Test and Treat Model for Tuberculosis Preventive Treatment among Household Contacts of Pulmonary Tuberculosis Patients in Selected Districts of Maharashtra: A Mixed-Methods Study on Care Cascade, Timeliness, and Early Implementation Challenges
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Setting
2.2.1. General Setting
2.2.2. Specific Setting
2.3. Study Population, Sample Size, and Sampling
2.4. Data Collection, Variables, and Source
2.5. Statistical Analysis
2.6. Ethics Approval
3. Results
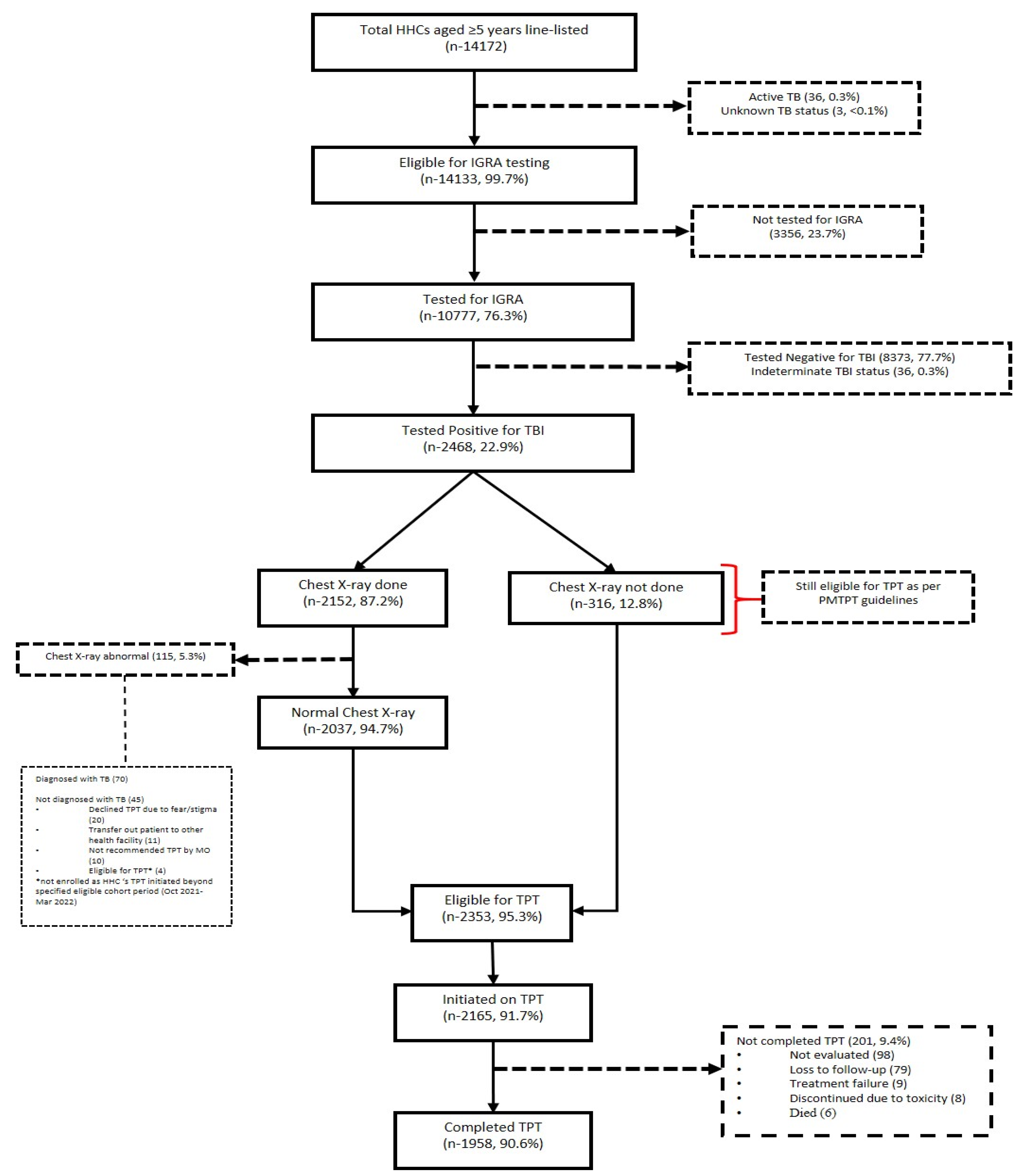
3.1. Quantitative
3.2. Qualitative
3.2.1. Challenges and Suggested Solutions to Improve HHC Screening, Testing, and Assessment for TPT
“had to send samples to Mumbai; do not have any in-district labs; takes at least 72 h to get the test results”; “We screened and sampled them at home. But the HHC need to come to the hospital for X-ray crossing all his barriers”.
“We can finish all the workup at home if there is a point of care testing and a mobile X-ray van that might reduce the time taken for work up”
“HHCs told that why are you asking us to take medicine when we don’t have any symptoms. Though TBI testing report helped in convincing them”.
“our family doctor told that it (TPT) is not necessary”; “the community health officer is not aware of the TPT assessment”
“quite overloaded with the work… over and above we need to enter the same data in excel, google sheet and also in diary…”; “fixing appointment and remembering the pending assessment for more than 5000 HHCs is quite hectic…it needs to be reduced to 1000 HHCs for each of us”
“I cannot take leave. I can come on Saturday or Sunday if the hospital is open”;
“Sometime I have to visit the HHC three times even to motivate them to visit health facility for chest x-ray but some HHC are unable to take leave from work to visit health facility”
3.2.2. Challenges and Suggested Solutions for TPT Initiation, Follow-up, and TPT Completion among HHCs
“Of course, if patient is suffering from diarrhea again and again, nausea, vomiting or loss of appetite, so adherence become little difficult.”; “Patient (HHC) has to take it for six months. And I also have to follow them for six months, instead shorter regimen (3HP: 3 months of combination of isoniazid and rifapentine) can be given to all… that is for only 3 months”; “I called the patient (HHC) to collect the TPT for third month. But the drug was stocked out due to which patient has to wait for some days to collect his medicine (TPT).”
“our doctor told to stop this medicine (TPT) for my son mentioning this is the reason for the current status (HHC is addicted to alcohol)”
“I don’t have money to visit every month to collect the medicine.”; “HHCs concerned about the multiple visits to his home by various staff… they also asked me enquire about them only through direct phone calls to them or through Accredited Social Health Activist (ASHA). Not to enquire through villagers or neighbors.”
“our MIS call them every month to check whether they are taking drugs or not. Some patients (HHCs) don’t take it daily… but they (HHCs) lie to us”
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ministry of Health and Family Welfare Government of India. India TB Report 2022: Coming Together to End TB Together. 2022. Available online: http://www.tbcindia.gov.in (accessed on 17 October 2023).
- World Health Organization. WHO Consolidated Guidelines on Tuberculosis: Tuberculosis Preventive Treatment. 2020. Available online: https://www.who.int/publications/i/item/9789240001503 (accessed on 17 October 2023).
- World Health Organization. A Situational Analysis of Programmatic Management of TB Preventive Treatment. 2020. Available online: https://www.who.int/publications/i/item/9789290228059 (accessed on 17 October 2023).
- Getahun, H.; Matteelli, A.; Chaisson, R.E.; Raviglione, M. Latent Mycobacterium Tuberculosis Infection. N. Engl. J. Med. 2015, 372, 2127–2135. [Google Scholar] [CrossRef] [PubMed]
- Diel, R.; Loddenkemper, R.; Zellweger, J.P.; Sotgiu, G.; D’Ambrosio, L.; Centis, R.; Van Der Werf, M.J.; Dara, M.; Detjen, A.; Gondrie, P.; et al. Old Ideas to Innovate Tuberculosis Control: Preventive Treatment to Achieve Elimination. Eur. Respir. J. 2013, 42, 785–801. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health and Family Welfare, Central Tuberculosis Division. Guidelines for Programmatic Management of TB Preventive Treatment in India. 2021. Available online: https://tbcindia.gov.in/index1.php?lang=1&level=1&sublinkid=5621&lid=3664 (accessed on 18 November 2022).
- World Health Organization. WHO Consolidated Guidelines on Tuberculosis. Module 1; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Alsdurf, H.; Hill, P.C.; Matteelli, A.; Getahun, H.; Menzies, D. The Cascade of Care in Diagnosis and Treatment of Latent Tuberculosis Infection: A Systematic Review and Meta-Analysis. Lancet Infect. Dis 2016, 16, 1269–1278. [Google Scholar] [CrossRef] [PubMed]
- International Union against Tuberculosis and Lung Disease. Project Axshya Plus. Available online: https://theunion.org/our-work/tuberculosis/project-axshya (accessed on 20 November 2022).
- Indian Council of Medical Research; National Institute for Research in Tuberculosis; Ministry of Health and Family Welfare, Government of India; Central TB Division; World Health Organization. National TB Prevalence Survey India 2019–2021. 2022. Available online: https://tbcindia.gov.in/showfile.php?lid=3659 (accessed on 17 October 2023).
- Sagili, K.D.; Muniyandi, M.; Shringarpure, K.; Singh, K.; Kirubakaran, R.; Rao, R.; Tonsing, J.; Sachdeva, K.S.; Tharyan, P. Strategies to Detect and Manage Latent Tuberculosis Infection among Household Contacts of Pulmonary TB Patients in High TB Burden Countries—A Systematic Review and Meta-Analysis. Trop. Med. Int. Health 2022, 27, 842–863. [Google Scholar] [CrossRef] [PubMed]
- Babu, S.P.; Ezhumalai, K.; Raghupathy, K.; Sundaresan, M.; Jain, K.; Narasimhan, P.B.; Knudsen, S.; Horsburgh, C.R.; Hochberg, N.S.; Salgame, P.; et al. Comparison of IGRA and TST in the Diagnosis of Latent Tuberculosis among Women of Reproductive Age in South India. Indian J. Tuberc. 2023, 70, 12–16. [Google Scholar] [CrossRef] [PubMed]
- Corbett, C.; Kulzhabaeva, A.; Toichkina, T.; Kalmambetova, G.; Ahmedov, S.; Antonenka, U.; Iskakova, A.; Kosimova, D.; Migunov, D.; Myrzaliev, B.; et al. Implementing Contact Tracing for Tuberculosis in Kyrgyz Republic and Risk Factors for Positivity Using QuantiFERON-TB Gold Plus. BMC Infect. Dis. 2020, 20, 746. [Google Scholar] [CrossRef] [PubMed]
- Krishnamoorthy, Y.; Ezhumalai, K.; Murali, S.; Rajaa, S.; Jose, M.; Sathishkumar, A.; Soundappan, G.; Horsburgh, C.; Hochberg, N.; Johnson, W.E.; et al. Prevalence and Risk Factors Associated with Latent Tuberculosis Infection among Household Contacts of Smear Positive Pulmonary Tuberculosis Patients in South India. Trop. Med. Int. Health 2021, 26, 1645–1651. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Recommendations for Investigating Contacts of Persons with Infectious Tuberculosis in Low- and Middle-Income Countries. 2012. Available online: https://www.who.int/publications/i/item/9789241504492 (accessed on 13 December 2023).
- Eom, J.S.; Kim, I.; Kim, W.Y.; Jo, E.J.; Mok, J.; Kim, M.H.; Lee, K.; Kim, K.U.; Park, H.K.; Lee, M.K. Household Tuberculosis Contact Investigation in a Tuberculosis-Prevalent Country. Medicine 2018, 97, e9681. [Google Scholar] [CrossRef] [PubMed]
- Pradipta, I.S.; Idrus, L.R.; Probandari, A.; Lestari, B.W.; Diantini, A.; Alffenaar, J.W.C.; Hak, E. Barriers and Strategies to Successful Tuberculosis Treatment in a High-Burden Tuberculosis Setting: A Qualitative Study from the Patient’s Perspective. BMC Public Health 2021, 21, 1903. [Google Scholar] [CrossRef] [PubMed]

| Index PTB Individuals | HHCs * of PTB Individuals | |||
|---|---|---|---|---|
| Characteristics | n | % | n | % |
| Total | 4186 | 100 | 15,290 | 100 |
| Age (years) | ||||
| 0–4 | - | - | 1118 | 7.3 |
| 0–14 | 83 | 1.9 | 2625 | 17.2 |
| 15–24 | 731 | 17.5 | 2749 | 17.9 |
| 25–34 | 592 | 14.2 | 4536 | 29.7 |
| 35–44 | 801 | 19.2 | 101 | 0.6 |
| 45–54 | 649 | 15.5 | 1770 | 11.6 |
| 55–64 | 540 | 12.9 | 1233 | 8.1 |
| ≥65 | 790 | 18.9 | 1158 | 7.6 |
| Not recorded | 4 | 0.1 | - | - |
| Gender | ||||
| Male | 2514 | 60.1 | 7591 | 49.7 |
| Female | 1671 | 39.9 | 7699 | 50.3 |
| Transgender | 1 | 0.02 | ||
| Microbiological confirmation | ||||
| Yes | 2167 | 51.8 | - | - |
| No | 2015 | 48.1 | - | - |
| Not recorded | 4 | 0.1 | - | - |
| Number of HHCs | ||||
| 1–3 | - | - | 4807 | 31.4 |
| 4–6 | - | - | 7020 | 45.9 |
| 6–9 | - | - | 2299 | 15.0 |
| >9 | - | - | 1164 | 7.6 |
| Duration (in Days) between | Median | IQR |
|---|---|---|
| Treatment initiation of index patient and HHC screening (n-12,195/14,172) | 31 | (14, 93) |
| HHC screening and IGRA testing (n-10,777/10,777) | 16 | (3, 53) |
| IGRA testing and TPT initiation (n-2199/2468) | 12 | (7, 23) |
| Treatment initiation of index patient and TPT initiation (n-1648/2468) | 64 | (35, 107.8) |
| HHC screening and TPT initiation (n-2150/2165) | 31 | (14, 68) |
| Initiation and completion of TPT (n-1926/1958)) | 183 | (180, 191) |
| HHC screening and initiation of TB treatment (n-26/40) | 25 | (15.5, 69.8) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mahajan, P.; Soundappan, K.; Singla, N.; Mehta, K.; Nuken, A.; Thekkur, P.; Nair, D.; Rattan, S.; Thakur, C.; Sachdeva, K.S.; et al. Test and Treat Model for Tuberculosis Preventive Treatment among Household Contacts of Pulmonary Tuberculosis Patients in Selected Districts of Maharashtra: A Mixed-Methods Study on Care Cascade, Timeliness, and Early Implementation Challenges. Trop. Med. Infect. Dis. 2024, 9, 7. https://doi.org/10.3390/tropicalmed9010007
Mahajan P, Soundappan K, Singla N, Mehta K, Nuken A, Thekkur P, Nair D, Rattan S, Thakur C, Sachdeva KS, et al. Test and Treat Model for Tuberculosis Preventive Treatment among Household Contacts of Pulmonary Tuberculosis Patients in Selected Districts of Maharashtra: A Mixed-Methods Study on Care Cascade, Timeliness, and Early Implementation Challenges. Tropical Medicine and Infectious Disease. 2024; 9(1):7. https://doi.org/10.3390/tropicalmed9010007
Chicago/Turabian StyleMahajan, Palak, Kathirvel Soundappan, Neeta Singla, Kedar Mehta, Amenla Nuken, Pruthu Thekkur, Divya Nair, Sampan Rattan, Chaturanand Thakur, Kuldeep Singh Sachdeva, and et al. 2024. "Test and Treat Model for Tuberculosis Preventive Treatment among Household Contacts of Pulmonary Tuberculosis Patients in Selected Districts of Maharashtra: A Mixed-Methods Study on Care Cascade, Timeliness, and Early Implementation Challenges" Tropical Medicine and Infectious Disease 9, no. 1: 7. https://doi.org/10.3390/tropicalmed9010007
APA StyleMahajan, P., Soundappan, K., Singla, N., Mehta, K., Nuken, A., Thekkur, P., Nair, D., Rattan, S., Thakur, C., Sachdeva, K. S., & Kalottee, B. (2024). Test and Treat Model for Tuberculosis Preventive Treatment among Household Contacts of Pulmonary Tuberculosis Patients in Selected Districts of Maharashtra: A Mixed-Methods Study on Care Cascade, Timeliness, and Early Implementation Challenges. Tropical Medicine and Infectious Disease, 9(1), 7. https://doi.org/10.3390/tropicalmed9010007






