Attempting to Determine the Relationship of Mandibular Third Molars to the Mandibular Canal on Digital Panoramic Radiography; Using CBCT as Gold Standard
Abstract
1. Introduction
2. Materials and Methods
- Patients with any pathology related to the mandibular M3 teeth or the mandibular canal
- Patients who have received any treatment to the mandibular M3 teeth and/or adjacent bone
- Patients who have not completed the root development of the mandibular M3 teeth
- Images with artifacts obscuring the mandibular M3 teeth and/or the mandibular canal
- DPR and/or CBCT images with insufficient diagnostic quality
- Patients who have/have received orthodontic treatment
- Patients with congenital and/or developmental malformations affecting the maxillofacial region
- Patients with fractures, trauma, and/or pathologies affecting the anatomy or integrity of the mandible
- Patients who have a systemic disorder that may affect bone metabolism (hyperparathyroidism, hypoparathyroidism, Paget’s disease, rheumatoid arthritis, etc.) and/or who are using a medication that may cause this
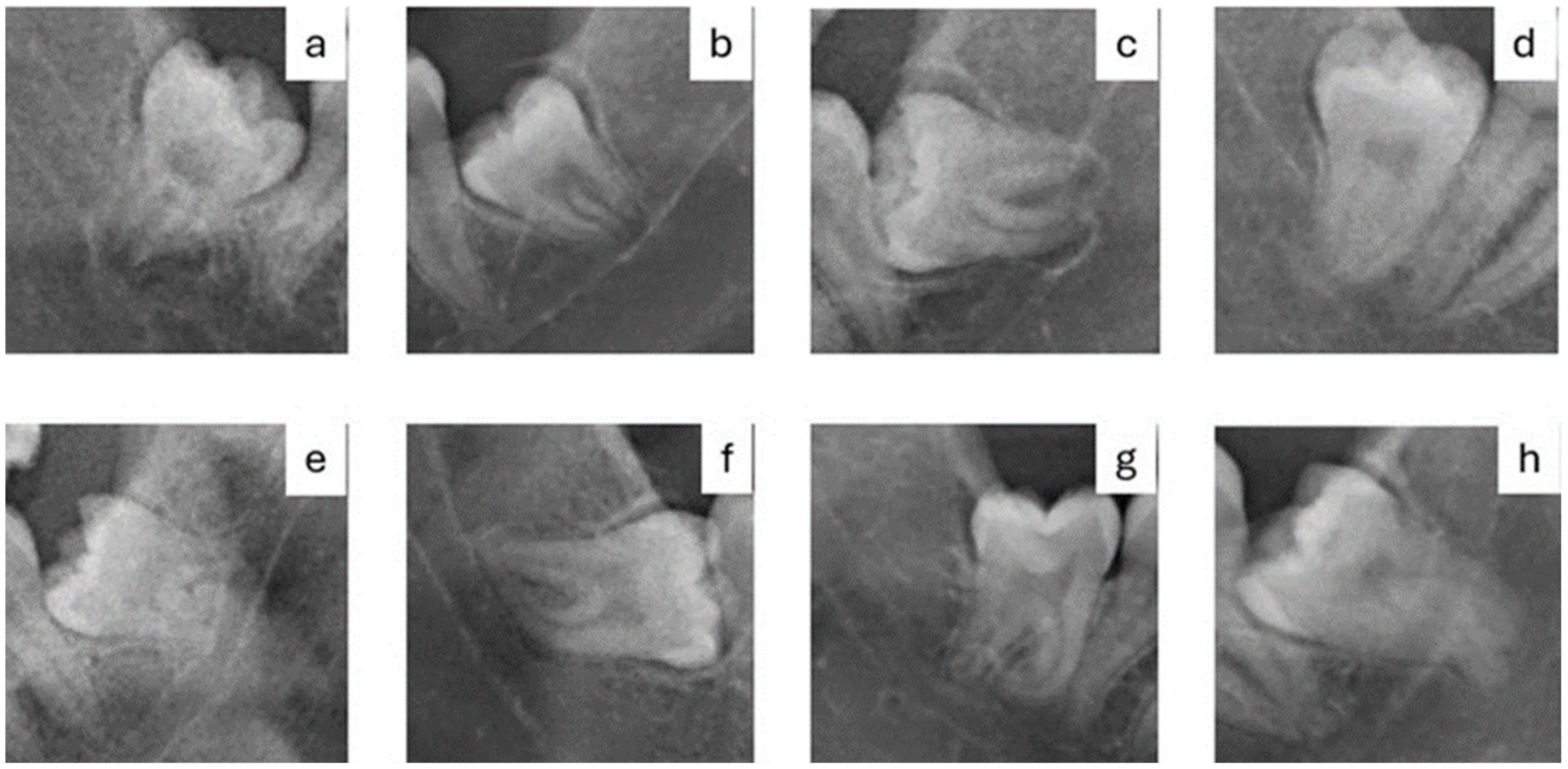
- a)
- Radiolucency at the root
- b)
- Narrowing of the root
- c)
- Radiolucency and bifurcation at the root apex
- d)
- Discontinuity of the mandibular canal cortex
- e)
- Narrowing of the mandibular canal
- f)
- Deviation of the root
- g)
- Deviation of the mandibular canal
- h)
- Superimposition of the root and the mandibular canal (overlapping)
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| M3 | Mandibular third molars |
| DPR | Digital Panoramic Radiography |
| CBCT | Cone Beam Computed Tomography |
| FA | Fractal Analysis |
| HA | Histogram Analysis |
| FD | Fractal Dimension |
| HR | High-Resolution |
| MRI | Magnetic Resonance Imaging |
| MGV | Mean Gray Value |
| TIFF | Tag Image File Format |
| ROI | Regions of Interest |
| EMF | Electromagnetic Field |
| SAR | Specific Absorption Rate |
| ∆T | Temperature Change |
| EC | Electrical Conductivity |
| FEM | Finite Element Modeling |
| AI | Artificial Intelligence |
| EIT | Electrical Impedance Tomography |
References
- Lopes, V.; Mumenya, R.; Feinmann, C.; Harris, M. Third molar surgery: An audit of the indications for surgery, post-operative complaints and patient satisfaction. Br. J. Oral Maxillofac. Surg. 1995, 33, 33–35. [Google Scholar] [CrossRef] [PubMed]
- Patel, P.S.; Shah, J.S.; Dudhia, B.B.; Butala, P.B.; Jani, Y.V.; Macwan, R.S. Comparison of panoramic radiograph and cone beam computed tomography findings for impacted mandibular third molar root and inferior alveolar nerve canal relation. Indian J. Dent. Res. 2020, 31, 91–102. [Google Scholar] [CrossRef]
- Al-Haj Husain, A.; Stadlinger, B.; Winklhofer, S.; Bosshard, F.A.; Schmidt, V.; Valdec, S. Imaging in Third Molar Surgery: A Clinical Update. J. Clin. Med. 2023, 12, 7688. [Google Scholar] [CrossRef]
- Neves, F.S.; Souza, T.C.; Almeida, S.M.; Haiter-Neto, F.; Freitas, D.Q.; Bóscolo, F.N. Correlation of panoramic radiography and cone beam CT findings in the assessment of the relationship between impacted mandibular third molars and the mandibular canal. Dentomaxillofac. Radiol. 2012, 41, 553–557. [Google Scholar] [CrossRef]
- Moreira-Souza, L.; Butini Oliveira, L.; Gaêta-Araujo, H.; Almeida-Marques, M.; Asprino, L.; Oenning, A.C. Comparison of CBCT and panoramic radiography for the assessment of bone loss and root resorption on the second molar associated with third molar impaction: A systematic review. Dentomaxillofac. Radiol. 2022, 51, 20210217. [Google Scholar] [CrossRef]
- Al Ali, S.; Jaber, M. Correlation of panoramic high-risk markers with the cone beam CT findings in the preoperative assessment of the mandibular third molars. J. Dent. Sci. 2020, 15, 75–83. [Google Scholar] [CrossRef]
- Davis, D.; Birnbaum, L.; Ben-Ishai, P.; Taylor, H.; Sears, M.; Butler, T.; Scarato, T. Wireless technologies, non-ionizing electromagnetic fields and children: Identifying and reducing health risks. Curr. Probl. Pediatr. Adolesc. Health Care 2023, 53, 101374. [Google Scholar] [CrossRef] [PubMed]
- Laganà, F.; Bibbò, L.; Calcagno, S.; De Carlo, D.; Pullano, S.A.; Pratticò, D.; Angiulli, G. Smart electronic device-based monitoring of SAR and temperature variations in indoor human tissue interaction. Appl. Sci. 2025, 15, 2439. [Google Scholar] [CrossRef]
- Kato, C.N.; Barra, S.G.; Tavares, N.P.; Amaral, T.M.; Brasileiro, C.B.; Mesquita, R.A.; Abreu, L.G. Use of fractal analysis in dental images: A systematic review. Dentomaxillofac. Radiol. 2020, 49, 20180457. [Google Scholar] [CrossRef]
- White, S.C.; Rudolph, D.J. Alterations of the trabecular pattern of the jaws in patients with osteoporosis. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1999, 88, 628–635. [Google Scholar] [CrossRef]
- Lopes, R.; Betrouni, N. Fractal and multifractal analysis: A review. Med. Image Anal. 2009, 13, 634–649. [Google Scholar] [CrossRef]
- Bhoraskar, M.; Denny, C.; Srikant, N.; Ongole, R.; Archana, M.; Sampath, P. Fractal Dimension and Lacunarity Analysis in the Dentulous and Edentulous Mandibular Posterior Region Using Cone-beam Computed Tomography: A Cross-sectional Retrospective Study. J. Contemp. Dent. Pract. 2024, 25, 581–587. [Google Scholar]
- Plotnick, R.E.; Gardner, R.H.; O’Neill, R.V. Lacunarity indices as measures of landscape texture. Landsc. Ecol. 1993, 8, 201–211. [Google Scholar] [CrossRef]
- Santos, I.G.; Ramos de Faria, F.; da Silva Campos, M.J.; de Barros, B.Á.C.; Rabelo, G.D.; Devito, K.L. Fractal dimension, lacunarity, and cortical thickness in the mandible: Analyzing differences between healthy men and women with cone-beam computed tomography. Imaging Sci. Dent. 2023, 53, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Önem, E.; Baksı, B.G.; Sogur, E. Changes in the fractal dimension, feret diameter, and lacunarity of mandibular alveolar bone during initial healing of dental implants. Int. J. Oral Maxillofac. Implant. 2012, 27, 1009–1013. [Google Scholar]
- Shrout, M.K.; Potter, B.J.; Hildebolt, C.F. The effect of image variations on fractal dimension calculations. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1997, 84, 96–100. [Google Scholar] [CrossRef] [PubMed]
- Dougherty, G.; Henebry, G.M. Lacunarity analysis of spatial pattern in CT images of vertebral trabecular bone for assessing osteoporosis. Med. Eng. Phys. 2002, 24, 129–138. [Google Scholar] [CrossRef]
- Heo, M.S.; Park, K.S.; Lee, S.S.; Choi, S.C.; Koak, J.Y.; Heo, S.J.; Han, C.H.; Kim, J.D. Fractal analysis of mandibular bony healing after orthognathic surgery. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2002, 94, 763–767. [Google Scholar] [CrossRef]
- Parsa, A.; Ibrahim, N.; Hassan, B.; van der Stelt, P.; Wismeijer, D. Bone quality evaluation at dental implant site using multislice CT, micro-CT, and cone beam CT. Clin. Oral Implant. Res. 2015, 26, e1–e7. [Google Scholar] [CrossRef]
- Patsch, J.M.; Burghardt, A.J.; Kazakia, G.; Majumdar, S. Noninvasive imaging of bone microarchitecture. Ann. N. Y. Acad. Sci. 2011, 1240, 77–87. [Google Scholar] [CrossRef]
- Sogur, E.; Baksi, B.G.; Mert, A. The effect of delayed scanning of storage phosphor plates on occlusal caries detection. Dentomaxillofac. Radiol. 2012, 41, 309–315. [Google Scholar] [CrossRef]
- Rood, J.P.; Shehab, B.A. The radiological prediction of inferior alveolar nerve injury during third molar surgery. Br. J. Oral Maxillofac. Surg. 1990, 28, 20–25. [Google Scholar] [CrossRef]
- de Melo Albert, D.G.; Gomes, A.C.; do Egito Vasconcelos, B.C.; de Oliveira e Silva, E.D.; Holanda, G.Z. Comparison of orthopantomographs and conventional tomography images for assessing the relationship between impacted lower third molars and the mandibular canal. J. Oral Maxillofac. Surg. 2006, 64, 1030–1037. [Google Scholar] [CrossRef]
- Nayak, D.S.; Raghavan, S.A.; Birur, P.; Gurudath, S.; Keerthi, G. Determination of proximity of mandibular third molar to mandibular canal using panoramic radiography and cone-beam computed tomography. J. Indian Acad. Oral Med. Radiol. 2017, 29, 273–277. [Google Scholar] [CrossRef]
- Deppe, H.; Ritschl, L.M.; Kleinschmidt, J.; Wagenpfeil, S.; Sculean, A. Contiguity between the mandibular canal and the mandibular third molar in panoramic tomography compared with cone beam computed tomography: A topographic analysis. Quintessence Int. 2019, 50, 470–477. [Google Scholar]
- Khan, I.; Halli, R.; Gadre, P.; Gadre, K.S. Correlation of panoramic radiographs and spiral CT scan in the preoperative assessment of intimacy of the inferior alveolar canal to impacted mandibular third molars. J. Craniofac. Surg. 2011, 22, 566–570. [Google Scholar] [CrossRef] [PubMed]
- Tofangchiha, M.; Koushaei, S.; Mortazavi, M.; Souri, Z.; Alizadeh, A.; Patini, R. Positive Predictive Value of Panoramic Radiography for Assessment of the Relationship of Impacted Mandibular Third Molars with the Mandibular Canal Based on Cone-Beam Computed Tomography: A Cross-Sectional Study. Diagnostics 2021, 11, 1578. [Google Scholar] [CrossRef]
- Monaco, G.; Montevecchi, M.; Bonetti, G.A.; Gatto, M.R.; Checchi, L. Reliability of panoramic radiography in evaluating the topographic relationship between the mandibular canal and impacted third molars. J. Am. Dent. Assoc. 2004, 135, 312–318. [Google Scholar] [CrossRef] [PubMed]
- Elkhateeb, S.M.; Awad, S.S. Accuracy of panoramic radiographic predictor signs in the assessment of proximity of impacted third molars with the mandibular canal. J. Taibah Univ. Med. Sci. 2018, 13, 254–261. [Google Scholar] [CrossRef] [PubMed]
- Tantanapornkul, W.; Okochi, K.; Bhakdinaronk, A.; Ohbayashi, N.; Kurabayashi, T. Correlation of darkening of impacted mandibular third molar root on digital panoramic images with cone beam computed tomography findings. Dentomaxillofac. Radiol. 2009, 38, 11–16. [Google Scholar] [CrossRef]
- Peker, I.; Sarikir, C.; Alkurt, M.T.; Zor, Z.F. Panoramic radiography and cone-beam computed tomography findings in preoperative examination of impacted mandibular third molars. BMC Oral Health 2014, 14, 71. [Google Scholar] [CrossRef]
- Bell, G.W.; Rodgers, J.M.; Grime, R.J.; Edwards, K.L.; Hahn, M.R.; Dorman, M.L.; Keen, W.D.; Stewart, D.J.; Hampton, N. The accuracy of dental panoramic tomographs in determining the root morphology of mandibular third molar teeth before surgery. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2003, 95, 119–125. [Google Scholar] [CrossRef]
- Janovics, K.; Soós, B.; Tóth, Á.; Szalma, J. Is it possible to filter third molar cases with panoramic radiography in which roots surround the inferior alveolar canal? A comparison using cone-beam computed tomography. J. Craniomaxillofac. Surg. 2021, 49, 971–979. [Google Scholar] [CrossRef]
- Versaci, M.; Laganà, F.; Manin, L.; Angiulli, G. Soft computing and eddy currents to estimate and classify delaminations in biomedical device CFRP plates. J. Electr. Eng. 2025, 76, 72–79. [Google Scholar] [CrossRef]
- Arvind, T.R.P.; Jain, R.K.; Nagi, R.; Tiwari, A. Evaluation of Alveolar Bone Microstructure around Impacted Maxillary Canines Using Fractal Analysis in Dravidian Population: A Retrospective CBCT Study. J. Contemp. Dent. Pract. 2022, 23, 593–600. [Google Scholar] [CrossRef] [PubMed]
- Sunal Akturk, E.; Toktas, A.I.; Can, E.; Kosen, E.; Sarica, I. Assessment of the Trabecular Bone Microstructure Surrounding Impacted Maxillary Canines Using Fractal Analysis on Cone-Beam Computed Tomography Images. Diagnostics 2024, 14, 2143. [Google Scholar] [CrossRef] [PubMed]
- Eid, F.Y.; Ghaleb, S.I.; Badr, F.F.; Marzouk, E.S. Three-dimensional assessment of the skeletal characteristics accompanying unilateral maxillary canine impaction: A retrospective cone-beam computed tomography study. BMC Oral Health 2024, 24, 1249. [Google Scholar] [CrossRef] [PubMed]
- Servais, J.A.; Gaalaas, L.; Lunos, S.; Beiraghi, S.; Larson, B.E.; Leon-Salazar, V. Alternative cone-beam computed tomography method for the analysis of bone density around impacted maxillary canines. Am. J. Orthod. Dentofac. Orthop. 2018, 154, 442–449. [Google Scholar] [CrossRef]
- Çakan, K.N.; İpek, İ. A dual approach to third molar complexity: Correlating fractal analysis with the pederson difficulty index—non-clinical research article. BMC Oral Health 2025, 25, 1073. [Google Scholar] [CrossRef]
- Balkan, E.P.; Deniz, H.A.; Kurt, M.H.; Samunahmetoğlu, E.; Karahan, S. Application of fractal analysis in detecting trabecular bone characteristics around mandibular impacted third molars on dental panoramic radiographs. Eur. Ann. Dent. Sci. 2024, 51, 67–73. [Google Scholar] [CrossRef]
- Yasar, F.; Akgünlü, F. Fractal dimension and lacunarity analysis of dental radiographs. Dentomaxillofac. Radiol. 2005, 34, 261–267. [Google Scholar] [CrossRef]
- Köseoğlu Seçgin, C.; Karslıoğlu, H.; Özemre, M.; Orhan, K. Gray value measurement for the evaluation of local alveolar bone density around impacted maxillary canine teeth using cone beam computed tomography. Med. Oral Patol. Oral Cir. Bucal 2021, 26, e669–e675. [Google Scholar] [CrossRef]
- Adiwinarno, B.; Narmada, I.B.; Hamid, T.A. Comparison of Trabecular Bone in Impacted and Normal Erupted Unilateral Maxillary Canine Teeth Using Cone-Beam Computed Tomography in Patients Scheduled for Orthodontic Treatment at the Universitas Airlangga Dental and Oral Hospital. Acta Med. Philipp. 2023, 57, 51–56. [Google Scholar]
- Laganà, F.; Pellicanò, D.; Arruzzo, M.; Pratticò, D.; Pullano, S.A.; Fiorillo, A.S. FEM-Based Modelling and AI-Enhanced Monitoring System for Upper Limb Rehabilitation. Electronics 2025, 14, 2268. [Google Scholar] [CrossRef]
- Langlotz, C.P. The future of AI and informatics in radiology: 10 predictions. Radiology 2023, 309, e231114. [Google Scholar] [CrossRef] [PubMed]
- Laganà, F.; Prattico, D.; De Carlo, D.; Oliva, G.; Pullano, S.A.; Calcagno, S. Engineering Biomedical Problems to Detect Carcinomas: A Tomographic Impedance Approach. Eng 2024, 5, 1594–1614. [Google Scholar] [CrossRef]
- Rani, S.; Bandyopadhyay-Ghosh, S.; Ghosh, S.B.; Liu, G. Advances in sensing technologies for monitoring of bone health. Biosensors 2020, 10, 42. [Google Scholar] [CrossRef] [PubMed]
| Relationship of M3-Mandibular Canal Determined by CBCT | p-Value | |||
|---|---|---|---|---|
| Related (N = 60) | Unrelated (N = 60) | |||
| N (%) | N (%) | |||
| High-risk radiological signs on DPR | Radiolucency at the root | 26 (43.3) | 17 (28.3) | 0.128 |
| Narrowing of the root | 10 (16.6) | 6 (10) | 0.42 | |
| Radiolucency and bifurcation at the root apex | 10 (16.6) | 2 (3.3) | 0.03 * | |
| Discontinuity of the mandibular canal cortex | 27 (45) | 7 (11.6) | 0.00012 * | |
| Narrowing of the mandibular canal | 20 (33.3) | 19 (31.6) | 0.845 | |
| Deviation of the root | 13 (21.6) | 14 (23.3) | 0.920 | |
| Deviation of the mandibular canal | 4 (6.6) | 4 (6.6) | 1.0 | |
| Superimposition of the root and the mandibular canal (overlapping) | 47 (78.3) | 32 (53.3) | 0.007 * | |
| Relationship of M3-Mandibular Canal Determined by CBCT | p-Value | |||
|---|---|---|---|---|
| Related (N = 60) | Unrelated (N = 60) | |||
| Mean ± SD | ||||
| Inside the mandibular canal | FD | 1.136 ± 0.017 | 1.124 ± 0.022 | 0.677 |
| Lacunarity | 0.457 ± 0.015 | 0.403 ± 0.018 | 0.027 * | |
| MGV | 101.313 ± 2.065 | 104.347 ± 1.973 | 0.290 | |
| Relationship of M3-Mandibular Canal Determined by CBCT | p-Value | |||
|---|---|---|---|---|
| Related (N = 60) | Unrelated (N = 60) | |||
| Mean ± SD | ||||
| Outside the mandibular canal | FD | 1.194 ± 0.017 | 1.211 ± 0.020 | 0.523 |
| Lacunarity | 0.407 ± 0.012 | 0.458 ± 0.014 | 0.008 * | |
| MGV | 109.814 ± 1.943 | 111.693 ± 1.849 | 0.485 | |
| Inside the Mandibular Canal | Outside the Mandibular Canal | p-Value | |||
|---|---|---|---|---|---|
| Mean ± SD | |||||
| Relationship of M3-mandibular canal determined by CBCT | Unrelated (N = 60) | FD | 1.124 ± 0.022 | 1.211 ± 0.020 | 0.004 * |
| Lacunarity | 0.403± 0.018 | 0.458 ± 0.014 | 0.020 * | ||
| MGV | 104.347 ± 1.973 | 111.693 ± 1.849 | 0.008 * | ||
| Related (N = 60) | FD | 1.136 ± 0.017 | 1.194 ± 0.017 | 0.018 * | |
| Lacunarity | 0.457 ± 0.015 | 0.407 ± 0.012 | 0.012 * | ||
| MGV | 101.313 ± 2.065 | 109.814 ± 1.942 | 0.003 * | ||
| Relationship of M3-Mandibular Canal Determined by CBCT | p-Value | |||
|---|---|---|---|---|
| Related (N = 60) | Unrelated (N = 60) | |||
| Mean ± SD | ||||
| The difference between the outside and inside measurements | FD | 0.059 ± 0.021 | 0.088 ± 0.027 | 0.398 |
| Lacunarity | −0.050 ± 0.017 | 0.055 ± 0.025 | 0.001 ** | |
| MGV | 8.5 ± 1.9 | 7.3 ± 1.9 | 0.666 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Erkan, H.I.; Yalcin, O.; Pamukcu, U.; Gungor, K. Attempting to Determine the Relationship of Mandibular Third Molars to the Mandibular Canal on Digital Panoramic Radiography; Using CBCT as Gold Standard. Fractal Fract. 2025, 9, 612. https://doi.org/10.3390/fractalfract9090612
Erkan HI, Yalcin O, Pamukcu U, Gungor K. Attempting to Determine the Relationship of Mandibular Third Molars to the Mandibular Canal on Digital Panoramic Radiography; Using CBCT as Gold Standard. Fractal and Fractional. 2025; 9(9):612. https://doi.org/10.3390/fractalfract9090612
Chicago/Turabian StyleErkan, Hilal Isra, Osman Yalcin, Umut Pamukcu, and Kahraman Gungor. 2025. "Attempting to Determine the Relationship of Mandibular Third Molars to the Mandibular Canal on Digital Panoramic Radiography; Using CBCT as Gold Standard" Fractal and Fractional 9, no. 9: 612. https://doi.org/10.3390/fractalfract9090612
APA StyleErkan, H. I., Yalcin, O., Pamukcu, U., & Gungor, K. (2025). Attempting to Determine the Relationship of Mandibular Third Molars to the Mandibular Canal on Digital Panoramic Radiography; Using CBCT as Gold Standard. Fractal and Fractional, 9(9), 612. https://doi.org/10.3390/fractalfract9090612






