner, and Allscripts, and the availability of these databases, have been noted to encourage healthcare workers to provide their medical services to patients within a shorter period [
33]. Based on the analysis, common challenges encountered by mobile EMR users are related to data migration, staff resistance, lack of staff training sessions, and data privacy. The findings were in line with [
34], who posited that the underlying issues of EMRs are linked to its application using the mobile platform, which reduces the opportunities to apply appropriate security policies.
3.1. Challenges of Trusted Elements for Mobile Health Records Management
3.1.1. Data Migration
A mobile EMR interface has been proven to provide healthcare workers with numerous benefits that may also result in improved patient experiences when the system is properly optimized. Despite this, one of the biggest challenges for the implementation of this platform is clinical data migration [
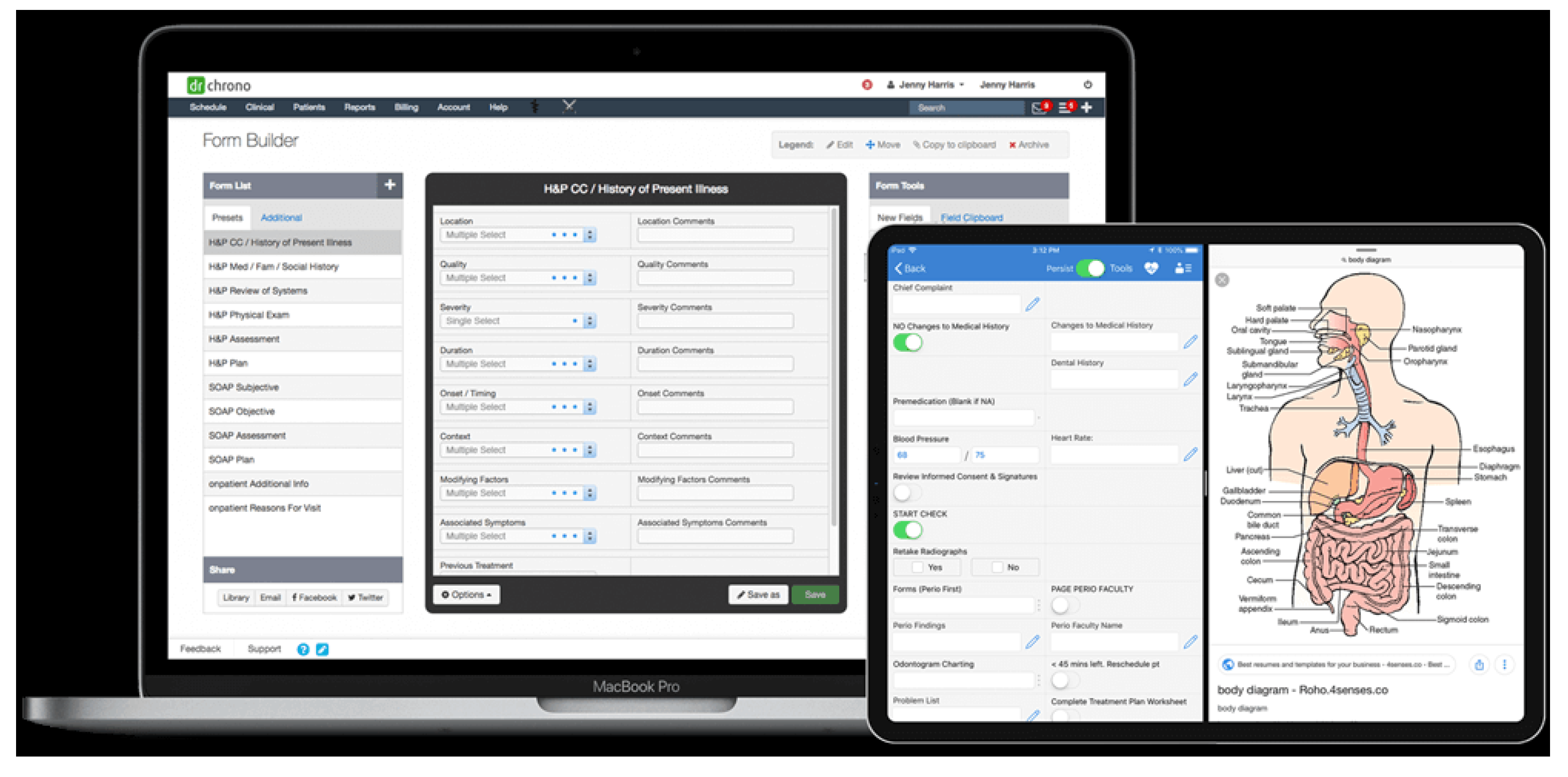
2]. Data migration refers to the process of selecting and transferring data from one storage device to another. Unfortunately, incorrect migration of clinical data can result in a huge impact on a patient’s outcomes. Furthermore, errors that occur during data migration may lead to loss of access to the entire database and consequently will require additional time and cost to correct the migration error. When additional costs are incurred, management may find the process to be less affordable than expected. In addition, during data migration, the presence of large amounts of data within the mobile application might burden the backend servers, which eventually causes data logistics issues. Therefore, to prevent data logistics issues when migrating data from one platform to another (see
Figure 1), the authors in [
3] explained that the migrated data must be digitized to mirror a paper-based document. Unfortunately, digitizing data and creating online forms are time-consuming, and the authors in [
4] reiterated that unintentional errors should be avoided when filling out online forms. Understandably, such carelessness can result in healthcare providers administering the wrong treatment.
3.1.2. Staff Resistance
Enjoying the benefits of the mobile EMR platform requires dedicated contributions from all levels of staff including clinical and non-clinical personnel. According to [
5], healthcare staff are responsible for ensuring that patients’ data are readily available, particularly for those who are awaiting treatment or medical assistance. However, the implementation of this platform does not always occur without resistance from healthcare staff because of the lack of knowledge or technical skills in personnel that allows them to use the mobile EMR system effectively. Notably, although the move to digitize medical records improves the healthcare industry, many healthcare workers are not ready to shift to a paperless format, as they doubt their ability to manage the technicalities of deploying the system on a mobile platform [
6,
7,
8]. Furthermore, it has been noted that healthcare staff’s refusal to use the EMR platform has led to incidences of miscommunication [
9]. Thus, to minimize staff resistance towards the mobile EMR system, there must be effective change enacted from the management level. Additionally, practices supporting the conversion must be applied to begin platform implementation.
3.1.3. Lack of Staff Training Session
From an advancement perspective, healthcare providers are encouraged to adopt the EMR approach instead of the traditional system. However, a lack of relevant technical knowledge supporting the use of EMR is prevalent among healthcare workers and thus restricts them from being able to use the technology. Therefore, offering healthcare staff adequate and effective training sessions can improve their overall technical knowledge base. On the other hand, it must also be noted that Malaysia’s healthcare industry lacks the required capacity to produce suitable training sessions for individuals, including the time, financial costs, and other resources required. As a result, the authors in [
10] believe that the scarcity of available training programs in the country has discouraged the improvement of technical skills among healthcare staff that may further boost the healthcare technology domain. Considering techniques and strategies acquired from healthcare professionals’ experiences may also be helpful to provide practical methods to reduce the system’s underlying issues [
11].
3.1.4. Data Privacy
With the implementation of the EMR mobile platform, it is possible to assume that all clinical and non-clinical personnel will be able to access patient information from anywhere via a mobile device. As such, this situation poses a challenge for data privacy. According to [
12], the documentation process of patient healthcare data exposes sensitive information, and thus any mandatory divulging of patient data for treatment purposes require data confidentiality. In 2016, Tucker and colleagues reported that the application of reduction techniques has helped to reduce risks targeted at patient privacy [
13]. Data privacy is particularly important, as [
14] posited that the unintentional loss of confidentiality associated with patient data can negatively affect the healthcare organization’s reputation in the market. Therefore, to prevent a breach in patient privacy, the authors in [
15] suggested that protecting data with a suitable security protocol is essential.
3.2. Obstacles of Trusted Elements for Mobile Health Records Management
While there are no complete records management systems, there are a few features that can develop the reliability of the management system. Unfortunately, implementing such a system at a national level is not an easy task due to the following identified obstacles.
3.2.1. Cost Structure
The overall cost of implementing an EMR mobile platform is high because the implementation process usually involves several steps including hardware setting, training of staff, software cost and maintenance, and network fees. Furthermore, implementation costs may even be higher in the event of unfavorable situations occurring during the process of optimizing the system, which may subsequently affect the system’s efficacy. In an average system, healthcare providers typically lean towards public company funding to implement the system. Unfortunately, a major challenge faced by the government is that it is typically unable to place a large sum of money into the electronic healthcare record system. For instance, the implementation of the EHR system offers transparency in healthcare charges. This has resultantly led to an increase in the prices of medical treatments. Thus, it can be said that the system is not helpful to average-income earners within the population to access the medical treatments that they need. These terms and conditions will undoubtedly create obstacles within the healthcare system and limit the support of the medical system due to the higher level of medical costs [
16].
3.2.2. Technical Limitations
An optimized mobile EHR platform requires several specialized pieces of equipment to allow the system to function effectively within the healthcare industry. However, the authors in [
17] have demonstrated that a lack of technical integration is present among the major barriers hindering the implementation of the mobile EHR system in healthcare facilities. In addition, mobile EHR requires artificial intelligence (AI) to ensure its cybersecurity, which can be extremely costly. Automation is also not included in mobile EHR, thus leading to data error and a lack of information in healthcare services. Therefore, managing the system by addressing its technical needs is imperative [
18]. For example, mobile EHR depends on technological innovation for its fiber healthcare information recording system. However, the authors in [
19] and [
20] have proven that the lack of technical innovation makes such devices powerless in healthcare facilities, as many healthcare personnel are initially reluctant to use the mobile EHR system.
3.2.3. Poor Data Standardization
Another obstacle identified in this study is poor data standardization in the healthcare industry. Although mobile EHR follows cybersecurity and data protection protocols, the system is not inspected or authenticated by the central authority, thus potentially leading to misdiagnoses. In such circumstances, the authors in [
21] stated that misdiagnosis could be life-threatening to patients. Furthermore, the data standardization process in the mobile EHR platform is complex and critical and requires good technical development knowledge [
36]. However, there is a lack of competent and skillful staff and technological opportunities to carry out such a process. Due to these limitations, healthcare providers have failed to use the adopted technology correctly [
22]. Medical records registered unethically have also been unable to serve as proper medical records for patients due to the risk of causing complications during medical treatments [
23].
3.2.4. Lack of Organizational Infrastructure
The organizational culture in a hospital can also pose an obstacle to EHR implementation. The authors in [
11] highlight that manually recording and maintaining patients’ medical records can lead to poor documentation. Hence, technology is believed to be more effective to standardize information. Unfortunately, the current organizational infrastructure in hospitals is not suitable to implement the mobile recording system, as many individuals in the low-income community are not comfortable recording their health issues on the mobile EHR platform [
5,
24,
25]. As such, healthcare providers, too, are not eager to record patients’ data using mobile devices. To address this issue, the government must take proper initiatives to manage mobile EHR systems in all proposed healthcare services [
26].
3.2.5. Poor Communication Tools
Many clinicians have highlighted that mobile EHR is not an effective communication tool to communicate with patients. Clinicians have found the platform to be challenging when attempting to assist patients as patients’ medical histories are digitally recorded. Apart from the inconvenience caused by mobile EHR, authors in [
23] reported that the mobile EHR platform has limited clinicians’ ability to have physical access to patients. Records displayed on the system have also been found to be incorrect and inadequate at times. As a result, healthcare providers find it difficult to access patients’ actual problems and health issues. Accessing patients’ records is a process that requires highly designed communicative tools for both patients and healthcare providers [
3], which may, unfortunately, pose a challenge for users.
3.2.6. Changes in Workflow
It is commonly highlighted that the mobile EHR platform can make significant workflow changes by reducing medical services’ work requirements as consultation sessions are captured digitally. However, according to [
27], this may also result in the possibility of losing data due to a lack of significant investment in training and operation. For instance, several doctors have reported that using a digital platform may reduce the number of patient visitations [
28]. For this reason, the authors in [
29] offer that this change may be challenging for healthcare providers who must identify patients’ medical issues accurately. Moreover, it has also been argued that medical services become complicated when devices are used to control medical records.
4. Conclusions, Limitations, and Future Implications
The challenges faced in the implementation of the mobile EHR system are: (i) data migration; (ii) staff resistance; (iii) a lack of staff training, and (iv) data privacy. In terms of obstacles, the system is impeded by: (i) cost; (ii) technical limitations; (iii) poor data standardization; (iv) a lack of organizational infrastructure; (v) a lack of communication tools, and (vi) changes in workflow. Unfortunately, the reviewed literature does not provide enough information on the contents that should be present in an ideal mobile medical record system. There is also little mention of how these contents can influence healthcare behavior and perception. Based on this review, it is recommended that greater emphasis be placed on the importance of mobility in medical records management, so that it may be possible to understand how mobile health records can be successfully integrated into healthcare providers’ medical record systems.
Author Contributions
Data curation: F.N.Z. and A.I.; Formal analysis: F.N.Z., N.H., S.F.M.Y. and A.I.; Funding acquisition: F.N.Z., N.H. and S.F.M.Y.; Investigation: F.N.Z. and A.I.; Methodology: F.N.Z. and N.H.; Project administration: F.N.Z.; Resources: F.N.Z. and A.I.; Software: F.N.Z. and A.I.; Supervision: N.H. and S.F.M.Y.; Validation: N.H. and S.F.M.Y.; Visualization: F.N.Z. and A.I.; Writing—original draft: F.N.Z.; Writing—review and editing: F.N.Z. and A.I. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
This paper was presented during the International Academic Symposium of Social Science 2022, organized by Universiti Teknologi MARA (UiTM) Kelantan, Malaysia.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Choi, W.; Park, M.; Hong, E.; Kim, S.; Ahn, R.; Hong, J.; Yeo, S. Early experiences with mobile electronic health records application in a tertiary hospital in Korea. Healthc. Inform. Res. 2015, 21, 292–298. [Google Scholar] [CrossRef] [PubMed]
- Dornan, L.; Pinyopornpanish, K.; Jiraporncharoen, W.; Hashmi, A.; Dejkriengkraikul, N.; Angkurawaranon, C. Utilisation of electronic health records for public health in Asia: A review of success factors and potential challenges. BioMed Res. Int. 2019, 2019, 7341841. [Google Scholar] [CrossRef] [PubMed]
- Lee, E. Taming performance variability of healthcare data service frameworks with proactive and coarse-grained memory cleaning. Int. J. Environ. Res. Public Health 2019, 16, 3096. [Google Scholar] [CrossRef] [PubMed]
- McCracken, S.S.; Edwards, J.S. Implementing a knowledge management system within an NHS hospital: A case study exploring the roll-out of an electronic patient record (EPR). Knowl. Manag. Res. Pract. 2017, 15, 1–11. [Google Scholar] [CrossRef]
- Ganiga, R.; Pai, M.M.M.; Sinha, R.K. Security framework for cloud-based Electronic Health Record (EHR) system. Int. J. Electr. Comput. Eng. 2020, 10, 455–466. [Google Scholar] [CrossRef]
- Xia, Q.; Sifah, E.B.; Smahi, A.; Amofa, S.; Zhang, X. BBDS: Blockchain-based data sharing for electronic medical records in cloud environments. Information 2017, 8, 44. [Google Scholar] [CrossRef]
- Asiri, A.; Obeidat, Q.; Alenezi, M.A. Cloud-based cross-enterprise imaging framework. i-Manag. J. Softw. Eng. 2017, 12, 6. [Google Scholar]
- Drigas, A.; Dede, D.E.; Dedes, S. Mobile and other applications for mental imagery to improve learning disabilities and mental health. Int. J. Comput. Sci. Issues (IJCSI) 2020, 17, 18–23. [Google Scholar]
- Liu, L.; Chen, W.; Nie, M.; Zhang, F.; Wang, Y.; He, A.; Wang, X.; Yan, G. iMAGE cloud: Medical image processing as a service for regional healthcare in a hybrid cloud environment. Environ. Health Prev. Med. 2016, 21, 563–571. [Google Scholar] [CrossRef]
- Evans, R.S. Electronic health records: Then, now, and in the future. Yearb. Med. Inform. 2016, S48–S61. [Google Scholar] [CrossRef]
- Epstein, R.H.; Dexter, F.; Schwenk, E.S. Provider access to legacy electronic anesthesia records following implementation of an electronic health record system. J. Med. Syst. 2019, 43, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Roehrs, A.; da Costa, C.A.; da Rosa Righi, R.; da Silva, V.F.; Goldim, J.R.; Schmidt, D.C. Analysing the performance of a blockchain-based personal health record implementation. J. Biomed. Inform. 2019, 92, 103140. [Google Scholar] [CrossRef] [PubMed]
- Helmers, R.; Doebbeling, B.N.; Kaufman, D.; Grando, A.; Poterack, K.; Furniss, S.; Burton, M.; Miksch, T. Mayo Clinic Registry of Operational Tasks (ROOT): A Paradigm Shift in Electronic Health Record Implementation Evaluation. Mayo Clin. Proc. Innov. Qual. Outcomes 2019, 3, 319–326. [Google Scholar] [CrossRef] [PubMed]
- Choi, E.; Xiao, C.; Stewart, W.F.; Sun, J. Mime: Multilevel medical embedding of electronic health records for predictive healthcare. In Proceedings of the 32nd Conference on Neural Information Processing Systems, Montreal, QC, Canada, 3–8 December 2018; pp. 1–11. [Google Scholar]
- Mukamba, N.; Beres, L.K.; Mwamba, C.; Law, J.W.; Topp, S.M.; Simbeza, S.; Sikombe, K.; Padian, N.; Holmes, C.B.; Geng, E.H.; et al. How might improved estimates of HIV programme outcomes influence practice? A formative study of evidence, dissemination and response. Health Res. Policy Syst. 2020, 18, 121. [Google Scholar] [CrossRef]
- Hussien, H.M.; Yasin, S.M.; Udzir, S.N.I.; Zaidan, A.A.; Zaidan, B.B. A systematic review for enabling of developing a blockchain technology in healthcare application: Taxonomy, substantially analysis, motivations, challenges, recommendations and future direction. J. Med. Syst. 2019, 43, 320. [Google Scholar] [CrossRef] [PubMed]
- French-Baidoo, R.; Asamoah, D.; Opoku Oppong, S. Achieving confidentiality in electronic health records using cloud systems, I.J. Comput. Netw. Inf. Secur. 2018, 1, 18–25. [Google Scholar]
- Simpao, A.F.; Tan, J.M.; Lingappan, A.M.; Gálvez, J.A.; Morgan, S.E.; Krall, M.A. A systematic review of near real-time and point-of-care clinical decision support in anesthesia information management systems. J. Clin. Monit. Comput. 2017, 31, 885–894. [Google Scholar] [CrossRef]
- Xu, J.; Williams-Livingston, A.; Gaglioti, A.; McAllister, C.; Rust, G. A practical risk stratification approach for implementing a primary care chronic disease management program in an underserved community. J. Health Care Poor Underserved 2018, 29, 202–213. [Google Scholar] [CrossRef]
- Kruse, C.S.; Smith, B.; Vanderlinden, H.; Nealand, A. Security techniques for the electronic health records. J. Med. Syst. 2017, 41, 1–9. [Google Scholar] [CrossRef]
- Barak-Corren, Y.; Castro, V.M.; Javitt, S.; Hoffnagle, A.G.; Dai, Y.; Perlis, R.H.; Nock, M.K.; Smoller, J.W.; Reis, B.Y. Predicting suicidal behavior from longitudinal electronic health records. Am. J. Psychiatry 2017, 174, 154–162. [Google Scholar] [CrossRef]
- Cowie, M.R.; Blomster, J.I.; Curtis, L.H.; Duclaux, S.; Ford, I.; Fritz, F.; Goldman, S.; Janmohamed, S.; Kreuzer, J.; Leenay, M.; et al. Electronic health records to facilitate clinical research. Clin. Res. Cardiol. 2017, 106, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Kruse, C.S.; Stein, A.; Thomas, H.; Kaur, H. The use of electronic health records to support population health: A systematic review of the literature. J. Med. Syst. 2018, 42, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Ratwani, R.; Fairbanks, T.; Savage, E.; Adams, K.; Wittie, M.; Boone, E.; Gettinger, A. Mind the gap: A systematic review to identify usability and safety challenges and practices during electronic health record implementation. Appl. Clin. Inform. 2016, 7, 1069. [Google Scholar] [PubMed] [Green Version]
- Larrison, C.R.; Xiang, X.; Gustafson, M.; Lardiere, M.R.; Jordan, N. Implementation of electronic health records among community mental health agencies. J. Behav. Health Serv. Res. 2018, 45, 133–142. [Google Scholar] [CrossRef]
- Hassen, D.B. Mobile-aided diagnosis systems are the future of health care. East. Mediterr. Health J. 2020, 26, 135–1140. [Google Scholar] [CrossRef]
- Mason, P.; Mayer, R.; Chien, W.W.; Monestime, J.P. Overcoming barriers to implementing electronic health records in rural primary care clinics. Qual. Rep. 2017, 22, 2943–2955. [Google Scholar] [CrossRef]
- Parah, S.A.; Sheikh, J.A.; Ahad, F.; Loan, N.A.; Bhat, G.M. Information hiding in medical images: A robust medical image watermarking system for E-healthcare. Multimed. Tools Appl. 2017, 76, 10599–10633. [Google Scholar] [CrossRef]
- López-Martínez, F.; Núñez-Valdez, E.R.; García-Díaz, V.; Bursac, Z. A case study for a big data and machine learning platform to improve medical decision support in population health management. Algorithms 2020, 13, 102. [Google Scholar] [CrossRef]
- Alhajeri, M.; Shah, S.G.S. Limitations in and solutions for improving the functionality of picture archiving and communication system: An exploratory study of PACS professionals’ perspectives. J. Digit. Imaging 2019, 32, 54–67. [Google Scholar] [CrossRef]
- Choi, E.; Xu, Z.; Li, Y.; Dusenberry, M.; Flores, G.; Xue, E.; Dai, A. Learning the graphical structure of electronic health records with graph convolutional transformer. In Proceedings of the AAAI Conference on Artificial Intelligence, New York, NY, USA, 7–12 February 2020; Volume 34, pp. 606–613. [Google Scholar]
- Aldosari, B. Causes of EHR projects stalling or failing: A study of EHR projects in Saudi Arabia. Comput. Biol. Med. 2017, 91, 372–381. [Google Scholar] [CrossRef]
- Anastas, T.; Waddell, E.N.; Howk, S.; Remiker, M.; Horton-Dunbar, G.; Fagnan, L.J. Building behavioral health homes: Clinician and staff perspectives on creating integrated care teams. J. Behav. Health Serv. Res. 2019, 46, 475–486. [Google Scholar] [CrossRef] [PubMed]
- Crowley, K.; Mishra, A.; Cruz-Cano, R.; Gold, R.; Kleinman, D.; Agarwal, R. Electronic health record implementation findings at a large, suburban health and human services department. J. Public Health Manag. Pract. 2019, 25, E11. [Google Scholar] [CrossRef]
- DrChrono. The EMR of the Future. Less Screen-Time. More Face-Time. Available online: https://www.drchrono.com/electronic-health-record-ehr/ (accessed on 14 September 2022).
- Xiao, C.; Choi, E.; Sun, J. Opportunities and challenges in developing deep learning models using electronic health records data: A systematic review. J. Am. Med. Inform. Assoc. 2018, 25, 1419–1428. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).