Continuous Circulation of Chikungunya Virus during COVID-19 Pandemic in Jambi, Sumatra, Indonesia
Abstract
1. Introduction
2. Detailed Case Description
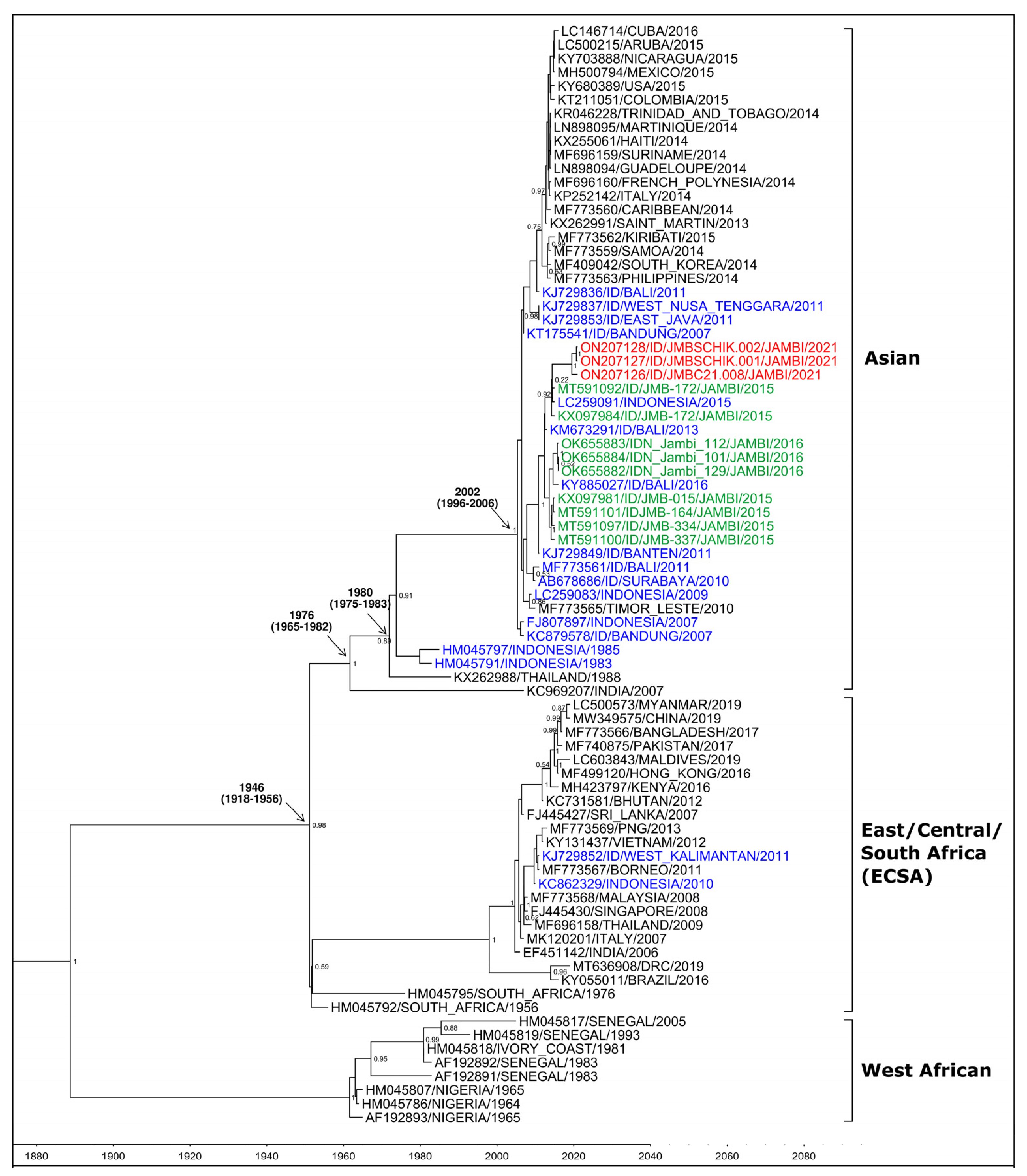
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Guidelines on Clinical Management of Chikungunya Fever; Regional Office for South-East Asia: New Delhi, India, 2008. [Google Scholar]
- Parola, P.; de Lamballerie, X.; Jourdan, J.; Rovery, C.; Vaillant, V.; Minodier, P.; Brouqui, P.; Flahault, A.; Raoult, D.; Charrel, R.N. Novel chikungunya virus variant in travelers returning from Indian Ocean islands. Emerg. Infect. Dis. 2006, 12, 1493–1499. [Google Scholar] [CrossRef] [PubMed]
- Ng, L.-C.; Tan, L.-K.; Tan, C.-H.; Tan, S.S.; Hapuarachchi, H.C.; Pok, K.-Y.; Lai, Y.-L.; Lam-Phua, S.-G.; Bucht, G.; Lin, R.T.; et al. Entomologic and virologic investigation of Chikungnya, Singapore. Emerg. Infect. Dis. 2009, 15, 1243–1249. [Google Scholar] [CrossRef] [PubMed]
- Harapan, H.; Michie, A.; Ernst, T.; Panta, K.; Mudatsir, M.; Yohan, B.; Haryanto, S.; McCarthy, S.; Sasmono, R.T.; Imrie, A. Co-Circulation of Chikungunya and Multiple DENV Serotypes and Genotypes, Western Indonesia 2015–2016. Viruses 2022, 14, 99. [Google Scholar] [CrossRef] [PubMed]
- Laras, K.; Sukri, N.C.; Larasati, R.P.; Bangs, M.J.; Kosim, R.; Djauzi; Wandra, T.; Master, J.; Kosasih, H.; Hartati, S.; et al. Tracking the re-emergence of epidemic chikungunya virus in Indonesia. Trans. R. Soc. Trop. Med. Hyg. 2005, 99, 128–141. [Google Scholar] [CrossRef] [PubMed]
- Yoshikawa, M.J.; Kusriastuti, R. Surge of dengue virus infection and chikungunya Fever in bali in 2010: The burden of mosquito-borne infectious diseases in a tourist destination. Trop. Med. Health 2013, 41, 67–78. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ministry of Health of the Republic of Indonesia. Indonesia Health Profile 2020; Ministry of Health of the Republic of Indonesia: Jakarta, Indonesia, 2021. [Google Scholar]
- Satuan Tugas Penanganan COVID-19: Peta Sebaran 2021. Available online: https://covid19.go.id/peta-sebaran (accessed on 13 April 2022).
- Kumar, S.; Stecher, G.; Li, M.; Knyaz, C.; Tamura, K. MEGA X: Molecular Evolutionary Genetics Analysis across Computing Platforms. Mol. Biol. Evol. 2018, 35, 1547–1549. [Google Scholar] [CrossRef] [PubMed]
- Bouckaert, R.; Vaughan, T.G.; Barido-Sottani, J.; Duchêne, S.; Fourment, M.; Gavryushkina, A.; Heled, J.; Jones, G.; Kühnert, D.; De Maio, N.; et al. BEAST 2.5: An advanced software platform for Bayesian evolutionary analysis. PLoS Comput. Biol. 2019, 15, e1006650. [Google Scholar] [CrossRef] [PubMed]
- Volk, S.M.; Chen, R.; Tsetsarkin, K.A.; Adams, A.P.; Garcia, T.I.; Sall, A.A.; Nasar, F.; Schuh, A.J.; Holmes, E.C.; Higgs, S.; et al. Genome-scale phylogenetic analyses of chikungunya virus reveal independent emergences of recent epidemics and various evolutionary rates. J. Virol. 2010, 84, 6497–6504. [Google Scholar] [CrossRef] [PubMed]
- Sasmono, R.T.; Ma’Roef, C.N.; Haryanto, S.; Myint, K.S.A.; Yohan, B.; Hayati, R.F.; Ledermann, J.P.; Yudhaputri, F.A.; Perkasa, A.; Powers, A.M. Chikungunya Detection during Dengue Outbreak in Sumatra, Indonesia: Clinical Manifestations and Virological Profile. Am. J. Trop. Med. Hyg. 2017, 97, 1393–1398. [Google Scholar] [CrossRef] [PubMed]
- Stubbs, S.C.B.; Johar, E.; Yudhaputri, F.A.; Yohan, B.; Santoso, M.S.; Hayati, R.F.; Denis, D.; Blacklaws, B.A.; Powers, A.M.; Sasmono, R.T.; et al. An Investig-Ation into the Epidemiology of Chikungunya Virus across Neglected Regions of Indonesia. PLoS Negl. Trop. Dis. 2020, 14, e0008934. [Google Scholar] [CrossRef] [PubMed]
- Anggraeni, Y.M.; Garjito, T.A.; Prihatin, M.T.; Handayani, S.W.; Negari, K.S.; Yanti, A.O.; Hidajat, M.C.; Prastowo, D.; Satoto, T.B.T.; Manguin, S.; et al. Fast Expansion of the Asian-Pacific Genotype of the Chikungunya Virus in Indonesia. Front. Cell Infect. Microbiol. 2021, 11, 631508. [Google Scholar] [CrossRef] [PubMed]
- Tarazona-Castro, Y.; Troyes-Rivera, L.; Martins-Luna, J.; Cabellos-Altamirano, F.; Aguilar-Luis, M.A.; Carrillo-Ng, H.; del Valle, L.J.; Kym, S.; Miranda-Maravi, S.; Silva-Caso, W.; et al. Detection of SARS-CoV-2 antibodies in febrile patients from an endemic region of dengue and chikungunya in Peru. PLoS ONE 2022, 17, e0265820. [Google Scholar] [CrossRef]
- Nunez-Avellaneda, D.; Villagómez, F.R.; Villegas-Pineda, J.C.; Barrios-Palacios, J.; Salazar, M.I.; Machain-Williams, C.; Blitvich, B.J. Evidence of Coinfections between SARS-CoV-2 and Select Arboviruses in Guerrero, Mexico, 2020–2021. Am. J. Trop. Med. Hyg. 2022, 106, 896–899. [Google Scholar] [CrossRef] [PubMed]
| Categories | Cases, N = 65 n (%) |
|---|---|
| Symptoms | |
| History of Chikungunya | 0 (0.0) |
| History of travel out of the city | 1 (1.5) |
| Fever | 3 (4.6) |
| Headache | 7 (10.8) |
| Myalgia | 6 (9.2) |
| Arthralgia | 9 (13.9) |
| Joint swelling | 2 (3.1) |
| Fatigue | 4 (6.2) |
| Rash | 2 (3.1) |
| Chikungunya Laboratory Results | |
| RT-PCR-positive | 1 (1.5) * |
| ELISA IgG-positive | 6 (9.2) |
| ELISA IgM-positive | 7 (10.8) |
| Dengue Laboratory Results | |
| RDT NS1-positive | 0 (0.0) |
| RDT IgG-positive | 3 (4.6) |
| RDT IgM-positive | 0 (0.0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Santoso, M.S.; Haryanto, S.; Rulian, F.; Hayati, R.F.; Kristiani, A.; Kartika, R.; Yohan, B.; Hibberd, M.L.; Sasmono, R.T. Continuous Circulation of Chikungunya Virus during COVID-19 Pandemic in Jambi, Sumatra, Indonesia. Trop. Med. Infect. Dis. 2022, 7, 91. https://doi.org/10.3390/tropicalmed7060091
Santoso MS, Haryanto S, Rulian F, Hayati RF, Kristiani A, Kartika R, Yohan B, Hibberd ML, Sasmono RT. Continuous Circulation of Chikungunya Virus during COVID-19 Pandemic in Jambi, Sumatra, Indonesia. Tropical Medicine and Infectious Disease. 2022; 7(6):91. https://doi.org/10.3390/tropicalmed7060091
Chicago/Turabian StyleSantoso, Marsha Sinditia, Sotianingsih Haryanto, Fadil Rulian, Rahma F. Hayati, Amanda Kristiani, Rini Kartika, Benediktus Yohan, Martin L. Hibberd, and R. Tedjo Sasmono. 2022. "Continuous Circulation of Chikungunya Virus during COVID-19 Pandemic in Jambi, Sumatra, Indonesia" Tropical Medicine and Infectious Disease 7, no. 6: 91. https://doi.org/10.3390/tropicalmed7060091
APA StyleSantoso, M. S., Haryanto, S., Rulian, F., Hayati, R. F., Kristiani, A., Kartika, R., Yohan, B., Hibberd, M. L., & Sasmono, R. T. (2022). Continuous Circulation of Chikungunya Virus during COVID-19 Pandemic in Jambi, Sumatra, Indonesia. Tropical Medicine and Infectious Disease, 7(6), 91. https://doi.org/10.3390/tropicalmed7060091







