Distinguishing SARS-CoV-2 Infection and Non-SARS-CoV-2 Viral Infections in Adult Patients through Clinical Score Tools
Abstract
1. Introduction
2. Materials and Methods
2.1. Statistical Analysis
2.2. Sample Size
3. Results
3.1. Characteristics of the Study Population
3.2. Comparison of COVID-19 and Influenza/RSV or Dengue
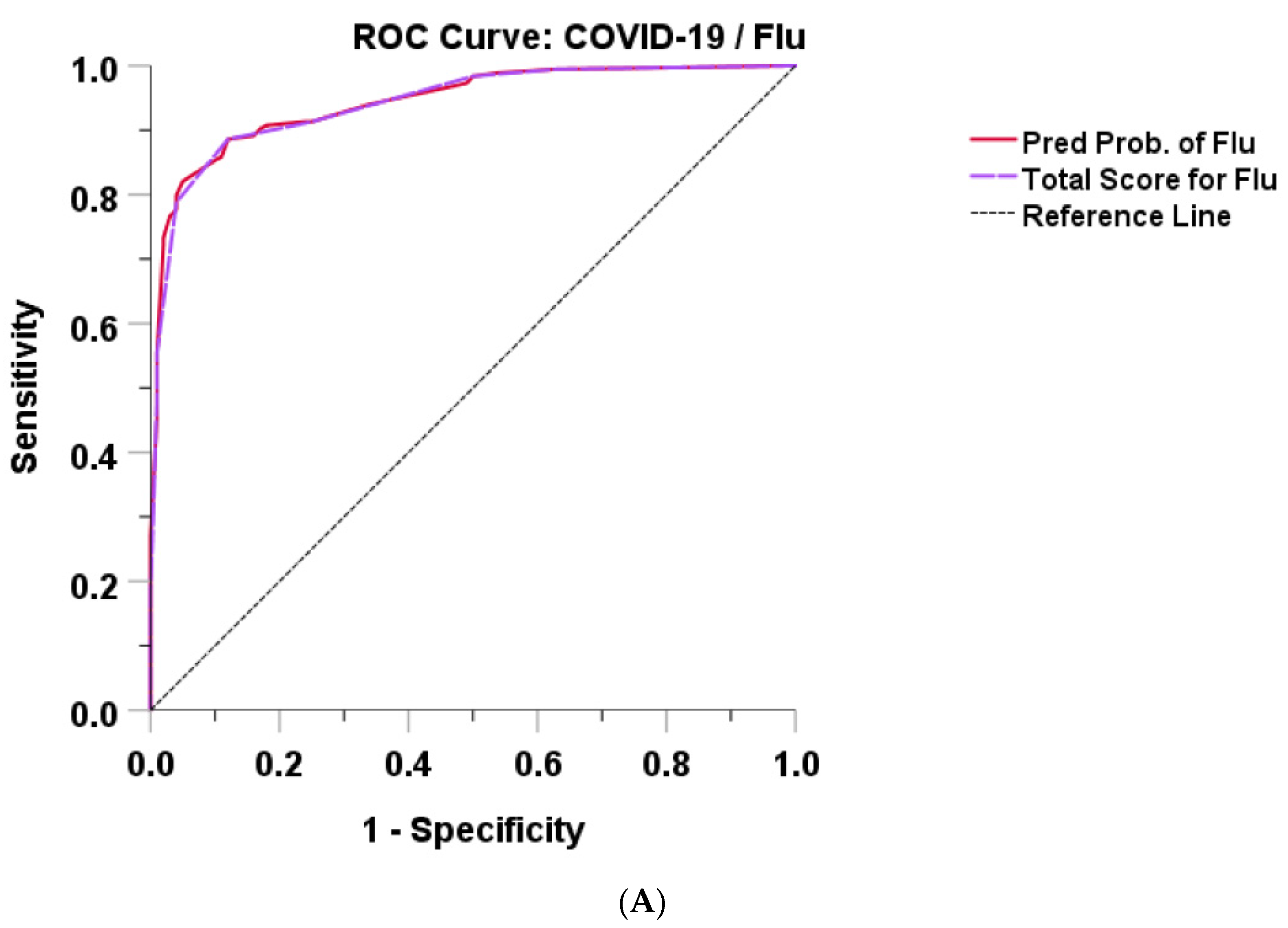
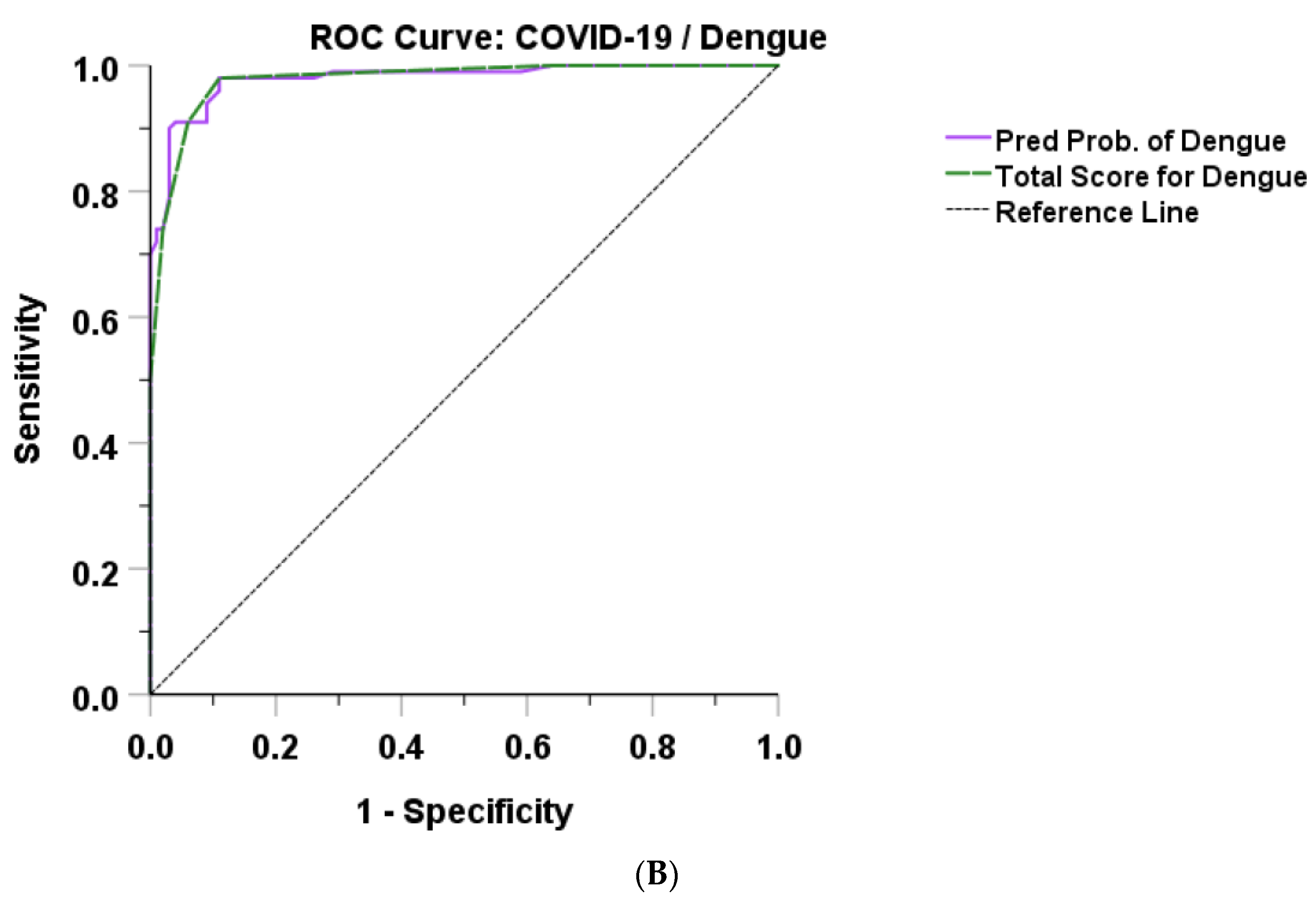
3.3. Model and Score Development
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Coronavirus Disease 2019 (COVID-19) Situation Reports. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (accessed on 10 April 2020).
- Bureau of Information, Ministry of Public Health, Thailand. COVID-19 News. Available online: https://ddc.moph.go.th (accessed on 6 October 2022).
- Brodin, P. Immune determinants of COVID-19 disease presentation and severity. Nat. Med. 2021, 27, 28–33. [Google Scholar] [CrossRef] [PubMed]
- COVID-19 Treatment Guidelines Panel. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. Available online: https://www.covid19treatmentguidelines.nih.gov (accessed on 31 January 2022).
- Bruminhent, J.; Ruangsubvilai, N.; Nabhindhakara, J.; Ingsathit, A.; Kiertiburanakul, S. Clinical characteristics and risk factors for coronavirus disease 2019 (COVID-19) among patients under investigation in Thailand. PLoS ONE 2020, 15, e0239250. [Google Scholar] [CrossRef] [PubMed]
- Costa, J.; Ferreira, E.C.; Santos, C. COVID-19, Chikungunya, Dengue and Zika Diseases: An Analytical Platform Based on MALDI-TOF MS, IR Spectroscopy and RT-qPCR for Accurate Diagnosis and Accelerate Epidemics Control. Microorganisms 2021, 9, 708. [Google Scholar] [CrossRef] [PubMed]
- Sirijatuphat, R.; Suputtamongkol, Y.; Angkasekwinai, N.; Horthongkham, N.; Chayakulkeeree, M.; Rattanaumpawan, P.; Koomanachai, P.; Assanasen, S.; Rongrungruang, Y.; Chierakul, N.; et al. Epidemiology, clinical characteristics, and treatment outcomes of patients with COVID-19 at Thailand’s university-based referral hospital. BMC Infect. Dis. 2021, 21, 382. [Google Scholar] [CrossRef]
- Chittaganpitch, M.; Waicharoen, S.; Yingyong, T.; Praphasiri, P.; Sangkitporn, S.; Olsen, S.J.; Lindblade, K.A. Viral etiologies of influenza-like illness and severe acute respiratory infections in Thailand. Influenza Other Respir. Viruses 2018, 12, 482–489. [Google Scholar] [CrossRef]
- Campbell, K.M.; Lin, C.D.; Iamsirithaworn, S.; Scott, T.W. The complex relationship between weather and dengue virus transmission in Thailand. Am. J. Trop. Med. Hyg. 2013, 89, 1066–1080. [Google Scholar] [CrossRef]
- Department of Disease Control, Ministry of Public Health Thailand. Situation of Vector Borne Diseases in Thailand. Available online: https://ddc.moph.go.th/dvb/ (accessed on 27 December 2022).
- Khongwichit, S.; Chansaenroj, J.; Chirathaworn, C.; Poovorawan, Y. Chikungunya virus infection: Molecular biology, clinicalcharacteristics, and epidemiology in Asian countries. J. Biomed. Sci. 2021, 28, 84. [Google Scholar] [CrossRef]
- Yan, G.; Lee, C.K.; Lam, L.T.M.; Yan, B.; Chua, Y.X.; Lim, A.Y.N.; Phang, K.F.; Kew, G.S.; Teng, H.; Ngai, C.H.; et al. Covert COVID-19 and false-positive dengue serology in Singapore. Lancet Infect. Dis. 2020, 20, 536. [Google Scholar] [CrossRef]
- Garg, I.; Gangu, K.; Shuja, H.; Agahi, A.; Sharma, H.; Bobba, A.; Nasrullah, A.; Chourasia, P.; Pal, S.; Sheikh, A.B.; et al. COVID-19 and Influenza Coinfection Outcomes among Hospitalized Patients in the United States: A Propensity Matched Analysis of National Inpatient Sample. Vaccines 2022, 10, 2159. [Google Scholar] [CrossRef]
- Han, H.; Saed, Y.A.; Song, W.; Wang, M.; Li, Y. Prevalence of Non-SARS-CoV-2 Respiratory Pathogens and Co-Infection with SARS-CoV-2 in the Early Stage of COVID-19 Epidemic. Pathogens 2022, 11, 1292. [Google Scholar] [CrossRef]
- Alhumaid, S.; Alabdulqader, M.; Al Dossary, N.; Al Alawi, Z.; Alnaim, A.A.; Al Mutared, K.M.; Al Noaim, K.; Al Ghamdi, M.A.; Albahrani, S.J.; Alahmari, A.A.; et al. Global Coinfections with Bacteria, Fungi, and Respiratory Viruses in Children with SARS-CoV-2: A Systematic Review and Meta-Analysis. Trop. Med. Infect. Dis. 2022, 7, 380. [Google Scholar] [CrossRef] [PubMed]
- Zepeda-Carrillo, E.A.; Soria Saavedra, F.M.; Mercado Villegas, M.B.; López Alvarado, A.; Regla-Nava, J.A.; Torres-Valadez, R. SARS-CoV-2 and Dengue Virus Coinfection in a Mexican Pediatric Patient: A Case Report from Early Molecular Diagnosis. Pathogens 2022, 11, 1360. [Google Scholar] [CrossRef] [PubMed]
- Anderson, K.B.; Simasathien, S.; Watanaveeradej, V.; Weg, A.L.; Ellison, D.W.; Suwanpakdee, D.; Klungthong, C.; Phonpakobsin, T.; Kerdpanich, P.; Phiboonbanakit, D.; et al. Clinical and laboratory predictors of influenza infection among individuals with influenza-like illness presenting to an urban Thai hospital over a five-year period. PLoS ONE 2018, 13, e0193050. [Google Scholar] [CrossRef] [PubMed]
- Muller, D.A.; Depelsenaire, A.C.; Young, P.R. Clinical and Laboratory Diagnosis of Dengue Virus Infection. J. Infect. Dis. 2017, 215, S89–S95. [Google Scholar] [CrossRef] [PubMed]
- Rahman, M.M.; Been Sayed, S.J.; Moniruzzaman, M.; Kabir, A.; Mallik, M.U.; Hasan, M.R.; Siddique, A.B.; Hossain, M.A.; Uddin, N.; Hassan, M.M.; et al. Clinical and Laboratory Characteristics of an Acute Chikungunya Outbreak in Bangladesh in 2017. Am. J. Trop. Med. Hyg. 2019, 100, 405–410. [Google Scholar] [CrossRef] [PubMed]
- Noorbakhsh, F.; Abdolmohammadi, K.; Fatahi, Y.; Dalili, H.; Rasoolinejad, M.; Rezaei, F.; Salehi-Vaziri, M.; Shafiei-Jandaghi, N.Z.; Gooshki, E.S.; Zaim, M.; et al. Zika Virus Infection, Basic and Clinical Aspects: A Review Article. Iran. J. Public Health 2019, 48, 20–31. [Google Scholar] [CrossRef]
- Azeredo, E.L.; Dos Santos, F.B.; Barbosa, L.S.; Souza, T.M.A.; Badolato-Corrêa, J.; Sánchez-Arcila, J.C.; Nunes, P.C.G.; de-Oliveira-Pinto, L.M.; de Filippis, A.M.; Dal Fabbro, M.; et al. Clinical and Laboratory Profile of Zika and Dengue Infected Patients: Lessons Learned From the Co-circulation of Dengue, Zika and Chikungunya in Brazil. PLoS Curr. 2018, 10. [Google Scholar] [CrossRef]
- Chuaychoo, B.; Ngamwongwan, S.; Kaewnaphan, B.; Athipanyasilp, N.; Horthongkham, N.; Kantakamalakul, W.; Muangman, N. Clinical manifestations and outcomes of respiratory syncytial virus infection in adult hospitalized patients. J. Clin. Virol. 2019, 117, 103–108. [Google Scholar] [CrossRef]
- Bujang, M.A.; Sa’at, N.; Sidik, T.; Joo, L.C. Sample Size Guidelines for Logistic Regression from Observational Studies with Large Population: Emphasis on the Accuracy Between Statistics and Parameters Based on Real Life Clinical Data. Malays. J. Med. Sci. 2018, 25, 122–130. [Google Scholar] [CrossRef]
- Waggoner, J.J.; Gresh, L.; Vargas, M.J.; Ballesteros, G.; Tellez, Y.; Soda, K.J.; Sahoo, M.K.; Nuñez, A.; Balmaseda, A.; Harris, E.; et al. Viremia and Clinical Presentation in Nicaraguan Patients Infected with Zika Virus, Chikungunya Virus, and Dengue Virus. Clin. Infect. Dis. 2016, 63, 1584–1590. [Google Scholar] [CrossRef]
- Cao, B.; Li, X.W.; Mao, Y.; Wang, J.; Lu, H.Z.; Chen, Y.S.; Liang, Z.A.; Liang, L.; Zhang, S.J.; Zhang, B.; et al. Clinical features of the initial cases of 2009 pandemic influenza A (H1N1) virus infection in China. N. Engl. J. Med. 2009, 361, 2507–2517. [Google Scholar] [CrossRef]
- Choreño-Parra, J.A.; Jiménez-Álvarez, L.A.; Cruz-Lagunas, A.; Rodríguez-Reyna, T.S.; Ramírez-Martínez, G.; Sandoval-Vega, M.; Hernández-García, D.L.; Choreño-Parra, E.M.; Balderas-Martínez, Y.I.; Martinez-Sánchez, M.E.; et al. Clinical and Immunological Factors That Distinguish COVID-19 From Pandemic Influenza A(H1N1). Front. Immunol. 2021, 12, 593595. [Google Scholar] [CrossRef]
- Hedberg, P.; Karlsson Valik, J.; van der Werff, S.; Tanushi, H.; Requena Mendez, A.; Granath, F.; Bell, M.; Mårtensson, J.; Dyrdak, R.; Hertting, O.; et al. Clinical phenotypes and outcomes of SARS-CoV-2, influenza, RSV and seven other respiratory viruses: A retrospective study using complete hospital data. Thorax 2022, 77, 154–163. [Google Scholar] [CrossRef] [PubMed]
- Wu, D.; Lu, J.; Liu, Q.; Ma, X.; He, W. To alert coinfection of COVID-19 and dengue virus in developing countries in the dengue-endemic area. Infect. Control. Hosp. Epidemiol. 2020, 41, 1482. [Google Scholar] [CrossRef]
- Nath, H.; Mallick, A.; Roy, S.; Sukla, S.; Basu, K.; De, A.; Biswas, S. Archived dengue serum samples produced false-positive results in SARS-CoV-2 lateral flow-based rapid antibody tests. J. Med. Microbiol. 2021, 70, 001369. [Google Scholar] [CrossRef] [PubMed]
- Rosso, F.; Parra-Lara, L.G.; Agudelo-Rojas, O.L.; Martinez-Ruiz, D.M. Differentiating Dengue from COVID-19: Comparison of Cases in Colombia. Am. J. Trop. Med. Hyg. 2021, 105, 745–750. [Google Scholar] [CrossRef]
- Thein, T.L.; Ang, L.W.; Young, B.E.; Chen, M.I.; Leo, Y.S.; Lye, D.C.B. Differentiating coronavirus disease 2019 (COVID-19) from influenza and dengue. Sci. Rep. 2021, 11, 19713. [Google Scholar] [CrossRef]
- Luvira, V.; Leaungwutiwong, P.; Thippornchai, N.; Thawornkuno, C.; Chatchen, S.; Chancharoenthana, W.; Tandhavanant, S.; Muangnoicharoen, S.; Piyaphanee, W.; Chantratita, N. False Positivity of Anti-SARS-CoV-2 Antibodies in Patients with Acute Tropical Diseases in Thailand. Trop. Med. Infect. Dis. 2022, 7, 132. [Google Scholar] [CrossRef]

| Type of Viral Infection | ||||||
|---|---|---|---|---|---|---|
| COVID-19 | Influenza | RSV | Dengue | Chikungunya | Zika | |
| (n = 100) | (n = 10) | (n = 100) | (n = 100) | (n = 100) | (n = 49) | |
| Female, n (%) | 39 (39) | 68 (68) | 59 (59) | 65 (65) | 72 (72) | 39 (79.6) |
| Age (years) @ | 40.2 ± 15.1 | 56.7 ± 21.3 | 63.1 ± 21.3 | 33.5 ± 13.6 | 45.1 ± 12.1 | 42.1 ± 13.7 |
| Body mass index (kg/m2) @ | 24.4 ± 5.2 | 23.5 ± 7.3 | 22.8 ± 3.3 | 23.5 ± 7.0 | 25.0 ± 4.9 | 26.06 ± 4.96 |
| Comorbidities, n (%) | 26 (26) | 71 (71) | 76 (76) | 29 (29) | 36 (36) | 16 (32.6) |
| Diabetes mellitus | 10 (10) | 31 (31) | 20 (20) | 9 (9) | 13 (13) | 4 (8.2) |
| Hypertension | 9 (9) | 55 (55) | 51 (51) | 13 (13) | 20 (20) | 8 (16.3) |
| Dyslipidemia | 6 (6) | 38 (38) | 20 (20) | 6 (6) | 17 (17) | 7 (14.3) |
| Heart disease | 2 (2) | 33 (33) | 26 (26) | 5 (5) | 2 (2) | 1 (2.0) |
| Lung disease | 2 (2) | 9 (9) | 22 (22) | 5 (5) | 4 (4) | 1 (2.0) |
| Neurologic disease | 3 (3) | 19 (19) | 20 (20) | 5 (5) | 4 (4) | 0 |
| Liver disease | 3 (3) | 7 (7) | 4 (4) | 3 (3) | 1 (1) | 1 (2.0) |
| Kidney disease | 1 (1) | 26 (26) | 25 (25) | 3 (3) | 2 (2) | 0 |
| Cancer | 3 (3) | 14 (14) | 23 (23) | 1 (1) | 4 (4) | 3 (6.1) |
| Setting, n (%) | ||||||
| Outpatient | 0 | 34 (34) | 15 (15) | 41 (41) | 87 (87) | 48 (98) |
| Inpatient | 100 (100) | 66 (66) | 85 (85) | 59 (59) | 13 (13) | 1 (2) |
| Type of Viral Infection | ||||||
|---|---|---|---|---|---|---|
| COVID-19 | Influenza (n = 100) | RSV | Dengue | Chikungunya (n = 100) | Zika | |
| (n = 100) | (n = 100) | (n = 100) | (n = 49) | |||
| Signs and symptoms, n (%) | ||||||
| Fever (≥37.5 °C) | 77 (77) | 83 (83) | 72 (72) | 91 (91) | 63 (63) | 9 (18.4) |
| Rhinorrhea | 23 (23) | 52 (52) | 46 (46) | 7 (7) | 3 (3) | 5 (10.2) |
| Sore throat | 36 (36) | 29 (29) | 14 (14) | 11 (11) | 4 (4) | 8 (16.3) |
| Cough | 62 (62) | 96 (96) | 89 (89) | 9 (9) | 8 (8) | 3 (6.1) |
| Productive sputum | 11 (11) | 72 (72) | 77 (77) | 0 | 2 (2) | 0 |
| Shortness of breath | 20 (20) | 53 (53) | 65 (65) | 2 (2) | 0 | 0 |
| Diarrhea | 9 (9) | 2 (2) | 24 (24) | 13 (13) | 2 (2) | 0 |
| Myalgia | 27 (27) | 30 (30) | 13 (13) | 86 (86) | 71 (71) | 18 (36.7) |
| Arthralgia | 0 | 0 | 0 | 11 (11) | 78 (78) | 1 (2.0) |
| Headache | 16 (16) | 14 (14) | 17 (17) | 53 (53) | 12 (12) | 4 (8.2) |
| Rash | 1 (1) | 1 (1) | 3 (3) | 15 (15) | 65 (65) | 49 (100) |
| Laboratory investigation | ||||||
| Hb (g/dL) @ | 13.9 ± 1.6 | 11.5 ± 2.3 | 10.7 ± 2.2 | 13.4 ± 1.9 | 12.8 ± 1.6 | 13.5 ± 1.3 |
| WBC (cells/mm3) # | 5120 (3915, 6440) | 6640 (4758, 8638) | 8180 (4868, 11,868) | 3355 (2340, 4863) | 4825 (3523, 6215) | 4715 (3673, 5473) |
| Lymphocyte count (cells/mm3) # | 1602 (1232, 2173) | 862 (622, 1256) | 986 (499, 1445) | 630 (421, 916) | 800 (562, 1159) | 1301 (911, 1670) |
| Platelet count (/mm3) # | 216,500 (173,000, 247,500) | 185,500 (147,250, 231,750) | 186,500 (131,000, 271,500) | 112,500 (66,750, 156,750) | 221,000 (170,500, 257,750) | 228,500 (201,750, 288, 750) |
| AST (U/L) # | 22 (18, 31) | 36 (23, 67) | 30 (22, 54) | 82 (48, 199) | 30 (22, 49) | 21 (18, 29) |
| ALT (U/L) # | 24 (16, 37) | 25 (15, 38) | 24 (14, 42) | 56 (30, 134) | 27 (17, 42) | 16 (11, 25) |
| Number (%) | p-Value | |||||
|---|---|---|---|---|---|---|
| COVID-19 (A) (n = 100) | Influenza and RSV (B) (n = 200) | Dengue (C) (n = 100) | A vs. B vs. C | A vs. B | A vs. C | |
| Female, n (%) | 39 (39) | 127 (63.5) | 65 (65) | <0.001 | * | * |
| Age (years) @ | 40.2 ± 15.1 | 59.9 ± 21.5 | 33.5 ± 13.6 | <0.001 | * | * |
| BMI (kg/m2) @ | 24.4 ± 5.2 | 23.1 ± 5.6 | 23.5 ± 7.0 | 0.128 | - | - |
| Comorbidities, n (%) | 26 (26) | 147 (73.5) | 29 (29) | <0.001 | * | NS |
| Diabetes mellitus | 10 (10) | 51 (25.5) | 9 (9) | <0.001 | * | NS |
| Hypertension | 9 (9) | 106 (53.0) | 13 (13) | <0.001 | * | NS |
| Dyslipidemia | 6 (6) | 58 (29.0) | 6 (6) | <0.001 | * | NS |
| Heart disease | 2 (2) | 59 (29.5) | 5 (5) | <0.001 | * | NS |
| Lung disease | 2 (2) | 31 (15.5) | 5 (5) | <0.001 | * | NS |
| Neurologic disease | 3 (3) | 39 (19.5) | 5 (5) | <0.001 | * | NS |
| Liver disease | 3 (3) | 11 (5.5) | 3 (3) | 0.523 | - | - |
| Kidney disease | 1 (1) | 51 (25.5) | 3 (3) | <0.001 | * | NS |
| Cancer | 3 (3) | 37 (18.5) | 1 (1) | <0.001 | * | NS |
| Signs and symptoms, n (%) | ||||||
| Fever (≥37.5 °C) | 77 (77) | 155 (77.5) | 91 (91) | 0.011 | NS | * |
| Baseline temperature @ | 37.3 ± 0.8 | 38.1 ± 0.9 | 38.4 ± 1.0 | <0.001 | * | * |
| O2 sat @ | 98.0 ± 2.2 | 94.7 ± 3.7 | 97.6 ± 1.5 | <0.001 | * | NS |
| Rhinorrhea | 23 (23) | 98 (49.0) | 7 (7) | <0.001 | * | * |
| Sore throat | 36 (36) | 43 (21.5) | 11 (11) | <0.001 | * | * |
| Cough | 62 (62) | 185 (92.5) | 9 (9) | <0.001 | * | * |
| Productive sputum | 11 (11) | 149 (74.5) | 0 | <0.001 | * | * |
| Shortness of breath | 20 (20) | 118 (59) | 2 (2) | <0.001 | * | * |
| Diarrhea | 9 (9) | 26 (13) | 13 (13) | 0.567 | - | - |
| Myalgia | 27 (27) | 43 (21.5) | 86 (86) | <0.001 | NS | * |
| Arthralgia | 0 | 0 | 11 (11) | <0.001 | - | * |
| Headache | 16 (16) | 31 (15.5) | 53 (53) | <0.001 | NS | * |
| Rash | 1 (1) | 4 (2) | 15 (15) | <0.001 | NS | * |
| Number (%) or Median (IQR) | p-Value | |||||
|---|---|---|---|---|---|---|
| Laboratory Investigation | COVID-19 (A) (n = 100) | Influenza and RSV (B) (n = 200) | Dengue (C) (n = 100) | A vs. B vs. C | A vs. B | A vs. C |
| Hb (g/dL) @ | 13.9 ± 1.6 | 11.1 ± 2.3 | 13.4 ± 1.9 | <0.001 | * | NS |
| WBC (cells/mm3) # | 5120 (3915, 6440) | 7410 (4833, 10,048) | 3355 (2340, 4863) | <0.001 | * | * |
| ≥4000, n (%) | 72 (72) | 160/184 (87) | 36 (36) | <0.01 | * | * |
| Lymphocyte count (cells/mm3) # | 1602 (1232, 2173) | 904 (562, 1350) | 630 (421, 916) | <0.001 | * | * |
| ≥1000, n (%) | 89 (89) | 83/184 (45.1) | 20 (20) | <0.01 | * | * |
| Platelet count (/mm3) # | 216,500 (−173,000, 247,500) | 185,500 (−139,250, 245,000) | 112,500 (−66,750, 156,750) | <0.001 | * | * |
| ≥150,000, n (%) | 92 (92) | 129/184 (70.1) | 28 (28) | <0.01 | * | * |
| AST (U/L) # | 22 (18, 31) | 32 (22, 58) | 82 (48, 199) | <0.001 | * | * |
| ≥40, n (%) | 18/99 (18.2) | 34/92 (37.0) | 68/83 (81.9) | <0.01 | * | * |
| ALT (U/L) # | 24 (16, 37) | 24 (15, 39) | 56 (30, 134) | <0.001 | NS | * |
| Risk Factors | b | Adjusted Odds Ratio | 95% CI | p-Value | |
|---|---|---|---|---|---|
| COVID-19 vs. | Age > 50 years old | 1.168 | 3.21 | 1.25–8.29 | 0.016 |
| Influenza/RSV (1) | Underlying disease | 1.425 | 4.16 | 1.62–10.69 | 0.003 |
| Rhinorrhea | 2.403 | 11.06 | 4.08–29.95 | <0.001 | |
| Productive sputum | 3.155 | 23.47 | 9.38–58.70 | <0.001 | |
| Lymphocyte count <1000 cells/mm3 | 1.836 | 6.25 | 2.50–15.72 | <0.001 | |
| COVID-19 vs. | Headache | 1.658 | 5.25 | 1.32–20.87 | 0.019 |
| Dengue (2) | Myalgia | 2.165 | 8.71 | 2.34–32.47 | 0.001 |
| No Cough | 2.478 | 11.92 | 2.61–54.35 | 0.001 | |
| Platelet count <150,000/mm3 | 3.262 | 26.10 | 6.43–105.91 | <0.001 | |
| Lymphocyte count < 1000 cells/mm3 | 3.504 | 33.24 | 8.42–131.24 | <0.001 |
| Risk Factors | b | b/|Smallest b| | Score | |
|---|---|---|---|---|
| COVID-19 vs. | Age > 50 years old | 1.168 | 1 | 1 |
| Influenza/RSV | Underlying disease | 1.425 | 1.22 | 1 |
| Rhinorrhea | 2.403 | 2.06 | 2 | |
| Productive sputum | 3.155 | 2.70 | 3 | |
| Lymphocyte count < 1000 cells/mm3 | 1.836 | 1.57 | 2 | |
| COVID-19 | Headache | 1.658 | 1 | 1 |
| vs. Dengue | Myalgia | 2.165 | 1.31 | 1 |
| No cough | 2.478 | 1.49 | 1 | |
| Platelet count < 150,000/mm3 | 3.262 | 1.97 | 2 | |
| Lymphocyte count < 1000 cells/mm3 | 3.504 | 2.11 | 2 |
| Number (%) | Number (%) | ||||
|---|---|---|---|---|---|
| Score for Influenza | COVID-19 (n = 100) | Influenza (n = 184) | Score for Dengue | COVID-19 (n = 100) | Dengue (n = 100) |
| 0 | 37 (37) | 1 (0.5) | 0 | 36 (36) | 0 (0) |
| 1 | 13 (13) | 2 (1.1) | 1 | 28 (28) | 1 (1) |
| 2 | 25 (25) | 13 (7.1) | 2 | 25 (25) | 1 (1) |
| 3 | 13 (13) | 5 (2.7) | 3 | 5 (5) | 7 (7) |
| 4 | 8 (8) | 18 (9.8) | 4 | 4 (4) | 17 (17) |
| 5 | 3 (3) | 43 (23.4) | 5 | 2 (2) | 24 (24) |
| 6 | 0 | 14 (7.6) | 6 | 0 (0) | 28 (28) |
| 7 | 1 (1) | 54 (29.3) | 7 | 0 (0) | 22 (22) |
| 8 | 0 | 8 (4.3) | |||
| 9 | 0 | 26 (14.1) | |||
| Score for Influenza/RSV: Cutoff Point | Sensitivity (95% CI) | Specificity (95% CI) |
|---|---|---|
| ≥3 | 91.3 (86.3, 95.0) | 75.0 (65.3, 83.1) |
| ≥4 | 88.6 (83.1, 92.8) | 88.0 (80.0, 93.6) |
| ≥5 | 78.8 (72.2, 84.5) | 96.0 (90.1, 98.9) |
| Score for Dengue: Cutoff Point | Sensitivity (95% CI) | Specificity (95% CI) |
| ≥3 | 98.0 (93.0, 99.8) | 89.0 (81.2, 94.4) |
| ≥4 | 91.0 (83.6, 95.8) | 94.0 (87.4, 97.8) |
| ≥5 | 74.0 (64.3, 82.3) | 98.0 (93.0, 99.8) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sirijatuphat, R.; Sirianan, K.; Horthongkham, N.; Komoltri, C.; Angkasekwinai, N. Distinguishing SARS-CoV-2 Infection and Non-SARS-CoV-2 Viral Infections in Adult Patients through Clinical Score Tools. Trop. Med. Infect. Dis. 2023, 8, 61. https://doi.org/10.3390/tropicalmed8010061
Sirijatuphat R, Sirianan K, Horthongkham N, Komoltri C, Angkasekwinai N. Distinguishing SARS-CoV-2 Infection and Non-SARS-CoV-2 Viral Infections in Adult Patients through Clinical Score Tools. Tropical Medicine and Infectious Disease. 2023; 8(1):61. https://doi.org/10.3390/tropicalmed8010061
Chicago/Turabian StyleSirijatuphat, Rujipas, Kulprasut Sirianan, Navin Horthongkham, Chulaluk Komoltri, and Nasikarn Angkasekwinai. 2023. "Distinguishing SARS-CoV-2 Infection and Non-SARS-CoV-2 Viral Infections in Adult Patients through Clinical Score Tools" Tropical Medicine and Infectious Disease 8, no. 1: 61. https://doi.org/10.3390/tropicalmed8010061
APA StyleSirijatuphat, R., Sirianan, K., Horthongkham, N., Komoltri, C., & Angkasekwinai, N. (2023). Distinguishing SARS-CoV-2 Infection and Non-SARS-CoV-2 Viral Infections in Adult Patients through Clinical Score Tools. Tropical Medicine and Infectious Disease, 8(1), 61. https://doi.org/10.3390/tropicalmed8010061






