A Computational Approach to Improve the Gathering of Ambient Assisted Living Requirements †
Abstract
:1. Introduction
2. Related Work
3. Methods
4. Results
4.1. What Caregivers Expect
4.2. A Specific Interview with C3
- Sometimes when speaking she forgets words. She is aware of that.
- Routinely forgets dates and times for schedules such as doctors.
- Forgets about tasks she has already done like having breakfast.
- She forgets about ever having been in places like the hospital where she usually goes.
- Has difficulties when she has to take decisions. For example at one time her house flooded and she didn’t knew what to do about it.
- Has had mood changes. It is reported that before she was more grumpy but now she seems more calmed and relaxed.
- She has lower energy drive. Nowadays she is more lazy while before she was always doing things.
4.3. Modeling the C3 Case
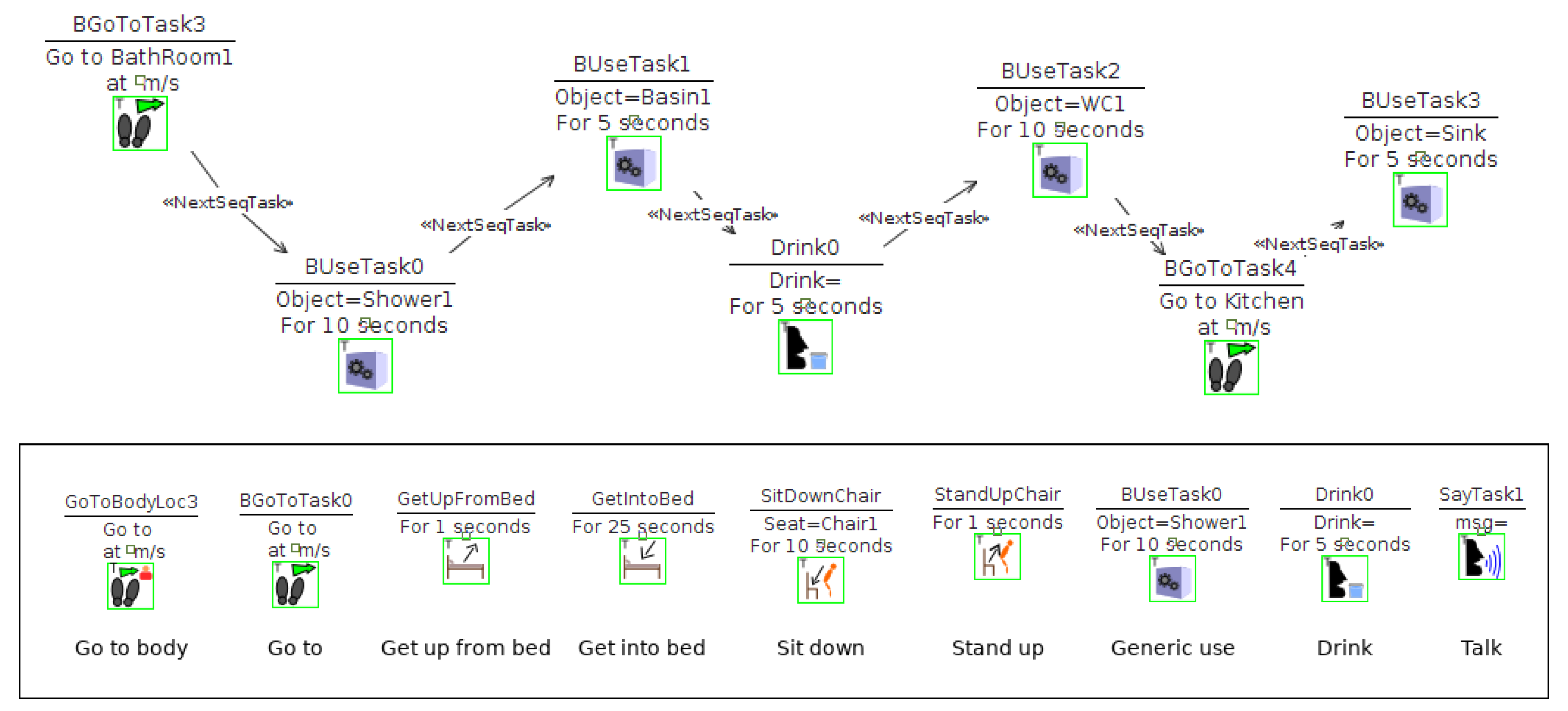
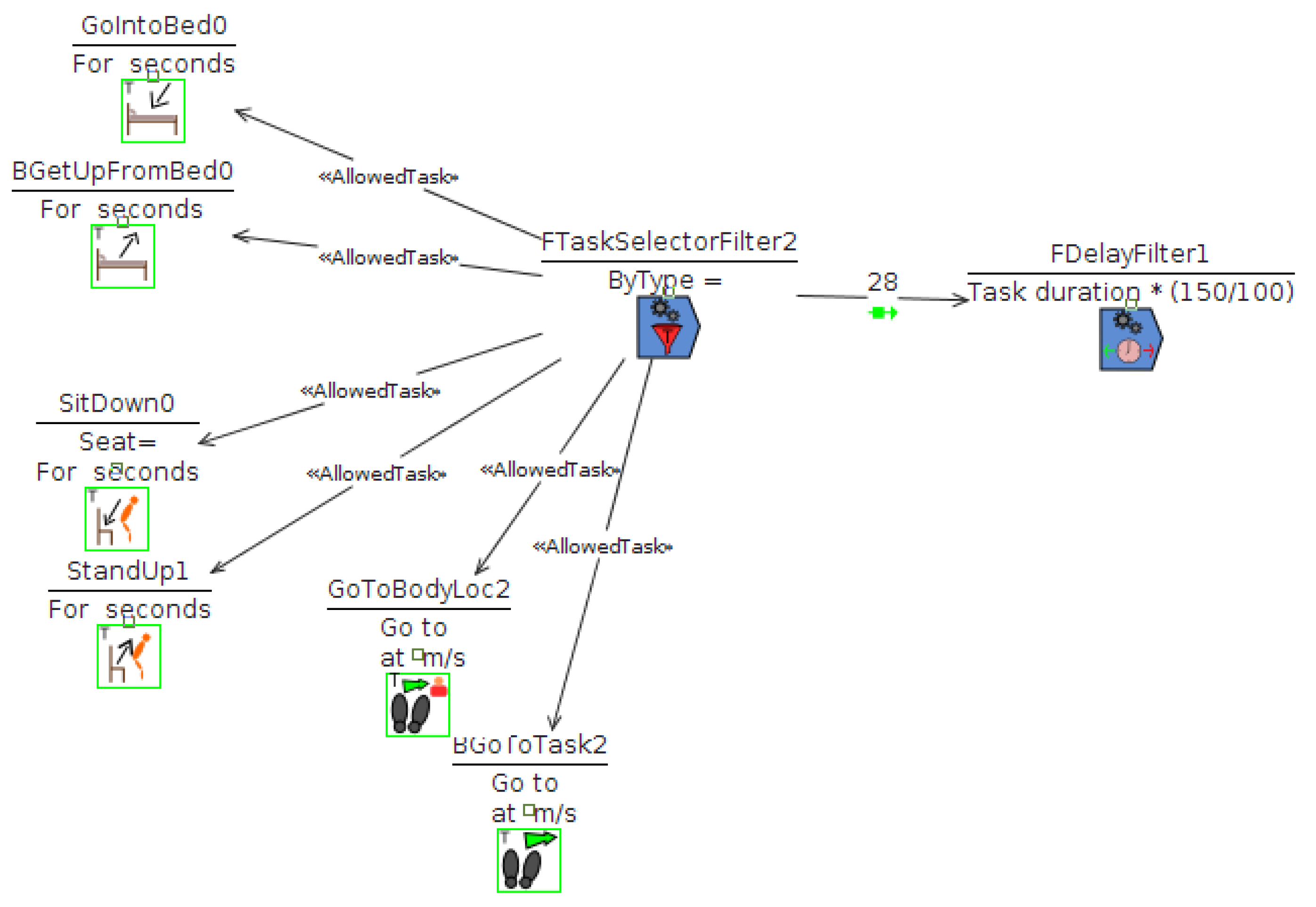
- Scen1—Patient sometimes forgets a task she was about to perform. For this simulation a sequence of tasks was constructed that tries to mimic typical actions performed in the morning such as showering or drinking water. To model this, a filter is then applied that cancels some of the tasks that have to be performed. The movements the agent makes are presented in Figure 2 and they are affected by filters defined in Figure 6.
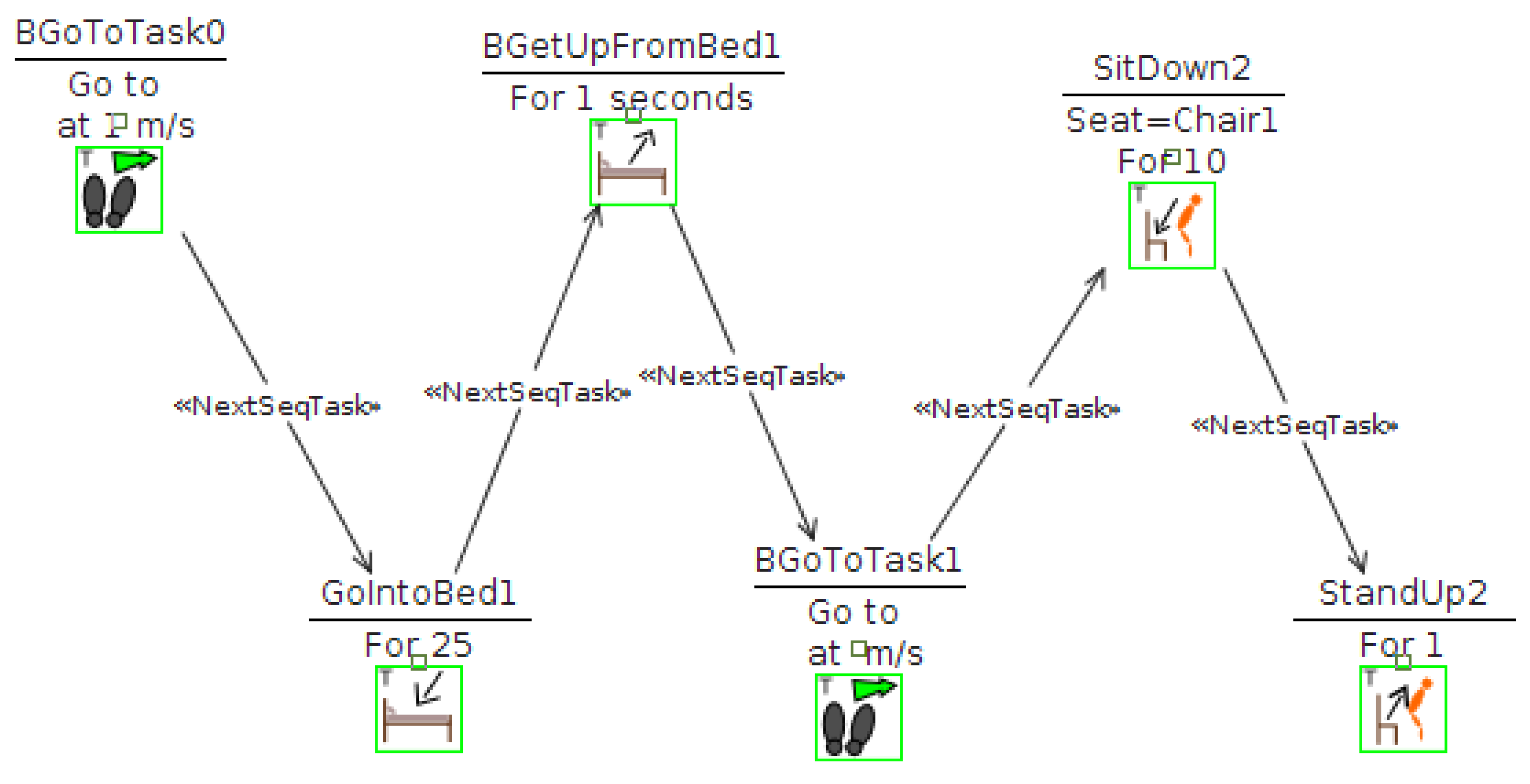
- Scen2—Patient is described as having a lower energy drive. In this case a simple sequence of getting in and out of bed, moving and using a chair was made. A filter is then applied that makes these actions take a longer time. The sequence of movements the agent performs is presented in Figure 3.
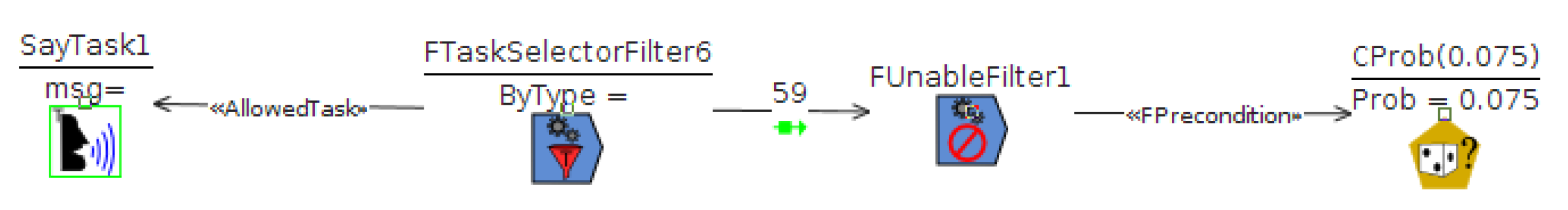
- Scen3—Patient sometimes forgets words. For this case we modeled a conversation and made a filter that makes her unable to speak on occasion. In this case, we try to model a conversation between the caregiver and the patient. See Figure 5.
- Discuss with other stakeholders to what extent the modeled scenarios capture the desired situations. Whether the positive sequence is what it should be and if these or additional effects are necessary. This leads to additional revisions of the specification and new simulations.
- Discuss what solutions could be applicable and evaluate the context each one will have to work on. The effect of the solution can be modeled as well and prototypes can be connected to the simulation. Restoring the without-symptoms status may not be possible, but it could be studied, from the perspective of the caregiver, what contingency actions would be accepted on behalf an AmI solution.
5. Discussion
- The higher precision when describing what happens, when, and where. The situation is different when a person falls in the same room the caregiver is, than when the caregiver is in a different room. Here, it may affect dialogue situations. Is it more difficult when both participants are in different rooms and sound is not reaching each one? AIDE permits to model this kind of situations and explore such situations.
- The benefits of developing the solution over the scenarios. Since there is a computational representation of what should happen (the positive sequence) and what should not happen (the resulting sequence after symptoms are enabled), it is possible to use these simulations as test bed. For instance, the solutions should be able, at least, to identify a negative sequence is in progress. A 3D simulation can produce a similar dataset to the one produced by a real environment, under controlled conditions [22].
- Better communication. Using plain text is risky to ensure the whole sequence is understood. AIDE allows to generate videos that can be commented and delivered to stakeholders. The videos are accompanied by diagrams (like those presented) and additional explanations in form of HTML pages. Also, we use this videos to start other co-creation activities, like focus groups. The videos can be used as motivating scenarios to trigger discussions. We expect this combination to be effective, but no experiments have been made to formally support this claim.
6. Conclusions and Further Research
Funding
Acknowledgments
Conflicts of Interest
References
- Kinney, J.M.; Kart, C.S.; Murdoch, L.D.; Ziemba, T.F. Challenges in caregiving and creative solutions: Using technology to facilitate caring for a relative with dementia. Ageing Int. 2003, 28, 295–313. [Google Scholar] [CrossRef]
- Dignum, V. Responsible Artificial Intelligence: Designing Ai for Human Values. ITU J. ICT Discoveries 2017, 1, 1–8. [Google Scholar]
- Kjeldskov, J.; Graham, C. A review of mobile HCI research methods. In International Conference on Mobile Human-Computer Interaction; Springer: Berlin, Germany, 2003; pp. 317–335. [Google Scholar]
- Rashidi, P.; Mihailidis, A. A survey on ambient-assisted living tools for older adults. IEEE J. Biomed. Health Informat. 2013, 17, 579–590. [Google Scholar] [CrossRef] [PubMed]
- Memon, M.; Wagner, S.R.; Pedersen, C.F.; Beevi, F.H.A.; Hansen, F.O. Ambient assisted living healthcare frameworks, platforms, standards, and quality attributes. Sensors 2014, 14, 4312–4341. [Google Scholar] [CrossRef] [PubMed]
- Prince, M.; Comas-Herrera, A.; Knapp, M.; Guerchet, M.; Karagiannidou, M. World Alzheimer Report 2016: Improving Healthcare for People Living with Dementia: Coverage, Quality and Costs Now and in the Future; Technical Report; Alzheimer’s Disease International: London, UK, 2016. [Google Scholar]
- Kart, C.; Kinney, J.; Murdoch, L.; Ziemba, T. Crossing the Digital Divide: Family Caregiver’S Acceptance of Technology; Scripps Gerontology Center, Miami University: Oxford, OH, USA, 2002. [Google Scholar]
- Kenigsberg, P.A.; Aquino, J.P.; Bérard, A.; Brémond, F.; Charras, K.; Dening, T.; Droës, R.M.; Gzil, F.; Hicks, B.; Innes, A.; et al. Assistive technologies to address capabilities of people with dementia: From research to practice. Dementia 2017, 1471301217714093. [Google Scholar] [CrossRef] [PubMed]
- Topo, P. Technology studies to meet the needs of people with dementia and their caregivers: A literature review. J. Appl. Gerontol. 2009, 28, 5–37. [Google Scholar] [CrossRef]
- Landau, R.; Auslander, G.K.; Werner, S.; Shoval, N.; Heinik, J. Families’ and professional caregivers’ views of using advanced technology to track people with dementia. Qual. Health Res. 2010, 20, 409–419. [Google Scholar] [CrossRef] [PubMed]
- Bruno, F.; Bruno, S.; De Sensi, G.; Luchi, M.L.; Mancuso, S.; Muzzupappa, M. From 3D reconstruction to virtual reality: A complete methodology for digital archaeological exhibition. J. Cult. Herit. 2010, 11, 42–49. [Google Scholar] [CrossRef]
- Campillo-Sánchez, P.; Gómez-Sanz, J.J. Modelling and Simulation of Alzheimer’s Disease Scenarios. Procedia Comput. Sci. 2016, 83, 353–360. [Google Scholar] [CrossRef]
- Nauha, L.; Keränen, N.S.; Kangas, M.; Jämsä, T.; Reponen, J. Assistive technologies at home for people with a memory disorder. Dementia 2016, 1471301216674816. [Google Scholar] [CrossRef] [PubMed]
- Rialle, V.; Ollivet, C.; Guigui, C.; Hervé, C. What do family caregivers of Alzheimer’s disease patients desire in smart home technologies? Methods Inf. Med. 2008, 47, 63–69. [Google Scholar] [PubMed]
- Portet, F.; Vacher, M.; Golanski, C.; Roux, C.; Meillon, B. Design and evaluation of a smart home voice interface for the elderly: Acceptability and objection aspects. Pers. Ubiquitous Comput. 2013, 17, 127–144. [Google Scholar] [CrossRef]
- Hagen, I.; Holthe, T.; Gilliard, J.; Topo, P.; Cahill, S.; Begley, E.; Jones, K.; Duff, P.; Macijauskiene, J.; Budraitiene, A.; et al. Development of a protocol for the assessment of assistive aids for people with dementia. Dementia 2004, 3, 281–296. [Google Scholar] [CrossRef]
- Arntzen, C.; Holthe, T.; Jentoft, R. Tracing the successful incorporation of assistive technology into everyday life for younger people with dementia and family carers. Dementia 2016, 15, 646–662. [Google Scholar] [CrossRef] [PubMed]
- Evans, J.; Brown, M.; Coughlan, T.; Lawson, G.; Craven, M.P. A systematic review of dementia focused assistive technology. In International Conference on Human-Computer Interaction; Springer: Berlin, Germany, 2015; pp. 406–417. [Google Scholar]
- Kitwood, T.M.; Kitwood, T. Dementia Reconsidered: The Person Comes First; Open University Press: Buckingham, UK, 1997; Volume 20. [Google Scholar]
- Coetzer, R. The potential role of relatives in designing person-centred assistive technologies (innovative practice). Dementia 2019, 18, 3161–3164. [Google Scholar] [CrossRef] [PubMed]
- Holbø, K.; Bøthun, S.; Dahl, Y. Safe walking technology for people with dementia: What do they want? In Proceedings of the 15th International ACM SIGACCESS Conference on Computers and Accessibility, Bellevue, WA, USA; 2013; p. 21. [Google Scholar]
- Gómez-Sanz, J.J.; Cardenas, M.; Pax, R.; Campillo, P. Building prototypes through 3D simulations. PAAMS 2016, 25, 299–301. [Google Scholar]






| Social class | Sex | Age | Level of studies | Occupation | Role | |
|---|---|---|---|---|---|---|
| C1 | Upper middle | Man | Secondary | Receptionist | Son | |
| C2 | Upper middle | Woman | 55 | University | Lecturer | Daughter |
| C3 | Middle | Women | 55 | University | Teacher | Niece |
| C4 | Middle | Man | 62 | University | Lecturer | Son-in-law |
| C5 | Upper middle | Woman | 62 | Primary | Homemaker | Daughter |
| C6 | Middle | Woman | 56 | University | Part time teacher | Daughter |
| C7 | Upper middle | Man | 78 | University | Retired computer technician | Husband |
| C8 | Middle | Woman | 39 | University | Graphic designer | Daughter |
| C9 | Middle | Woman | 59 | University | Pharmacist | Daughter |
| C10 | Middle | Man | 56 | Secondary | Bird breeder | Son |
| C11 | Lower middle | Woman | 60 | University | Architectural technologist | Professional caregiver |
| C12 | Upper middle | Woman | 60 | University | Retired teacher | Daughter |
| C13 | Middle | Man | 58 | Secondary | Graphic designer | Son |
| C14 | Lower middle | Woman | 47 | Secondary | House cleaner | Daughter |
| C15 | Middle | Woman | 60 | Primary | Homemaker | Daughter-in-law |
| C16 | Middle | Woman | 65 | Primary | Homemaker | Daughter |
| C17 | Lower middle | Woman | 64 | Primary | Homemaker | Daughter |
| C18 | Upper middle | Woman | 26 | University | Pharmacist | Daughter |
| C19 | Middle | Man | 66 | University | Retired administrative assistant | Husband |
| C20 | Middle | Woman | 56 | Secondary | Retired administrative assistant | Daughter-in-law |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Castillo, N.G.; Pérez, J.L.; Gómez-Sanz, J.J. A Computational Approach to Improve the Gathering of Ambient Assisted Living Requirements. Proceedings 2018, 2, 1246. https://doi.org/10.3390/proceedings2191246
Castillo NG, Pérez JL, Gómez-Sanz JJ. A Computational Approach to Improve the Gathering of Ambient Assisted Living Requirements. Proceedings. 2018; 2(19):1246. https://doi.org/10.3390/proceedings2191246
Chicago/Turabian StyleCastillo, Noelia García, Juan Luis Pérez, and Jorge J. Gómez-Sanz. 2018. "A Computational Approach to Improve the Gathering of Ambient Assisted Living Requirements" Proceedings 2, no. 19: 1246. https://doi.org/10.3390/proceedings2191246
APA StyleCastillo, N. G., Pérez, J. L., & Gómez-Sanz, J. J. (2018). A Computational Approach to Improve the Gathering of Ambient Assisted Living Requirements. Proceedings, 2(19), 1246. https://doi.org/10.3390/proceedings2191246





