Development of Catheter Flow Sensor for Breathing Measurements at Different Levels of Tracheobronchial Airway †
Abstract
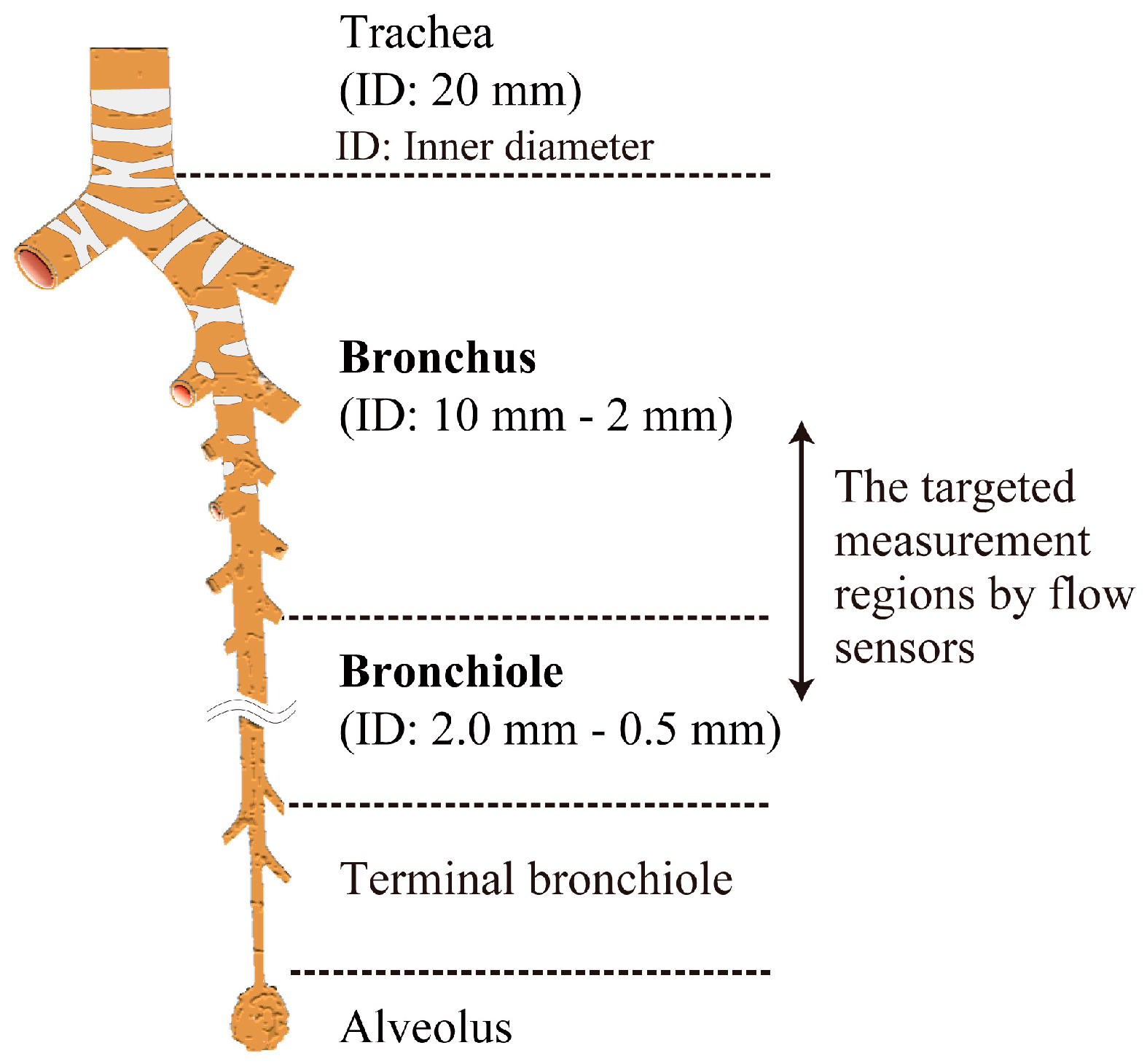
:1. Introduction
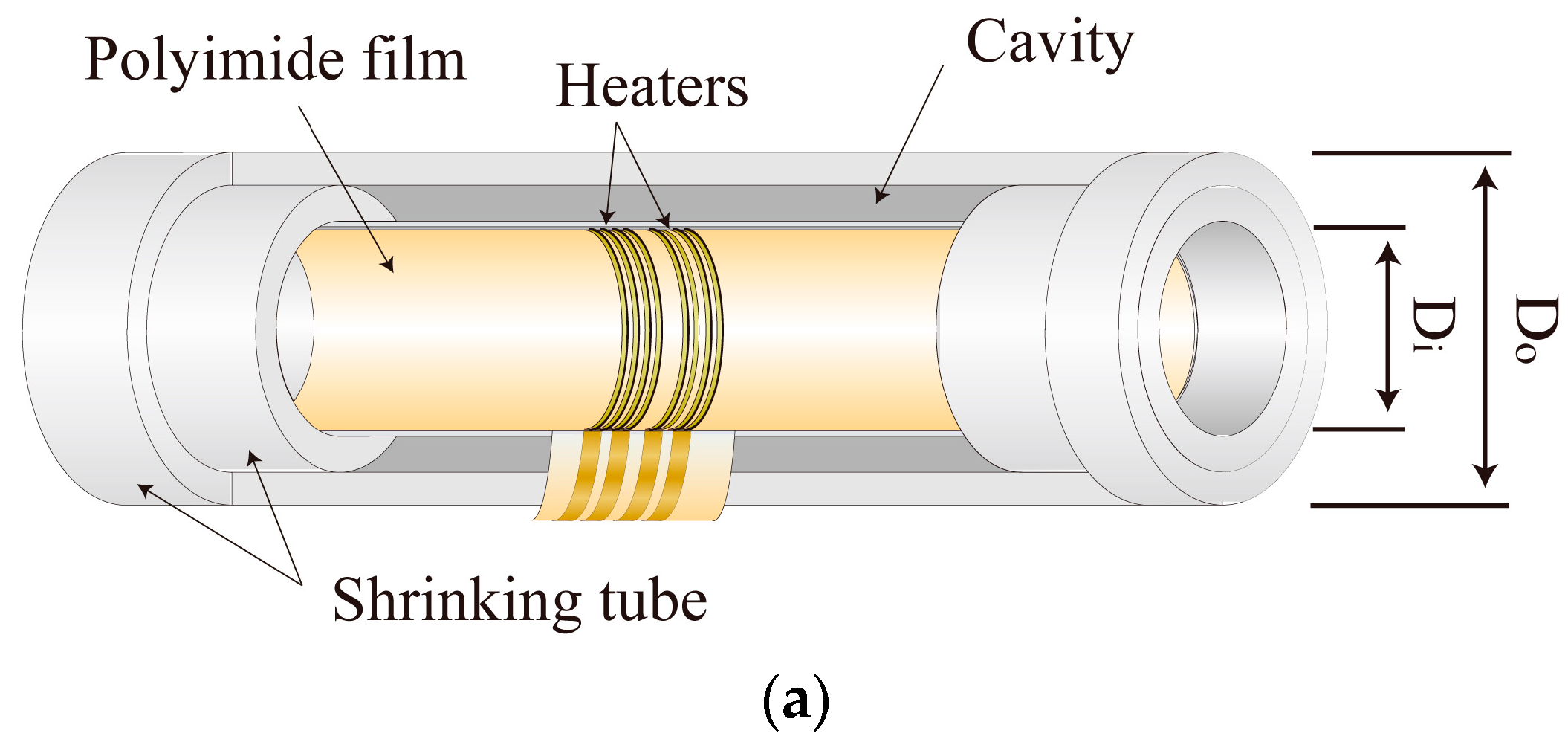
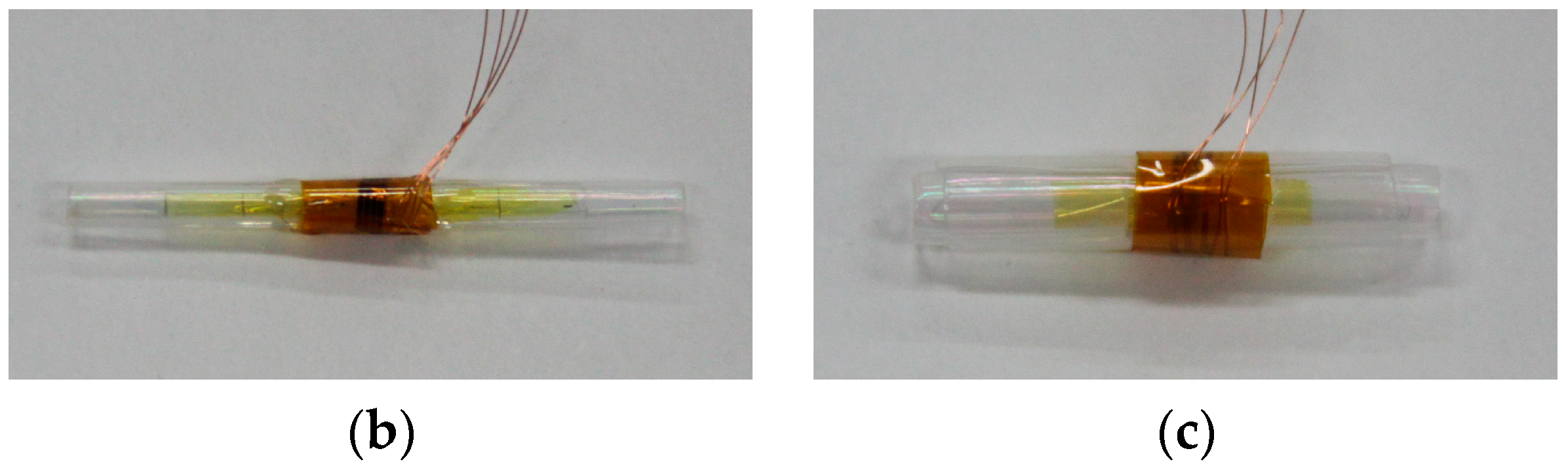
2. Catheter Flow Sensor
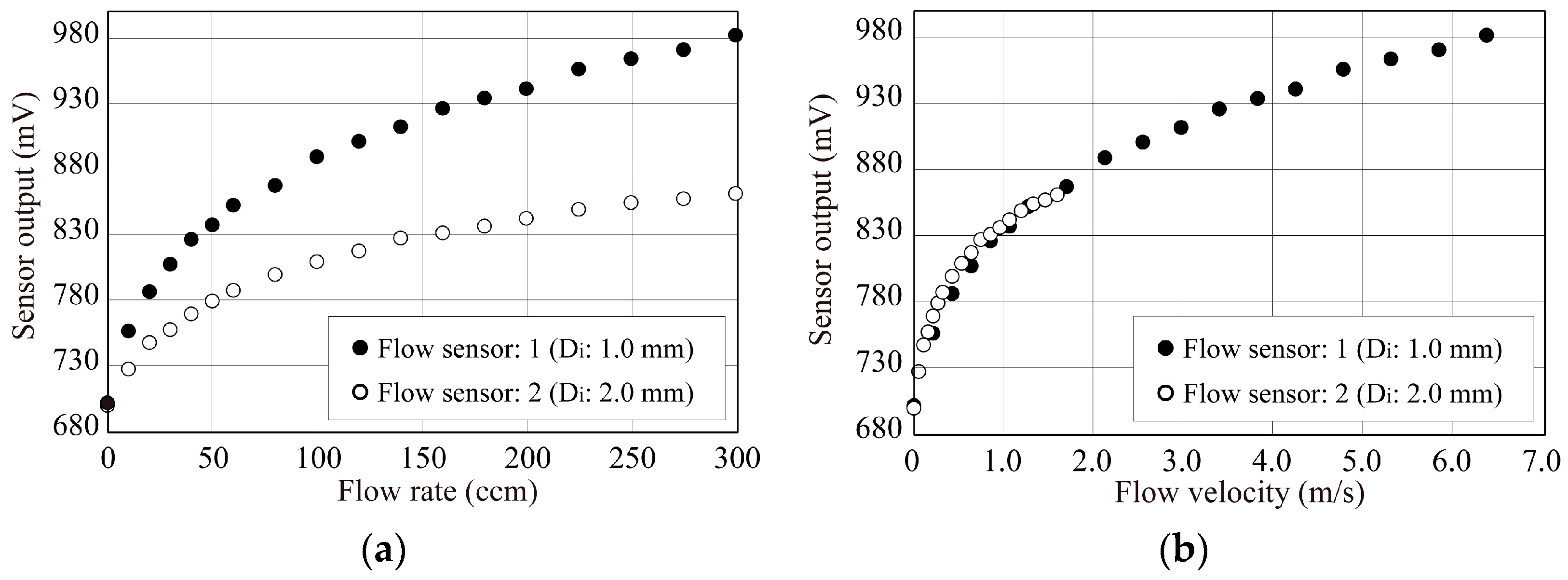
3. Experiments
4. Conclusions
- (1)
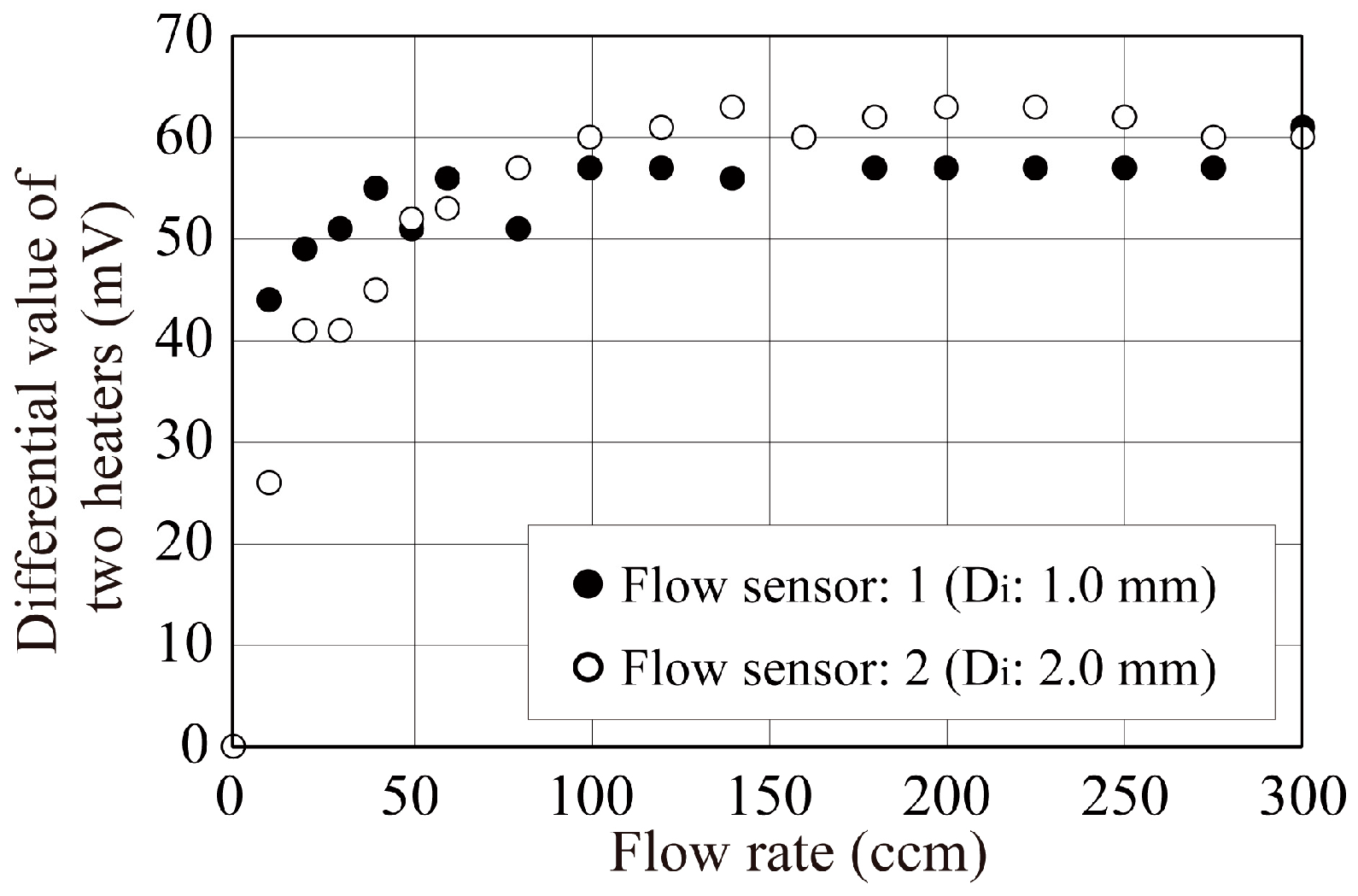
- The sensor outputs were coincident at the same flow velocity condition even if the inner tube diameters were different.
- (2)
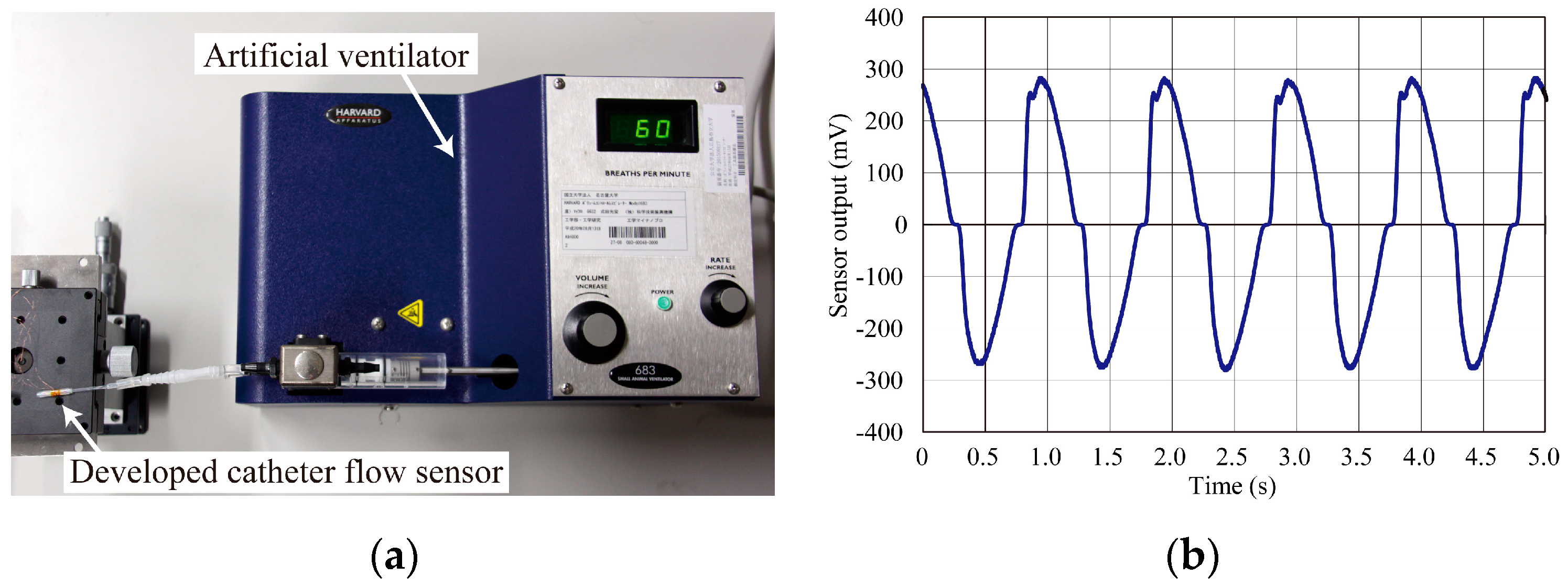
- The developed catheter flow sensors successfully detected the oscillating airflow produced by the ventilator.
Acknowledgments
Conflicts of Interest
References
- Independent Administrative Institution, Environmental Restoration and Conservation Agency. Available online: http://www.erca.go.jp/ (accessed on 11 June 2014).
- Shikida, M.; Naito, J.; Yokota, T.; Kawabe, T.; Hayashi, Y.; Sato, K. A catheter-type flow sensor for measurement of aspirated- and inspired-air characteristics in bronchial region. J. Micromech. Microeng. 2009, 19, 105027. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fujinori, T.; Hasegawa, Y.; Matsushima, M.; Kawabe, T.; Shikida, M. Development of Catheter Flow Sensor for Breathing Measurements at Different Levels of Tracheobronchial Airway. Proceedings 2017, 1, 356. https://doi.org/10.3390/proceedings1040356
Fujinori T, Hasegawa Y, Matsushima M, Kawabe T, Shikida M. Development of Catheter Flow Sensor for Breathing Measurements at Different Levels of Tracheobronchial Airway. Proceedings. 2017; 1(4):356. https://doi.org/10.3390/proceedings1040356
Chicago/Turabian StyleFujinori, Tomohiro, Yoshihiro Hasegawa, Miyoko Matsushima, Tsutomo Kawabe, and Mitsuhiro Shikida. 2017. "Development of Catheter Flow Sensor for Breathing Measurements at Different Levels of Tracheobronchial Airway" Proceedings 1, no. 4: 356. https://doi.org/10.3390/proceedings1040356
APA StyleFujinori, T., Hasegawa, Y., Matsushima, M., Kawabe, T., & Shikida, M. (2017). Development of Catheter Flow Sensor for Breathing Measurements at Different Levels of Tracheobronchial Airway. Proceedings, 1(4), 356. https://doi.org/10.3390/proceedings1040356



