Riding the Pandemic Waves—Lessons to Be Learned from the COVID-19 Crisis Management in Romania
Abstract
:1. Introduction
- To evaluate the government’s pandemic responses in 2021 regarding excess mortality;
- To ascertain the main experiences and lessons that can be learned from managing the pandemic in Romania.
2. Materials and Methods
3. Results
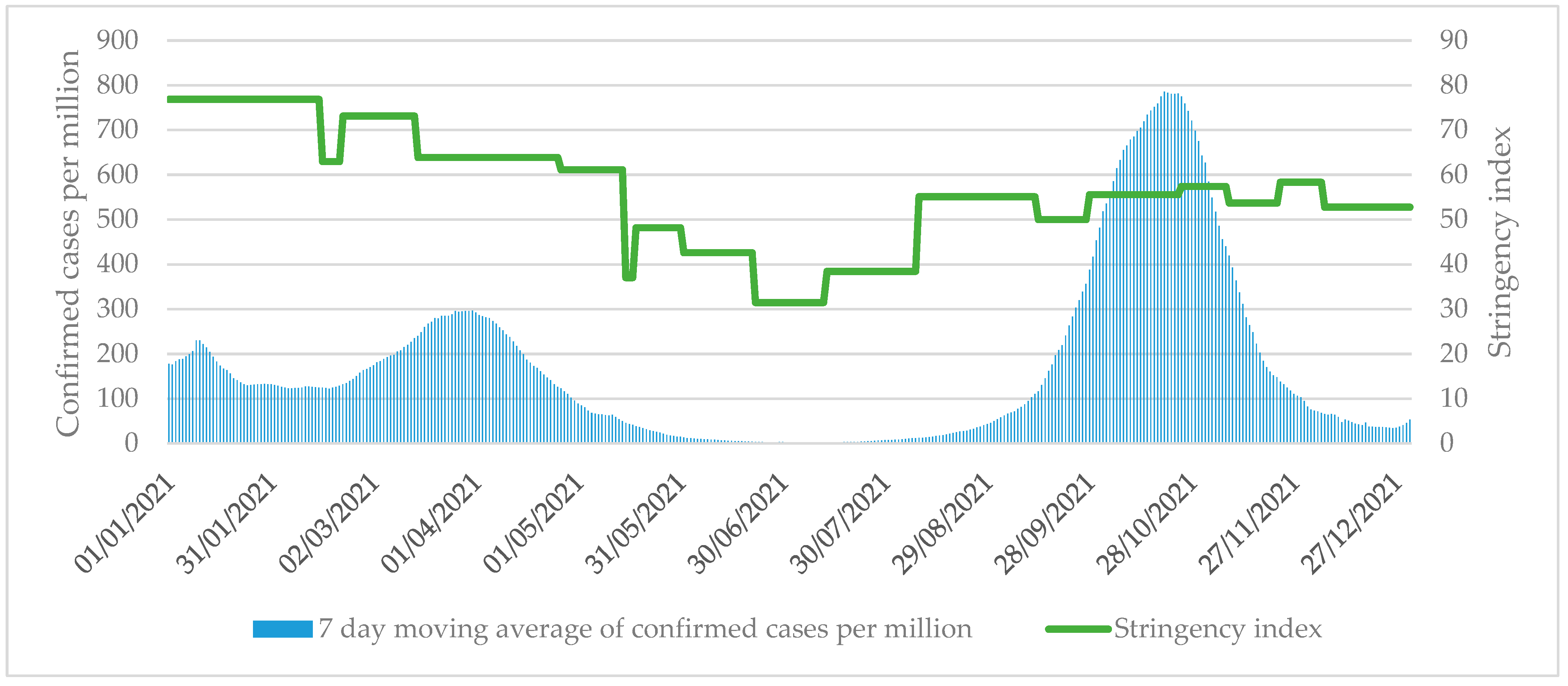
3.1. Preventing Local Transmission
3.2. Ensuring Sufficient Health Workforce Capacity and Infrastructure
3.3. Providing Health Services Effectively
3.4. Governance
3.5. Health Outcomes of Pandemic Management Measures to Slow down the Spread of the Pandemic
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Bank. Romania Country Overview. Available online: https://www.worldbank.org/en/country/romania/overview#1 (accessed on 31 March 2022).
- OECD and European Observatory on Health Systems and Policies. Romania: Country Health Profile 2021. Published Online 2021. Available online: https://www.oecd-ilibrary.org/content/publication/74ad9999-en (accessed on 31 March 2022).
- Dascalu, S. The Successes and Failures of the Initial COVID-19 Pandemic Response in Romania. Front. Public Health 2020, 8, 344. [Google Scholar] [CrossRef] [PubMed]
- Thye, A.Y.K.; Law, J.W.F.; Pusparajah, P.; Letchumanan, V.; Chan, K.G.; Lee, L.H. Emerging SARS-CoV-2 Variants of Concern (VOCs): An Impending Global Crisis. Biomedicines 2021, 9, 1303. [Google Scholar] [CrossRef] [PubMed]
- Nehal, K.R.; Steendam, L.M.; Campos Ponce, M.; van der Hoeven, M.; Smit, G.S.A. Worldwide Vaccination Willingness for COVID-19: A Systematic Review and Meta-Analysis. Vaccines 2021, 9, 1071. [Google Scholar] [CrossRef] [PubMed]
- Tartof, S.Y.; Slezak, J.M.; Fischer, H.; Hong, V.; Ackerson, B.K.; Ranasinghe, O.N.; Frankland, T.B.; Ogun, O.A.; Zamparo, J.M.; Gray, S.; et al. Effectiveness of mRNA BNT162b2 COVID-19 vaccine up to 6 months in a large integrated health system in the USA: A retrospective cohort study. Lancet 2021, 398, 1407–1416. [Google Scholar] [CrossRef]
- Vladescu, C.; Scintee, S.G.; Olsavszky, V.; Hernandez-Quevedo, C.; Sagan, A. Romania: Health System Review. Health Syst. Transit. 2016, 18, 1–170. [Google Scholar]
- Romania Insider. Worrying Statistics: Over 300 Communes in Romania Have No Family Doctors. Available online: https://www.romania-insider.com/romania-communes-family-doctors (accessed on 31 March 2022).
- Ziarul Financiar. Criză de medici de urgenţă în spitale. La Concursuri Nu Vine Niciun Candidat. Available online: https://www.zf.ro/profesii/criza-de-medici-de-urgenta-in-spitale-la-concursuri-nu-vine-niciun-candidat-16989265 (accessed on 31 March 2022).
- Kuhlmann, E.; Brînzac, M.G.; Burau, V.; Correia, T.; Ungureanu, M.I. Health workforce protection and preparedness during the COVID-19 pandemic: A tool for the rapid assessment of EU health systems. Eur. J. Public Health 2021, 31 (Suppl. 4), iv14–iv20. [Google Scholar] [CrossRef]
- WHO. Public Health Criteria to Adjust Public health and Social Measures in the Context of COVID-19 Annex to Considerations in Adjusting Public Health and Social Measures in the Context of COVID-19 12 May 2020. Available online: https://apps.who.int/iris/handle/10665/332073 (accessed on 31 March 2022).
- Merianos, A.; Peiris, M. International health regulations (2005). Lancet 2005, 366, 1249–1251. [Google Scholar] [CrossRef]
- WHO. Joint External Evaluation Tool: International Health Regulations (2005), 2nd ed.; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Bosa, I.; Castelli, A.; Castelli, M.; Ciani, O.; Compagni, A.; Galizzi, M.M.; Garofano, M.; Ghislandi, S.; Giannoni, M.; Marini, G.; et al. Response to COVID-19: Was Italy (un)prepared? Health Econ. Policy Law 2022, 17, 1–13. [Google Scholar] [CrossRef]
- WHO. COVID-19 Strategic Preparedness and Response: Monitoring and Evaluation Framework. Published Online 2020. Available online: https://www.who.int/publications/i/item/monitoring-and-evaluation-framework (accessed on 31 March 2022).
- Mustafa, S.; Zhang, Y.; Zibwowa, Z.; Seifeldin, R.; Ako-Egbe, L.; McDarby, G.; Kelley, E.; Saikat, S. COVID-19 Preparedness and Response Plans from 106 countries: A review from a health systems resilience perspective. Health Policy Plan. 2022, 37, 255–268. [Google Scholar] [CrossRef]
- European Observatory on Health Systems and Policies. COVID-19 Health System Response Monitor (HSRM). Available online: https://eurohealthobservatory.who.int/monitors/hsrm/overview (accessed on 31 March 2022).
- Alexander, M.; Unruh, L.; Koval, A.; Belanger, W. United States response to the COVID-19 pandemic, January-November 2020. Health Econ. Policy Law 2022, 17, 62–75. [Google Scholar] [CrossRef]
- Sagan, A.; Bryndova, L.; Kowalska-Bobko, I.; Smatana, M.; Spranger, A.; Szerencses, V.; Webb, E.; Gaal, P. A reversal of fortune: Comparison of health system responses to COVID-19 in the Visegrad group during the early phases of the pandemic. Health Policy 2021, 126, 446–455. [Google Scholar] [CrossRef] [PubMed]
- Webb, E.; Winkelmann, J.; Scarpetti, G.; Behmane, D.; Habicht, T.; Kahur, K.; Kasekamp, K.; Köhler, K.; Miščikienė, L.; Misins, J.; et al. Lessons learned from the Baltic countries’ response to the first wave of COVID-19. Health Policy 2021, 126, 438–445. [Google Scholar] [CrossRef] [PubMed]
- Kisa, S.; Kisa, A. Under-reporting of COVID-19 cases in Turkey. Int. J. Health Plan. Manag. 2020, 35, 1009–1013. [Google Scholar] [CrossRef] [PubMed]
- Molla, M.M.A.; Disha, J.A.; Yeasmin, M.; Ghosh, A.K.; Nafisa, T. Decreasing transmission and initiation of countrywide vaccination: Key challenges for future management of COVID-19 pandemic in Bangladesh. Int. J. Health Plan. Manag. 2021, 36, 1014–1029. [Google Scholar] [CrossRef] [PubMed]
- Okereke, M.; Ukor, N.A.; Adebisi, Y.A.; Ogunkola, I.O.; Iyagbaye, E.F.; Owhor, G.A.; Iii, D.E.L. Impact of COVID-19 on access to healthcare in low- and middle-income countries: Current evidence and future recommendations. Int. J. Health Plan. Manag. 2021, 36, 13–17. [Google Scholar] [CrossRef] [PubMed]
- Choi, E.M. COVID-19 vaccines for low- and middle-income countries. Trans. R. Soc. Trop. Med. Hyg. 2021, 115, 447–456. [Google Scholar] [CrossRef]
- Van Nguyen, H.; Van Hoang, M.; Dao, A.T.M.; Nguyen, H.L.; Nguyen, T.V.; Nguyen, P.T.; Khuong, L.Q.; Le, P.M.; Gilmour, S. An adaptive model of health system organization and responses helped Vietnam to successfully halt the COVID-19 pandemic: What lessons can be learned from a resource-constrained country. Int. J. Health Plan. Manag. 2020, 35, 988–992. [Google Scholar] [CrossRef]
- Impouma, B.; Williams, G.S.; Moussana, F.; Mboussou, F.; Farham, B.; Wolfe, C.M.; Okot, C.; Downing, K.; Tores, C.C.; Flahault, A.; et al. The first 8 months of COVID-19 pandemic in three West African countries: Leveraging lessons learned from responses to the 2014–2016 Ebola virus disease outbreak. Epidemiol. Infect. 2021, 149, 1–22. [Google Scholar] [CrossRef]
- University of Oxford. Our World in Data Database. Available online: https://ourworldindata.org/coronavirus (accessed on 31 March 2022).
- European Centre for Disease Prevention and Control. COVID-19 datasets. Available online: https://www.ecdc.europa.eu/en/covid-19/data (accessed on 31 March 2022).
- Eurostat. Eurostat database. Available online: https://ec.europa.eu/eurostat/data/database (accessed on 31 March 2022).
- Peters, M.D.J.; Godfrey, C.; McInerney, P.; Munn, Z.; Tricco, A.C.; Khalil, H. Chapter 11: Scoping Reviews (2020 version). In JBI Manual for Evidence Synthesis, JBI; Aromataris, E., Munn, Z., Eds.; Joanna Briggs Institute: Adelaide, Australia, 2020; Available online: https://synthesismanual.jbi.global (accessed on 31 March 2022).
- Dascalu, S.; Geambasu, O.; Valentin Raiu, C.; Azoicai, D.; Damian Popovici, E.; Apetrei, C. COVID-19 in Romania: What Went Wrong? Front. Public Health 2021, 9, 3941. [Google Scholar] [CrossRef]
- Ministerul Afacerilor Interne. HOTĂRÂRE nr. 52 din 05.11.2020 Privind Stabilirea Unor Măsuri Suplimentare Necesar a fi Aplicate Pentru Prevenirea și Combaterea Efectelor Pandemiei de COVID-19. Available online: https://www.mai.gov.ro/wp-content/uploads/2019/01/Hotarare-CNSU-52-din-05.11.2020-v19.pdf (accessed on 31 March 2022).
- Commission, E.; Centre, J.R.; Velicu, A. The School Year 2020–2021 in Romania during the Pandemic: Country Report. Published Online 2021. Available online: https://op.europa.eu/en/publication-detail/-/publication/084dd1be-da18-11eb-895a-01aa75ed71a1 (accessed on 31 March 2022).
- Digi24.ro. Klaus Iohannis: Circulația Pe Timp De Noapte Va Fi Restricționată Mai Devreme. Nu Avem în Vedere Un lockdown De Paște. Available online: https://www.digi24.ro/stiri/actualitate/politica/klaus-iohannis-circulatia-pe-timp-de-noapte-va-fi-restrictionata-mai-devreme-nu-avem-in-vedere-un-lockdown-de-paste-1465087 (accessed on 31 March 2022).
- Garda.com. Romania: Authorities to Ease COVID-19-Related Domestic Restrictions from May 15/update 19. Available online: https://crisis24.garda.com/alerts/2021/05/romania-authorities-to-ease-covid-19-related-domestic-restrictions-from-may-15-update-19 (accessed on 31 March 2022).
- Garda.com. Romania: Authorities Ease COVID-19-Related Domestic Restrictions June 1; International Entry Measures Unchanged. Available online: https://crisis24.garda.com/alerts/2021/06/romania-authorities-ease-covid-19-related-domestic-restrictions-june-1-international-entry-measures-unchanged-update-20 (accessed on 31 March 2022).
- Garda.com. Romania: Authorities Extend COVID-19-Related State of Alert until Aug. 10. Available online: https://crisis24.garda.com/alerts/2021/07/romania-authorities-extend-covid-19-related-state-of-alert-until-aug-10-update-22 (accessed on 31 March 2022).
- Garda.com. Authorities to Tighten Domestic COVID-19 Restrictions for at Least 30 days Effective Oct. 25. Available online: https://crisis24.garda.com/alerts/2021/10/romania-authorities-to-tighten-domestic-covid-19-restrictions-for-at-least-30-days-effective-oct-25-update-26 (accessed on 31 March 2022).
- Lorenzovici, L.; Bârzan-Székely, A.; Kaló, Z.; Sz, F.R.; Nagy Gy, A.; Nyulas, A.B.; Precup, A.M.; Pavel, M.; Gheorghe, M.; Calcan, A.; et al. Epidemiology, Hospitalization Cost, and Socioeconomic Burden of COVID-19 in Romania. Published Online 2022. Available online: https://www.researchgate.net/publication/358753042_Epidemiology_hospitalization_cost_and_socioeconomic_burden_of_COVID-19_in_Romania (accessed on 31 March 2022).
- Grubaugh, N.D.; Hodcroft, E.B.; Fauver, J.R.; Phelan, A.L.; Cevik, M. Public health actions to control new SARS-CoV-2 variants. Cell 2021, 184, 1127–1132. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. Guidance for Representative and Targeted Genomic SARS-CoV-2 Monitoring. Published Online 2021. Available online: https://www.ecdc.europa.eu/sites/default/files/documents/Guidance-for-representative-and-targeted-genomic-SARS-CoV-2-monitoring-updated-with%20erratum-20-May-2021.pdf (accessed on 31 March 2022).
- Politico. Romania Suspends Surgeries, Asks EU for Help as It Battles Coronavirus Wave. Available online: https://www.politico.eu/article/romania-surgeries-eu-coronavirus-help/ (accessed on 31 March 2022).
- The Council of the European Union. Council regulation (EU) 2020/521 of 14 April 2020 Activating the Emergency Support under Regulation (EU) 2016/369, and Amending Its Provisions Taking into Account the COVID-19 Outbreak. Off. J. Eur. Union. Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/HTML/?uri=CELEX:32020R0521&from=EN (accessed on 31 March 2022).
- European Centre for Disease Prevention and Control. Overview of the Implementation of COVID-19 Vaccination Strategies and Deployment Plans in the EU/EEA. Published Online 2021. Available online: https://www.ecdc.europa.eu/en/publications-data/overview-implementation-covid-19-vaccination-strategies-and-deployment-plans (accessed on 31 March 2022).
- Europen Commission. EU Continues to Support Romania Tackle the Increase of COVID-19 Caseseu Continues to Support Romania Tackle the Increase of COVID-19 Cases. Available online: https://ec.europa.eu/echo/news-stories/news/eu-continues-support-romania-tackle-increase-covid-19-cases-2021-10-21_en (accessed on 31 March 2022).
- Lorenzovici, L.; Székely, A.; Farkas, R.S.; Sófalvi, A. The Impact of COVID-19 Pandemic on Romanian Hospital Services. Published Online 2021. Available online: https://www.researchgate.net/publication/346006458_The_impact_of_Covid-19_pandemic_on_Romanian_hospital_services (accessed on 31 March 2022).
- Dascalu, S. Measles Epidemics in Romania: Lessons for Public Health and Future Policy. Front. Public Health 2019, 7, 98. [Google Scholar] [CrossRef] [PubMed]
- Marcec, R.; Majta, M.; Likic, R. Will vaccination refusal prolong the war on SARS-CoV-2? Postgrad. Med. J. 2021, 97, 143–149. [Google Scholar] [CrossRef] [PubMed]
- Dascalu, S.; Flammer, P.G.; Ghafari, M.; Henson, S.C.; Nascimento, R.; Bonsall, M.B. Engaging Religious Institutions and Faith-Based Communities in Public Health Initiatives: A Case Study of the Romanian Orthodox Church During the COVID-19 Pandemic. Front. Public Health 2021, 9, 8091. [Google Scholar] [CrossRef] [PubMed]
- Manolescu, L.S.C.; Zaharia, C.N.; Dumitrescu, A.I.; Prasacu, I.; Radu, M.C.; Boeru, A.C.; Boidache, L.; Nita, I.; Necsulescu, A.; Chivu, R.D. Early COVID-19 Vaccination of Romanian Medical and Social Personnel. Vaccines 2021, 9, 1127. [Google Scholar] [CrossRef] [PubMed]
- Maftei, A.; Holman, A.C. SARS-CoV-2 Threat Perception and Willingness to Vaccinate: The Mediating Role of Conspiracy Beliefs. Front. Psychol. 2021, 12, 672634. [Google Scholar] [CrossRef] [PubMed]
- Euobserver. COVID-Pass Protestors Try to Storm Romanian Parliament. Available online: https://euobserver.com/coronavirus/153888. (accessed on 31 March 2022).
- Stoica, C.A.; Umbreș, R. Suspicious minds in times of crisis: Determinants of Romanians’ beliefs in COVID-19 conspiracy theories. Null 2021, 23, S246–S261. [Google Scholar] [CrossRef]
- Ratchev, V.; Tagarev, T.; Minchev, Z. Romania: Capabilities, Organisations, Policies, and Legislation in Crisis Management and Disaster Response; Institute of Information and Communication Technologies: Bucharest, Romania, 2015. [Google Scholar]
- Andrei Chirileasa. What’s the Real Incidence Rate of COVID-19 Cases in Romania and Which Are the Most Affected Regions? Romania Insider. Available online: https://www.romania-insider.com/covid-19-incidence-rates-romania-october-6-2020 (accessed on 31 March 2022).
- Euractive.ro. Romanian Government Changes COVID-19 Rules as Incidence Rate Surpasses Threshold. Available online: https://www.euractiv.com/section/politics/short_news/romanian-government-changes-covid-19-rules-as-incidence-rate-surpasses-threshold/ (accessed on 31 March 2022).
- Politico. Romania—2020 General Election. Available online: https://www.politico.eu/europe-poll-of-polls/romania/ (accessed on 31 March 2022).
- OECD. Quarterly GDP (Indicator). Available online: https://data.oecd.org/gdp/quarterly-gdp.htm (accessed on 31 March 2022).
- European Digital Media Observatory. COVID-19 Vaccination in Bulgaria and Romania: Too Easy to Blame it on “Fake News”. Available online: https://edmo.eu/2021/10/18/covid-19-vaccination-in-bulgaria-and-romania-too-easy-to-blame-it-on-fake-news/ (accessed on 31 March 2022).
- Gozzi, N.; Bajardi, P.; Perra, N. The importance of non-pharmaceutical interventions during the COVID-19 vaccine rollout. PLoS Comput. Biol. 2021, 17, e1009346. [Google Scholar] [CrossRef]
- Sonabend, R.; Whittles, L.K.; Imai, N.; Perez-Guzman, P.N.; Knock, E.S.; Rawson, T.; Gaythorpe, K.A.M.; A Djaafara, B.; Hinsley, W.; FitzJohn, R.G.; et al. Non-pharmaceutical interventions, vaccination, and the SARS-CoV-2 delta variant in England: A mathematical modelling study. Lancet 2021, 398, 1825–1835. [Google Scholar] [CrossRef]
- MacIntyre, C.R.; Costantino, V.; Trent, M. Modelling of COVID-19 vaccination strategies and herd immunity, in scenarios of limited and full vaccine supply in NSW, Australia. Vaccine 2022, 40, 2506–2513. [Google Scholar] [CrossRef]
- Liu, Y.; Rocklöv, J. The reproductive number of the Delta variant of SARS-CoV-2 is far higher compared to the ancestral SARS-CoV-2 virus. J. Travel Med. 2021, 28, 12. [Google Scholar] [CrossRef]
- Fiolet, T.; Kherabi, Y.; MacDonald, C.J.; Ghosn, J.; Peiffer-Smadja, N. Comparing COVID-19 vaccines for their characteristics, efficacy and effectiveness against SARS-CoV-2 and variants of concern: A narrative review. Clin. Microbiol. Infect. 2022, 28, 202–221. [Google Scholar] [CrossRef] [PubMed]
- Minh, L.H.N.; Khoi Quan, N.; Le, T.N.; Khanh, P.N.Q.; Huy, N.T. COVID-19 Timeline of Vietnam: Important Milestones Through Four Waves of the Pandemic and Lesson Learned. Front. Public Health 2021, 9, 9067. [Google Scholar] [CrossRef] [PubMed]
- Chiyaka, E.T.; Chingarande, G.; Dzinamarira, T.; Murewanhema, G.; Madziva, R.; Herrera, H.; Musuka, G. Prevention and Control of Infectious Diseases: Lessons from COVID-19 Pandemic Response in Zimbabwe. COVID 2022, 2, 642–648. [Google Scholar] [CrossRef]
- Túri, G.; Virág, A. Experiences and Lessons Learned from COVID-19 Pandemic Management in South Korea and the V4 Countries. Trop. Med. Infect. Dis. 2021, 6, 201. [Google Scholar] [CrossRef] [PubMed]
- Park, H.; Sim, B.; Zhao, B.; Nam, E.W. Public Health Financing and Responses to COVID-19: Lessons from South Korea. Healthcare 2022, 10, 750. [Google Scholar] [CrossRef]
- Feng, J.; Li, J.; Hu, W.; Li, G. Public Interest, Risk, Trust, and Personal Protective Equipment Purchase and Usage: Face Masks Amid the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 5502. [Google Scholar] [CrossRef]
- Østebø, M.T.; Østebø, T.; Tronvoll, K. Health and politics in pandemic times: COVID-19 responses in Ethiopia. Health Policy Plan. 2021, 36, 1681–1689. [Google Scholar] [CrossRef]
- Badman, R.P.; Wang, A.X.; Skrodzki, M.; Cho, H.-C.; Aguilar-Lleyda, D.; Shiono, N.; Yoo, S.B.M.; Chiang, Y.-S.; Akaishi, R. Trust in Institutions, Not in Political Leaders, Determines Compliance in COVID-19 Prevention Measures within Societies across the Globe. Behav. Sci. 2022, 12, 170. [Google Scholar] [CrossRef]
- Vermeşan, D.; Todor, A.; Andrei, D.; Niculescu, M.; Tudorache, E.; Haragus, H. Effect of COVID-19 Pandemic on Orthopedic Surgery in Three Centers from Romania. Int. J. Environ. Res. Public Health 2021, 18, 2196. [Google Scholar] [CrossRef]
- Pinte, L.; Caraiola, S.; Balaban, D.V.; Badea, C.; Mazilu, D.; Ionescu, G.D.; Iosub, M.-I.; Bălan, E.-S.; Negoi, F.; Dumitrescu, B.; et al. COVID-19 Impact and Vaccination Willingness among Romanian Patients with Autoimmune/Immune-Mediated Diseases. Healthcare 2021, 9, 1707. [Google Scholar] [CrossRef]
- Bogos, K.; Kiss, Z.; Fronius, A.K.; Temesi, G.; Elek, J.; Madurka, I.; Cselkó, Z.; Csányi, P.; Abonyi-Tóth, Z.; Rokszin, G.; et al. Different Trends in Excess Mortality in a Central European Country Compared to Main European Regions in the Year of the COVID-19 Pandemic (2020): A Hungarian Analysis. Pathol. Oncol. Res. 2021, 27, 9774. [Google Scholar] [CrossRef] [PubMed]


| Indicator | Sources |
|---|---|
| Confirmed COVID-19 cases per million | University of Oxford |
| Weekly test positivity rate | European Centre for Disease Control and Prevention |
| Stringency index | University of Oxford |
| Practicing medical doctors, medical graduates, and available hospital beds per hundred thousand inhabitants | European Centre for Disease Control and Prevention |
| Number of COVID-19 patients in ICU per million | University of Oxford |
| Number of fully vaccinated people per hundred | University of Oxford |
| Share of fully vaccinated people by age groups | European Centre for Disease Control and Prevention |
| Weekly number of confirmed COVID-19 death per million | University of Oxford |
| Weekly excess death per million | Our World in Data |
| Date | Measures | Sources |
|---|---|---|
| In force on 1 January 2021 | Mandatory mask wearing in indoor and outdoor public spaces, stay-at home requirement between 23:00 and 05:00, school closure, closure of markets in closed spaces, restaurants and cafes could operate at reduced capacity and opening hours, restrictions on private gatherings, mandatory remote working where possible. | [32] |
| 8 February 2021 | Opening of kindergartens and primary schools, partial opening of secondary schools based on epidemic situation | [33] |
| 8 March 2021 | Stay-at home restrictions between 22:00 and 05:00, restaurants and cafes operate at reduced opening hours | [34] |
| 2 April 2021 | Extended holiday in schools until 4 May 2021 to reduce mobility | [33] |
| 15 May 2021 | Removal of stay-at home requirements, release mandatory mask wearing on outdoor spaces, partial release ban on mass gatherings, reopen cultural centers | [35] |
| 1 June 2021 | Lifting restrictions on the attendance of vaccinated people at concerts, weddings, cultural and religious events; reopen gyms and sport centres, mass gatherings up to 1000 people are permitted | [36] |
| 10 August 2021 | Gatherings up to 10 people are permitted, mandatory mask wearing in crowded spaces, social distancing and capacity restrictions for busnisses | [37] |
| 25 October 2021 | Stay-at home restrictions between 22:00 and 05:00 except for vaccinated and recently recovered; health passes and reduced opening hours for busnisses and restaurants | [38] |
| Romania | EU 27 Countries (Average) | |
|---|---|---|
| Practising medical doctors | 318.6 | 390.5 |
| Medical graduates | 25.6 | 14.3 |
| Hospital beds | 705.7 | 531.9 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Túri, G.; Kassay, J.; Virág, A.; Dózsa, C.; Horváth, K.; Lorenzovici, L. Riding the Pandemic Waves—Lessons to Be Learned from the COVID-19 Crisis Management in Romania. Trop. Med. Infect. Dis. 2022, 7, 122. https://doi.org/10.3390/tropicalmed7070122
Túri G, Kassay J, Virág A, Dózsa C, Horváth K, Lorenzovici L. Riding the Pandemic Waves—Lessons to Be Learned from the COVID-19 Crisis Management in Romania. Tropical Medicine and Infectious Disease. 2022; 7(7):122. https://doi.org/10.3390/tropicalmed7070122
Chicago/Turabian StyleTúri, Gergő, János Kassay, Attila Virág, Csaba Dózsa, Krisztián Horváth, and László Lorenzovici. 2022. "Riding the Pandemic Waves—Lessons to Be Learned from the COVID-19 Crisis Management in Romania" Tropical Medicine and Infectious Disease 7, no. 7: 122. https://doi.org/10.3390/tropicalmed7070122
APA StyleTúri, G., Kassay, J., Virág, A., Dózsa, C., Horváth, K., & Lorenzovici, L. (2022). Riding the Pandemic Waves—Lessons to Be Learned from the COVID-19 Crisis Management in Romania. Tropical Medicine and Infectious Disease, 7(7), 122. https://doi.org/10.3390/tropicalmed7070122






