Trends of Infective Endocarditis at Two Teaching Hospitals: A 12-Year Retrospective Cohort Study in Rio de Janeiro, Brazil
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Setting and Participants
2.2. Infective Endocarditis Diagnosis
2.2.1. Modified Duke Criteria
2.2.2. Echocardiographic Data
2.2.3. Microbiological Data
2.3. Statistical Analysis
2.4. Ethics Statement
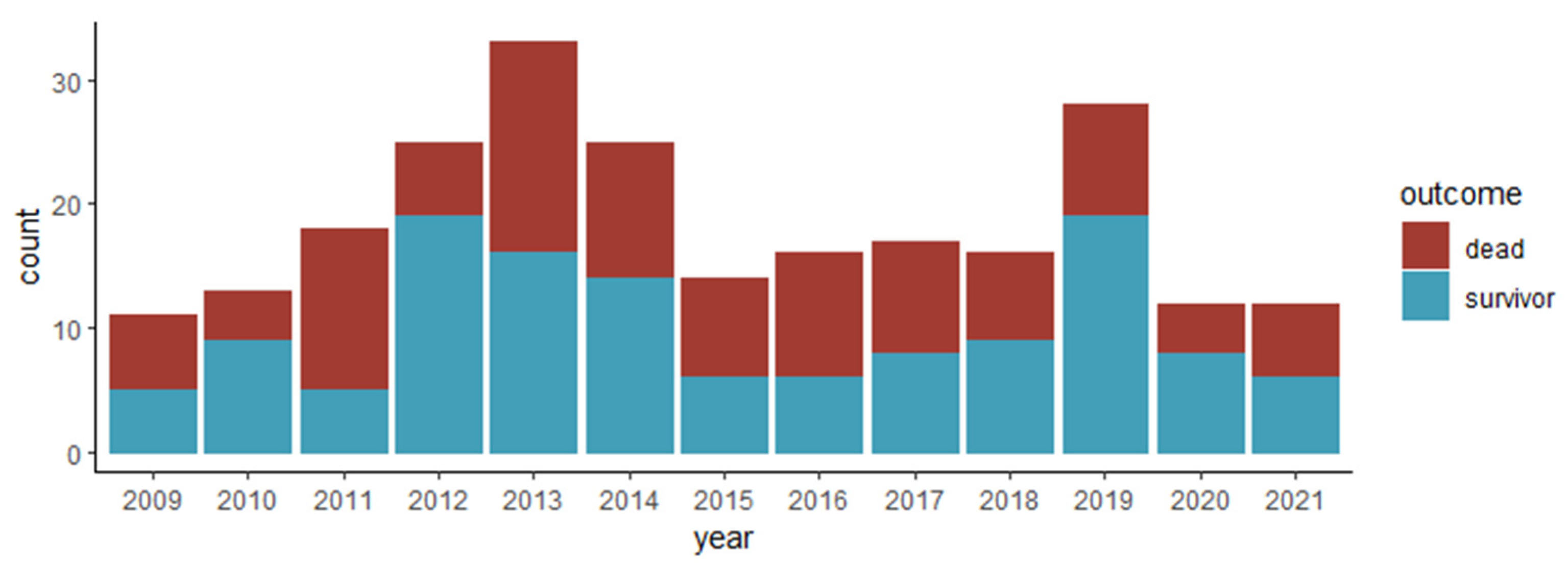
3. Results
3.1. Baseline Characteristics of Patients with Infective Endocarditis
3.2. Etiology
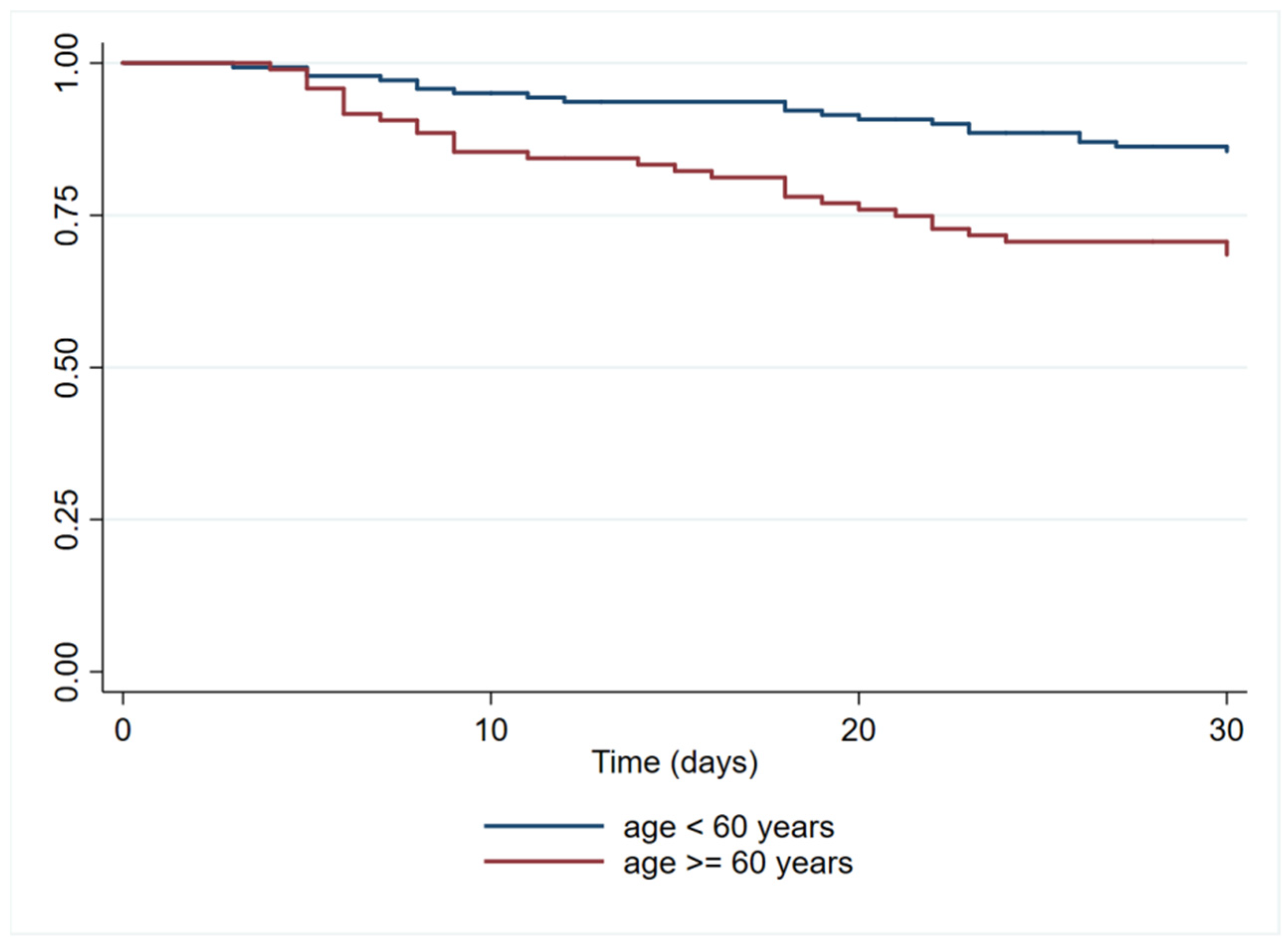
3.3. Mortality Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Habib, G.; Lancellotti, P.; Antunes, M.J.; Bongiorni, M.G.; Casalta, J.P.; Del Zotti, F.; Dulgheru, R.; El Khoury, G.; Erba, P.A.; Iung, B.; et al. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur. Heart J. 2015, 36, 3075–3128. [Google Scholar]
- Mestres, C.A.; Paré, J.C.; Miró, J.M. Organization and Functioning of a Multidisciplinary Team for the Diagnosis and Treatment of Infective Endocarditis: A 30-year Perspective (1985–2014). Rev. Esp. Cardiol. 2015, 68, 363–368. [Google Scholar] [CrossRef]
- Que, Y.A.; Moreillon, P. Infective endocarditis. Nat. Rev. Cardiol. 2011, 8, 322–336. [Google Scholar] [CrossRef]
- Urina-Jassir, M.; Jaimes-Reyes, M.A.; Martinez-Vernaza, S.; Quiroga-Vergara, C.; Urina-Triana, M. Clinical, Microbiological, and Imaging Characteristics of Infective Endocarditis in Latin America: A Systematic Review. Int. J. Infect. Dis. 2022, 117, 312–321. [Google Scholar] [CrossRef]
- Murdoch, D.R.; Corey, G.R.; Hoen, B.; Miró, J.M.; Fowler, V.G., Jr.; Bayer, A.S.; Karchmer, A.W.; Olaison, L.; Pappas, P.A.; Moreillon, P.; et al. Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: The International Collaboration on Endocarditis Prospective Cohort Study. Arch. Intern. Med. 2009, 169, 463–473. [Google Scholar] [CrossRef]
- Nappi, F.; Martuscelli, G.; Bellomo, F.; Singh, S.S.A.; Moon, M.R. Infective endocarditis in high-income countries. Metabolites 2022, 12, 682. [Google Scholar] [CrossRef]
- Bin Abdulhak, A.A.; Baddour, L.M.; Erwin, P.J.; Hoen, B.; Chu, V.H.; Mensah, G.A.; Tleyjeh, I.M. Global and regional burden of infective endocarditis, 1990–2010: A systematic review of the literature. Glob. Heart 2014, 9, 131–143. [Google Scholar] [CrossRef]
- Mutagaywa, R.K.; Vroon, J.C.; Fundikira, L.; Wind, A.M.; Kunambi, P.; Manyahi, J.; Kamuhabwa, A.; Kwesigabo, G.; Chamuleau, S.A.J.; Cramer, M.J.; et al. Infective endocarditis in developing countries: An update. Front. Cardiovasc. Med. 2022, 9, 1007118. [Google Scholar] [CrossRef]
- Spellberg, B.; Chambers, H.F.; Musher, D.M.; Walsh, T.L.; Bayer, A.S. Evaluation of a Paradigm Shift From Intravenous Antibiotics to Oral Step-Down Therapy for the Treatment of Infective Endocarditis: A Narrative Review. JAMA Intern. Med. 2020, 180, 769–777. [Google Scholar] [CrossRef]
- Talha, K.M.; Dayer, M.J.; Thornhill, M.H.; Tariq, W.; Arshad, V.; Tleyjeh, I.M.; Bailey, K.R.; Palraj, R.; Anavekar, N.S.; Sohail, M.R.; et al. Temporal Trends of Infective Endocarditis in North America From 2000 to 2017-A Systematic Review. Open Forum Infect. Dis. 2021, 8, ofab479. [Google Scholar] [CrossRef]
- Damasco, P.V.; Correal, J.C.D.; Cruz-Campos, A.C.D.; Wajsbrot, B.R.; Cunha, R.G.D.; Fonseca, A.G.D.; Castier, M.B.; Fortes, C.Q.; Jazbick, J.C.; Lemos, E.R.S.; et al. Epidemiological and clinical profile of infective endocarditis at a Brazilian tertiary care center: An eight-year prospective study. Rev. Soc. Bras. Med. Trop. 2019, 52, e2018375. [Google Scholar] [CrossRef]
- Ambrosioni, J.; Hernandez-Meneses, M.; Téllez, A.; Pericàs, J.; Falces, C.; Tolosana, J.M.; Vidal, B.; Almela, M.; Quintana, E.; Llopis, J.; et al. The Changing Epidemiology of Infective Endocarditis in the Twenty-First Century. Curr. Infect. Dis. Rep. 2017, 19, 21. [Google Scholar] [CrossRef]
- Li, J.S.; Sexton, D.J.; Mick, N.; Nettles, R.; Fowler, V.G., Jr.; Ryan, T.; Bashore, T.; Corey, G.R. Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin. Infect. Dis. 2000, 30, 633–638. [Google Scholar] [CrossRef]
- Chen, H.; Zhan, Y.; Zhang, K.; Gao, Y.; Chen, L.; Zhan, J.; Chen, Z.; Zeng, Z. The Global, Regional, and National Burden and Trends of Infective Endocarditis From 1990 to 2019: Results From the Global Burden of Disease Study 2019. Front. Med. 2022, 9, 774224. [Google Scholar] [CrossRef]
- Armiñanzas, C.; Fariñas-Alvarez, C.; Zarauza, J.; Muñoz, P.; González Ramallo, V.; Martínez Sellés, M.; Miró Meda, J.M.; Pericás, J.M.; Goenaga, M.Á.; Ojeda Burgos, G.; et al. Role of age and comorbidities in mortality of patients with infective endocarditis. Eur. J. Intern. Med. 2019, 64, 63–71. [Google Scholar] [CrossRef]
- Hadji-Turdeghal, K.; Jensen, A.D.; Bruun, N.E.; Iversen, K.K.; Bundgaard, H.; Smerup, M.; Kober, L.; Østergaard, L.; Fosbøl, E.L. Temporal trends in the incidence of infective endocarditis in patients with a prosthetic heart valve. Open Heart 2023, 10, e002269. [Google Scholar] [CrossRef]
- Ursi, M.P.; Durante Mangoni, E.; Rajani, R.; Hancock, J.; Chambers, J.B.; Prendergast, B. Infective Endocarditis in the Elderly: Diagnostic and Treatment Options. Drugs Aging 2019, 36, 115–124. [Google Scholar] [CrossRef]
- Cresti, A.; Chiavarelli, M.; Scalese, M.; Nencioni, C.; Valentini, S.; Guerrini, F.; D’aiello, I.; Picchi, A.; De Sensi, F.; Habib, G. Epidemiological and mortality trends in infective endocarditis, a 17-year population-based prospective study. Cardiovasc. Diagn. Ther. 2017, 7, 27–35. [Google Scholar] [CrossRef]
- Tramujas Vasconcellos Neumann, L.; Albert, S.M. Aging in Brazil. Gerontologist 2018, 58, 611–617. [Google Scholar] [CrossRef]
- Damasco, P.V.; Ramos, J.N.; Correal, J.C.D.; Potsch, M.V.; Vieira, V.V.; Camello, T.C.F.; Pereira, M.P.; Marques, V.D.; Santos, K.R.N.; Marques, E.A.; et al. Infective endocarditis in Rio de Janeiro, Brazil: A 5-year experience at two teaching hospitals. Infection 2014, 42, 835–842. [Google Scholar] [CrossRef]
- Cahill, T.J.; Baddour, L.M.; Habib, G.; Hoen, B.; Salaun, E.; Pettersson, G.B.; Schäfers, H.J.; Prendergast, B.D. Challenges in Infective Endocarditis. J. Am. Coll. Cardiol. 2017, 69, 325–344. [Google Scholar] [CrossRef]
- Slipczuk, L.; Codolosa, J.N.; Davila, C.D.; Romero-Corral, A.; Yun, J.; Pressman, G.S.; Figueredo, V.M. Infective endocarditis epidemiology over five decades: A systematic review. PLoS ONE 2013, 8, e82665. [Google Scholar] [CrossRef]
- Ferraris, L.; Milazzo, L.; Rimoldi, S.G.; Mazzali, C.; Barosi, A.; Gismondo, M.R.; Vanelli, P.; Cialfi, A.; Sollima, S.; Galli, M.; et al. Epidemiological trends of infective endocarditis in a single center in Italy between 2003–2015. Infect. Dis. 2018, 50, 749–756. [Google Scholar] [CrossRef]
- Escolà-Vergé, L.; Fernández-Hidalgo, N.; Larrosa, M.N.; Fernandez-Galera, R.; Almirante, B. Secular trends in the epidemiology and clinical characteristics of Enterococcus faecalis infective endocarditis at a referral center (2007–2018). Eur. J. Clin. Microbiol. Infect. Dis. 2021, 40, 1137–1148. [Google Scholar] [CrossRef]
- Østergaard, L.; Voldstedlund, M.; Bruun, N.E.; Bundgaard, H.; Iversen, K.; Køber, N.; Christensen, J.J.; Rosenvinge, F.S.; Jarløv, J.O.; Moser, C.; et al. Temporal Changes, Patient Characteristics, and Mortality, According to Microbiological Cause of Infective Endocarditis: A Nationwide Study. J. Am. Heart Assoc. 2022, 11, e025801. [Google Scholar] [CrossRef]
- Shah, A.S.V.; McAllister, D.A.; Gallacher, P.; Astengo, F.; Rodríguez Pérez, J.A.; Hall, J.; Lee, K.K.; Bing, R.; Anand, A.; Nathwani, D.; et al. Incidence, Microbiology, and Outcomes in Patients Hospitalized with Infective Endocarditis. Circulation 2020, 141, 2067–2077. [Google Scholar] [CrossRef]
- Andrade, N.L.; da Cruz Campos, A.C.; Cabral, A.M.; Damasco, P.H.; Lo-Ten-Foe, J.; Rosa, A.C.P.; Damasco, P.V. Infective endocarditis caused by Enterobacteriaceae: Phenotypic and molecular characterization of Escherichia coli and Klebsiella pneumoniae in Rio de Janeiro, Brazil. Braz. J. Microbiol. 2021, 52, 1887–1896. [Google Scholar] [CrossRef]
- Ramos, J.N.; dos Santos, L.S.; Vidal, L.M.; Pereira, P.M.; Salgado, A.A.; Fortes, C.Q.; Vieira, V.V.; Mattos-Guaraldi, A.L.; Júnior, R.H.; Damasco, P.V. A case report and literature overview: Abiotrophia defectiva aortic valve endocarditis in developing countries. Infection 2014, 42, 579–584. [Google Scholar] [CrossRef]
- Tagliari, A.P.; Steckert, G.V.; da Silveira, L.M.V.; Kochi, A.N.; Wender, O.C.B. Infective endocarditis profile, prognostic factors and in-hospital mortality: 6-year trends from a tertiary university center in South America. J. Card. Surg. 2020, 35, 1905–1911. [Google Scholar] [CrossRef]
- Cahill, T.J.; Prendergast, B.D. Infective endocarditis. Lancet 2016, 387, 882–893. [Google Scholar] [CrossRef]
- Bea, C.; Vela, S.; García-Blas, S.; Perez-Rivera, J.A.; Díez-Villanueva, P.; de Gracia, A.I.; Fuertes, E.; Oltra, M.R.; Ferrer, A.; Belmonte, A.; et al. Infective Endocarditis in the Elderly: Challenges and Strategies. J. Cardiovasc. Dev. Dis. 2022, 9, 192. [Google Scholar] [CrossRef] [PubMed]
- Forestier, E.; Fraisse, T.; Roubaud-Baudron, C.; Selton-Suty, C.; Pagani, L. Managing infective endocarditis in the elderly: New issues for an old disease. Clin. Interv. Aging 2016, 11, 1199–1206. [Google Scholar] [CrossRef] [PubMed]
- Babeș, E.E.; Lucuța, D.A.; Petcheși, C.D.; Zaha, A.A.; Ilyes, C.; Jurca, A.D.; Vesa, M.C.; Zaha, D.C.; Babeș, V.V. Clinical Features and Outcome of Infective Endocarditis in a University Hospital in Romania. Medicina 2021, 57, 158. [Google Scholar] [CrossRef]
| Total n = 240 | Survivor n = 130 | Dead n = 110 | p | ||||
|---|---|---|---|---|---|---|---|
| Age (years) * | 55 | (39–66) | 50 | (32–60) | 61 | (48–71) | <0.001 ‡ |
| ≥60 years | 97 | 41% | 36 | 28% | 61 | 55% | <0.001 ¶ |
| Sex | |||||||
| Female | 104 | 43% | 55 | 42% | 49 | 45% | 0.727 ¶ |
| Male | 136 | 57% | 75 | 58% | 61 | 55% | |
| Pre-existing conditions | |||||||
| Charlson comorbidity index ≥ 3 | 99 | 41% | 40 | 31% | 59 | 54% | <0.001 ¶ |
| Chronic kidney disease | 77 | 32% | 36 | 28% | 41 | 37% | 0.113 ¶ |
| Valvular heart disease | 76 | 32% | 40 | 31% | 36 | 33% | 0.745 ¶ |
| History of dialysis | 60 | 25% | 28 | 22% | 32 | 29% | 0.178 ¶ |
| Diabetes | 50 | 21% | 26 | 20% | 24 | 22% | 0.730 ¶ |
| Congenital heart disease | 25 | 10% | 18 | 14% | 7 | 6% | 0.059 ¶ |
| Previous infective endocarditis | 18 | 8% | 6 | 5% | 12 | 11% | 0.065 ¶ |
| Cancer | 17 | 7% | 9 | 7% | 8 | 7% | 0.916 ¶ |
| HIV infection | 13 | 5% | 7 | 5% | 6 | 5% | 0.981 ¶ |
| Intracardiac device | 12 | 5% | 5 | 4% | 7 | 6% | 0.373 ¶ |
| Vegetation † | |||||||
| mitral | 102 | 43% | 50 | 38% | 52 | 47% | 0.169 ¶ |
| aortic | 52 | 22% | 25 | 19% | 27 | 25% | 0.319 ¶ |
| tricuspid | 27 | 11% | 20 | 15% | 7 | 6% | 0.028 ¶ |
| other location | 14 | 6% | 7 | 5% | 7 | 6% | 0.734 ¶ |
| left-sided | 180 | 75% | 88 | 68% | 92 | 84% | 0.004 ¶ |
| Type of valve | |||||||
| native | 186 | 77.5% | 106 | 82% | 80 | 73% | 0.103 ¶ |
| prosthetic | 54 | 22.5% | 24 | 18% | 30 | 27% | |
| Source | |||||||
| Community-associated IE (CAIE) | 111 | 46% | 69 | 53% | 42 | 38% | |
| Healthcare-associated IE (HAIE) | 129 | 54% | 61 | 47% | 68 | 62% | 0.021 ¶ |
| Surgery | |||||||
| Surgical treatment | 69 | 29% | 36 | 28% | 33 | 30% | 0.694 ¶ |
| Number of days of hospitalization * | 45 | (28–78) | 54 | (36–84) | 34 | (18–61) | <0.001 § |
| Number of days until surgery * | 21 | (–35) | 17 | (6–35) | 25 | (10–35) | 0.314 § |
| Microorganism | Total n = 240 | Survivor n = 130 | Dead n = 110 | p | |||
|---|---|---|---|---|---|---|---|
| Staphylococcus aureus | 62 | 26% | 37 | 29% | 25 | 23% | 0.263 * |
| MRSA * | 19 | 8% | 11 | 9% | 8 | 7% | 0.695 * |
| Streptococcus spp. | 49 | 21% | 34 | 27% | 15 | 14% | 0.013 * |
| Viridans group streptococci | 29 | 12% | 21 | 17% | 8 | 7% | 0.030 * |
| Streptococcus bovis group | 12 | 5% | 8 | 6% | 4 | 4% | 0.391 † |
| Enterococcus spp. | 42 | 18% | 14 | 11% | 28 | 25% | 0.004 * |
| Enterococcus faecalis | 33 | 14% | 10 | 8% | 23 | 21% | 0.004 * |
| VRE † | 4 | 4% | 1 | 2% | 3 | 6% | 0.658 † |
| Coagulase negative Staphylococci | 21 | 9% | 10 | 8% | 11 | 10% | 0.556 * |
| Enterobacteriaceae | 11 | 5% | 6 | 5% | 5 | 5% | 0.948 * |
| Fastidious bacteria | 8 | 3% | 5 | 4% | 3 | 3% | 0.728 † |
| Bartonella henselae | 2 | 0.8% | 2 | 1.5% | 0 | 0% | |
| HACEK group | 2 | 0.8% | 2 | 1.5% | 0 | 0% | |
| Abiotrofia defective | 1 | 0.4% | 0 | 0% | 1 | 0.9% | |
| Coxiella burnetii | 1 | 0.4% | 1 | 0.8% | 0 | 0% | |
| Gemella morbillorum | 1 | 0.4% | 0 | 0% | 1 | 0.9% | |
| Microbacterium testaceum | 1 | 0.4% | 0 | 0% | 1 | 0.9% | |
| Fungus | 8 | 3.4% | 4 | 3.2% | 4 | 3.6% | 1.000 † |
| Candida spp. | 7 | 3.0% | 3 | 2.4% | 4 | 3.6% | |
| Rhodotorula mucilaginosa | 1 | 0.4% | 1 | 0.8% | 0 | 0% | |
| Negative | 45 | 19% | 25 | 19% | 20 | 18% | 0.836 * |
| Microorganism | Total n = 240 | CAIE n = 111 | HAIE n = 129 | p | |||
|---|---|---|---|---|---|---|---|
| Staphylococcus aureus | 62 | 26% | 17 | 16% | 45 | 35% | 0.001 * |
| Streptococcus spp. | 49 | 21% | 43 | 39% | 6 | 5% | <0.001 * |
| Viridans group streptococci | 29 | 12% | 28 | 26% | 1 | 1% | <0.001 † |
| Streptococcus bovis group | 12 | 5% | 11 | 10% | 1 | 1% | 0.002 † |
| Enterococcus spp. | 42 | 18% | 10 | 9% | 32 | 25% | 0.001 * |
| Enterococcus faecalis | 33 | 14% | 9 | 8% | 24 | 19% | 0.020 † |
| Coagulase negative staphylococci | 21 | 9% | 10 | 9% | 11 | 9% | 0.875 * |
| Enterobacteriaceae | 11 | 5% | 2 | 2% | 9 | 7% | 0.069 † |
| Fastidious bacteria | 8 | 3% | 6 | 6% | 2 | 2% | 0.148 † |
| Fungus | 8 | 3% | 1 | 1% | 7 | 5% | 0.073 † |
| Negative | 45 | 19% | 23 | 21% | 16 | 13% | 0.075 * |
| Variable | Unadjusted HR (95% CI) | p | Adjusted HR (95% CI) | p | ||
|---|---|---|---|---|---|---|
| Age ≥ 60 years | 2.0 | (1.4–2.9) | 0.000 | 1.9 | (1.2–3.1) | 0.008 |
| CCI score ≥ 3 | 1.6 | (1.1–2.4) | 0.016 | 1.1 | (0.6–1.7) | 0.815 |
| Left-side IE | 1.5 | (0.9–2.6) | 0.036 | 1.5 | (0.9–2.5) | 0.121 |
| HAIE | 1.0 | (0.7–1.5) | 0.996 | 1.1 | (0.7–1.6) | 0.789 |
| Enterococcal IE | 1.2 | (0.8–1.9) | 0.357 | 1.0 | (0.7–1.6) | 0.902 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Damasco, P.V.; Solórzano, V.E.F.; Fortes, N.R.Q.; Setta, D.X.d.B.; Fonseca, A.G.d.; Perez, M.C.A.; Jazbick, J.C.; Gonçalves-Oliveira, J.; Horta, M.A.P.; de Lemos, E.R.S.; et al. Trends of Infective Endocarditis at Two Teaching Hospitals: A 12-Year Retrospective Cohort Study in Rio de Janeiro, Brazil. Trop. Med. Infect. Dis. 2023, 8, 516. https://doi.org/10.3390/tropicalmed8120516
Damasco PV, Solórzano VEF, Fortes NRQ, Setta DXdB, Fonseca AGd, Perez MCA, Jazbick JC, Gonçalves-Oliveira J, Horta MAP, de Lemos ERS, et al. Trends of Infective Endocarditis at Two Teaching Hospitals: A 12-Year Retrospective Cohort Study in Rio de Janeiro, Brazil. Tropical Medicine and Infectious Disease. 2023; 8(12):516. https://doi.org/10.3390/tropicalmed8120516
Chicago/Turabian StyleDamasco, Paulo Vieira, Victor Edgar Fiestas Solórzano, Natália Rodrigues Querido Fortes, Daniel Xavier de Brito Setta, Aloysio Guimaraes da Fonseca, Mario Castro Alvarez Perez, João Carlos Jazbick, Jonathan Gonçalves-Oliveira, Marco Aurélio Pereira Horta, Elba Regina Sampaio de Lemos, and et al. 2023. "Trends of Infective Endocarditis at Two Teaching Hospitals: A 12-Year Retrospective Cohort Study in Rio de Janeiro, Brazil" Tropical Medicine and Infectious Disease 8, no. 12: 516. https://doi.org/10.3390/tropicalmed8120516
APA StyleDamasco, P. V., Solórzano, V. E. F., Fortes, N. R. Q., Setta, D. X. d. B., Fonseca, A. G. d., Perez, M. C. A., Jazbick, J. C., Gonçalves-Oliveira, J., Horta, M. A. P., de Lemos, E. R. S., & Fortes, C. Q. (2023). Trends of Infective Endocarditis at Two Teaching Hospitals: A 12-Year Retrospective Cohort Study in Rio de Janeiro, Brazil. Tropical Medicine and Infectious Disease, 8(12), 516. https://doi.org/10.3390/tropicalmed8120516






