An Unusual Case of Oro-Facial Chronic Pain †
1. Introduction
2. Therapeutically Approach
3. Exercise and Physical Therapies
4. Alternative Therapies
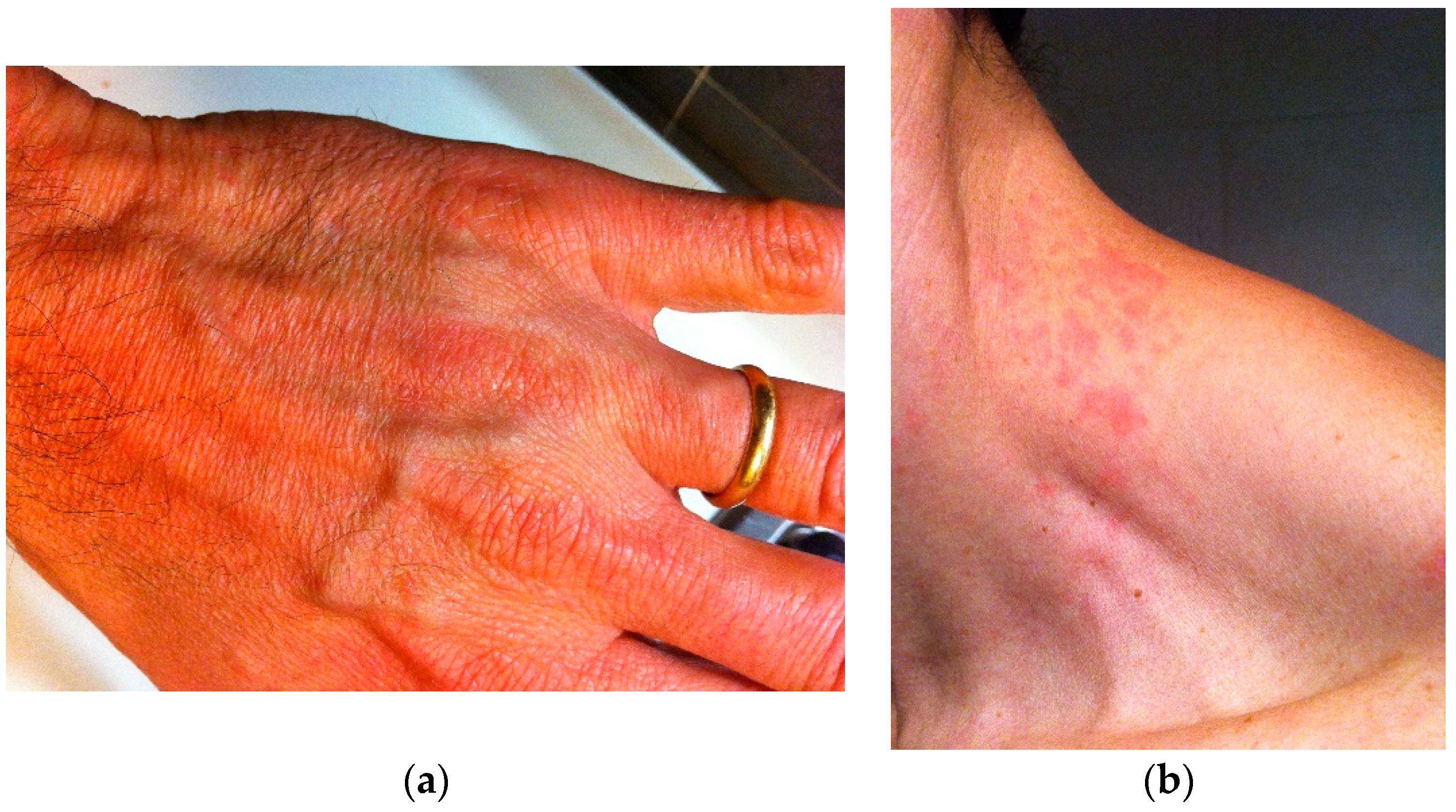
5. Case Report
Conflicts of Interest
References
- Balasubramaniam, R.; Laudenbach, J.M.; Stoopler, E.T. Fibromyalgia: An update for oral health care providers. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2007, 104, 589–602. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, F.; Smythe, H.A.; Yunus, M.B.; Bennett, R.M.; Bombardier, C.; Goldenberg, D.L.; Tugwell, P.; Campbell, S.M.; Abeles, M.; Clark, P.; et al. The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Arthritis Rheum. Off. J. Am. Coll. Rheumatol. 1990, 33, 160–172. [Google Scholar] [CrossRef] [PubMed]
- Goulet, J.P.; Clark, G.T.; Flack, V.F.; Liu, C. The reproducibility of muscle and joint tenderness detection methods and maximum mandibular movement measurement for the temporomandibular system. J. Orofac. Pain 1998, 12, 17–26. [Google Scholar] [PubMed]
- Leblebici, B.; Pektaş, Z.O.; Ortancil, O.; Hürcan, E.C.; Bagis, S.; Akman, M.N. Coexistence of fibromyalgia, temporomandibular disorder, and masticatory myofascial pain syndromes. Rheumatol. Int. 2007, 27, 541–544. [Google Scholar] [CrossRef] [PubMed]
- Plesh, O.; Wolfe, F.; Lane, N. The relationship between fibromyalgia and temporomandibular disorders: Prevalence and symptom severity. J. Rheumatol. 1996, 23, 1948–1952. [Google Scholar] [PubMed]
- Korszun, A.; Papadopoulos, E.; Demitrack, M.; Engleberg, C.; Crofford, L. The relationship between temporomandibular disorders and stress-associated syndromes. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 1998, 86, 416–420. [Google Scholar] [CrossRef] [PubMed]
- Dao, T.T.; Reynolds, W.J.; Tenenbaum, H.C. Comorbidity between myofascial pain of the masticatory muscles and fibromyalgia. J. Orofac. Pain 1997, 11, 232–241. [Google Scholar] [PubMed]
- Aaron, L.A.; Burke, M.M.; Buchwald, D. Overlapping conditions among patients with chronic fatigue syndrome, fibromyalgia, and temporomandibular disorder. Arch. Intern. Med. 2000, 160, 221–227. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lauritano, D.; Lucchese, A.; Petruzzi, M. An Unusual Case of Oro-Facial Chronic Pain. Proceedings 2019, 35, 5. https://doi.org/10.3390/proceedings2019035005
Lauritano D, Lucchese A, Petruzzi M. An Unusual Case of Oro-Facial Chronic Pain. Proceedings. 2019; 35(1):5. https://doi.org/10.3390/proceedings2019035005
Chicago/Turabian StyleLauritano, Dorina, Alberta Lucchese, and Massimo Petruzzi. 2019. "An Unusual Case of Oro-Facial Chronic Pain" Proceedings 35, no. 1: 5. https://doi.org/10.3390/proceedings2019035005
APA StyleLauritano, D., Lucchese, A., & Petruzzi, M. (2019). An Unusual Case of Oro-Facial Chronic Pain. Proceedings, 35(1), 5. https://doi.org/10.3390/proceedings2019035005




