Abstract
This work proposes to adapt an existing sensor and embed it on mannequins used in cardiopulmonary resuscitation (CPR) training to accurately measure the amount of air supplied to the lungs during ventilation. The proposed sensor consists of measuring the airflow using propellers. The method directly measures the variable of interest and makes reference to spirometric techniques in the elaboration of its model, improving the realism of the dummies. Besides advantages over the sensors that are commonly used for this purpose, the projected sensor presented an agreement with its theoretical model and with the spirometric model. It is suitable for applications with a resolution of 17 mL, and precision of 50 mL and 26 mL for initial (< 900 mL) and final ranges, respectively.
1. Introduction
Cardiopulmonary resuscitation (CPR) is a recurring practice in medical urgencies and emergencies. CPR is characterized by a set of maneuvers performed in an attempt to reanimate the victim of cardiac and/or respiratory arrest, in order to restore the heart and lung to normal functions while maintaining the oxygenation of the brain. These procedures provide a continuous improvement of the quality of health professionals by using automated dummies in teaching.
The procedures required to perform rescue ventilation in the practice of CPR are in accordance with the parameters of the American Heart Association [1], which establishes a breath every five or six seconds, that is, 10 to 12 breaths per minute. Approximately 500 mL of air enters and leaves the lungs of a healthy young adult in a resting state at each respiratory cycle [2]. Therefore, efficient ventilation should provide such a volume of air to the lungs by mouth-to-mouth or using devices for this purpose.
The pioneers in automating CPR dummies [3] used the Resusci Anne® manikin. Compression and ventilation sensors were developed using digital logic and normally open contacts. The monitoring of the system was done by means of a display panel or indicator lamps, which showed indications of “insufficient”, “acceptable”, and “above acceptable”. Currently, identical models are still widely used [4].
In the present study, it is proposed to measure the volume of air supplied to the lungs in rescue ventilations during CPR by means of a rotor-type flow sensor with propellers. A theoretical model was developed with the intention of making it function equivalent to spirometric models. This brings more realism to the dummies and introduces advantages to possible debriefings after various simulations.
2. Methods
The flow sensor YF-S201 (Sea brand) has been widely used for measuring the water flow in pipes. Figure 1 shows different views of the sensor. It is noteworthy that there is a Hall effect sensor on the flow sensor cover (Figure 1d), which interacts with the magnet of the propeller (Figure 1b). The air flow QIO (inflow and outflow, L/s) passing through it can be described as
where k is a constant equal to (2.61 ± 3) · 10−3 L, calculated according to the sensor dimensions, and f is the frequency of one rotation of its propeller (Hz). Thus, the volumetric flow is
where V is the volume of air (L) flowing inside the lung (reservoir) of the dummy during the time interval ∆t (s) [5,6,7].
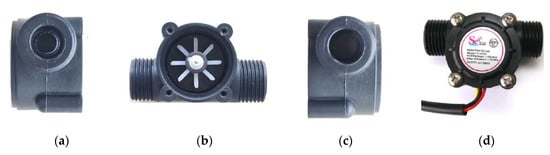
Figure 1.
Flow sensor YF-S201: (a) Input profile; (b) propeller and compartment; (c) output profile; and (d) full view of the sensor.
The sensor reading was developed using the Arduino UNO external interrupts option in conjunction with a real-time operating system.
Spirometry is the measure of the air that enters (inspired) and exits (expired) the lungs. It can be performed during slow breathing or during forced expiratory maneuvers. One of the results generated by this measure is an inspired/expired volume versus time graph [8,9].
3. Results and Discussion
The procedure performed to obtain the curves in Figure 1 is very similar to the calibration of a flow spirometer [8]. Comparing the graphs in Figure 1 with the spirometric model, it can be noted that from zero to the maximum experimental volume, the behavior is in accordance with the spirometer model, characterizing the inspiration. From this point, there is the expiration profile, but experimentally, it is the propeller losing speed until it stops. These results can be used to simulate air exiting the dummies’ lungs, but it is not valid as spirometric data because they do not represent the mirror symmetry of expiration.
It is also verified that there are repeatability and agreement between the results of the measurements carried out under the same conditions. Therefore, for the experiment application, the modeling sensor had a precision up to 50 mL, considering a 95% probability. It was also found that there is accordance between the measurement results and the conventional true values for the measured volume, considering the experimental error. For the true values of 300, 600, 900, 1200, 1500, and 1800 mL; the measurement results were 288, 593, 893, 1162, 1475, and 1755 mL (Figure 2a–f, respectively).
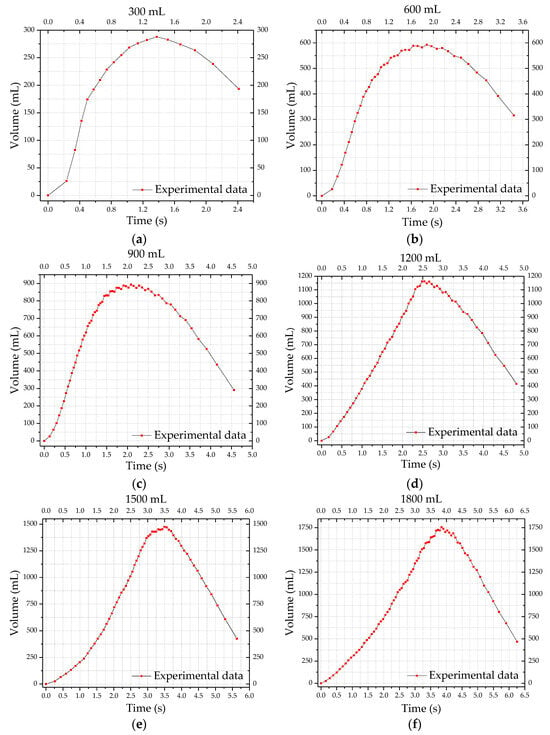
Figure 2.
Result of validation of the YF-S201 sensor with air: (a) 300 mL; (b) 600 mL; (c) 900 mL; (d) 1200 mL; (e) 1500 mL; and (f) 1800 mL.
Comparing measurements performed with the Laerdal® model simultaneously with the model of this study, the latter presents a superior performance when compared to the first one, besides a smaller experimental error. The main advantage of the prepared mechanism lies in the feedback that is expected to generate, in future works, with the model of this experiment, which includes expiration charts based on spirometric models, in order to bring more realism to the simulations and innumerable debriefing possibilities.
4. Conclusions
The performance of the proposed sensor was verified by experiments identical to the calibration of a flow spirometer. It presented resolution of 17 mL, and precision of 50 mL and 26 mL for initial (< 900 mL) and final ranges, respectively [10].
The experiment confirmed that the measurements can be performed in various simulations using the dummies in conjunction with the sensor. It is a cost-effective alternative and relatively easy to adapt to different mannequins. The results were based on spirometric models, bringing more realism to the simulations and bringing numerous possibilities of debriefing. Thus, the sensor has great potential in various future applications.
Acknowledgments
The authors acknowledge the Collective Health Laboratory EMED/UFOP for lending the spirometer.
References
- Association, A.H. Updating the CPR and ACE Guidelines: Highlights of the American Heart Association 2015. Am. Hear. Assoc. 2015, 4–22. [Google Scholar]
- Jorge, A.d.S.; Ribeiro, A.; Gomes, C.; Frederico, C.; Aragão, D.; Gonçalves, F.; Júnior, F.F.; Dantas, I.; Vale, L.; Serafim, M.; et al. Fundamentals of Physics and Biophysics, 1st ed.; FTC EaD: Salvador, BA, Brazil, 2008. [Google Scholar]
- Patrick, H.; Eisenberg, L. An Electronic Resuscitation Evaluation System. IEEE Trans. Biomed. Eng. 1972, BME-19, 317–320. [Google Scholar] [CrossRef]
- Li, H.N.; Wang, Z.T.; Li, X.B. Hardware design of CPR Simulation Control System based on SCM. In Proceedings of the 2011 International Conference on Electrical and Control Engineering, Yichang, China, 16–18 September 2011; pp. 4802–4805. [Google Scholar]
- Munson, B.R.; Yong, D.F.; Okiishi, T.H. Fundamentals of Fluid Mechanics, 4th ed.; Edgard Bluncher: Ames, IA, USA, 2004. [Google Scholar]
- Ribeiro, F.S.; Teixeira, W.L.R. Mathematical Modeling for Real Gases applied to a flooring pipes; Federal University of Espírito Santo—UFES: Vitória, ES, Brazil, December 2008. [Google Scholar]
- Perry, R.H.; Green, D.W.; Maloney, J.O. Perry’s Chemical Engineers’ Handbook, 7th ed.; McGraw-Hill: Lawrence, KS, USA, 1997; Volume 27. [Google Scholar]
- Pereira, C.A.D.C. Spirometry. J. Bras. Pneumol. 2002, 28, S1–S82. [Google Scholar]
- Kulish, V. Human Respiration; WIT Press: Billerica, MA, USA, 2006. [Google Scholar]
- Júnior, A.A.G.; de Sousa, A.R. Fundations of Scientific and Industrial Metrology; Federal University of Santa Catarina — UFSC, Manole: Florianópolis, SC, Brazil, 2008. [Google Scholar]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).