Rickettsiosis in Southeast Asia: Summary for International Travellers during the COVID-19 Pandemic
Abstract
1. Introduction
2. Spotted Fever Group Rickettsiosis (SFGR)
3. Murine Typhus
4. Scrub Typhus
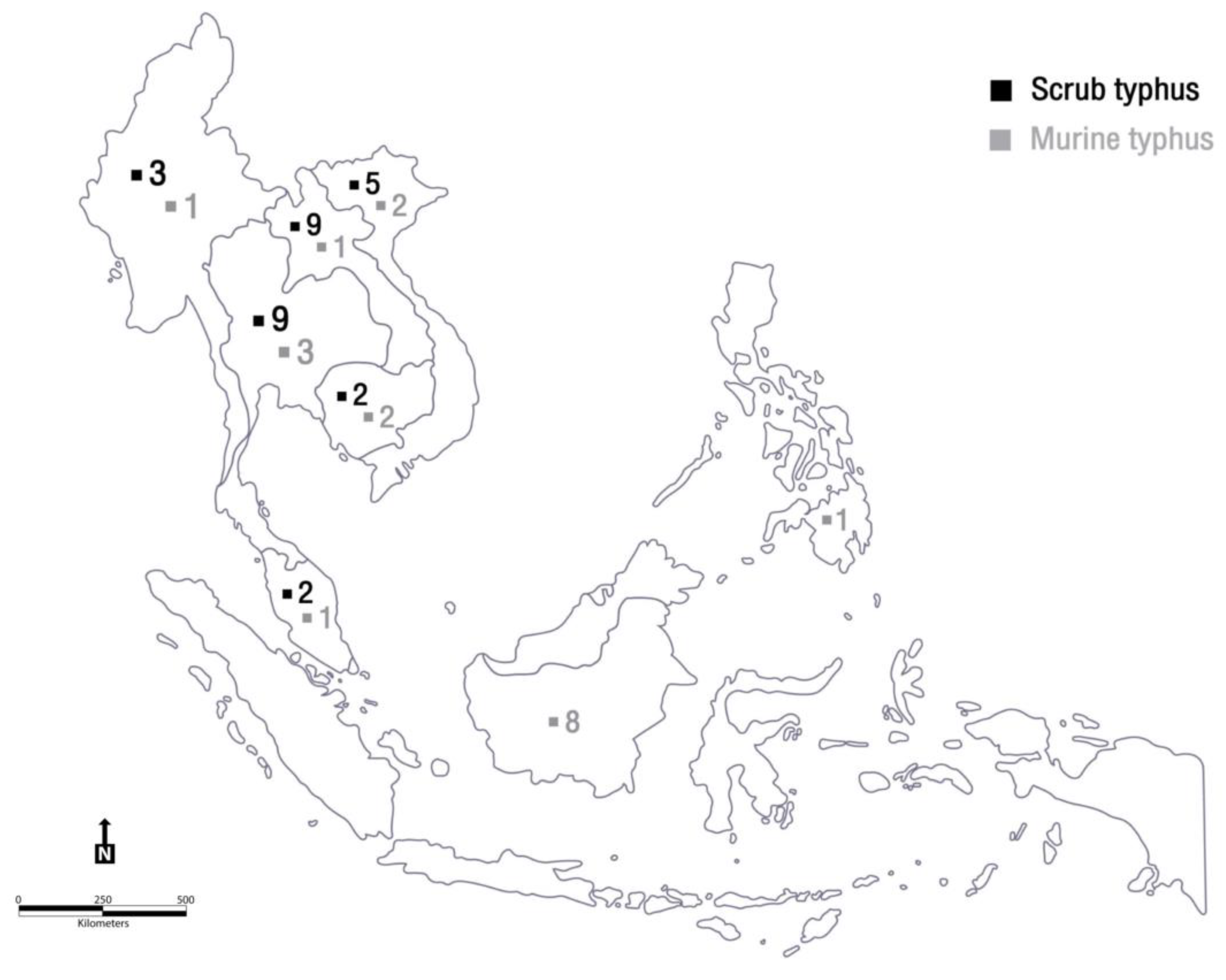
5. Travel-Associated Rickettsiosis
6. Reported Cases of Scrub Typhus and Murine Typhus in Travellers from SEA
7. Impact of the COVID-19 Pandemic on Rickettsiosis
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Buss, I.; Genton, B.; D’Acremont, V. Aetiology of fever in returning travellers and migrants: A systematic review and meta-analysis. J. Travel Med. 2020, 27, 8–32. [Google Scholar] [CrossRef] [PubMed]
- Freedman, D.O.; Weld, L.; Kozarsky, P.E.; Fisk, T.; Robins, R.; Von Sonnenburg, F.; Keystone, J.S.; Pandey, P.; Cetron, M.S. Spectrum of Disease and Relation to Place of Exposure among Ill Returned Travelers. N. Engl. J. Med. 2006, 354, 119–130. [Google Scholar] [CrossRef] [PubMed]
- Van Eekeren, L.E.; de Vries, S.G.; Wagenaar, J.F.P.; Spijker, R.; Grobusch, M.P.; Goorhuis, A. Under-diagnosis of rickettsial disease in clinical practice: A systematic review. Travel Med. Infect. Dis. 2018, 26, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Pietzsch, M.E.; Hansford, K.M.; Cull, B.; Jahfari, S.; Sprong, H.; Medlock, J.M. Detection of Dermacentor marginatus and a possible Rickettsia slovaca case in the United Kingdom—The risk of the visiting traveller. Travel Med. Infect. Dis. 2015, 13, 200–201. [Google Scholar] [CrossRef]
- Ericsson, C.D.; Jensenius, M.; Fournier, P.-E.; Raoult, D. Rickettsioses and the International Traveler. Clin. Infect. Dis. 2004, 39, 1493–1499. [Google Scholar] [CrossRef]
- Raoult, D.; Fournier, P.E.; Fenollar, F.; Jensenius, M.; Prioe, T.; De Pina, J.J.; Caruso, G.; Jones, N.; Laferl, H.; Rosenblatt, J.E.; et al. Rickettsia africae, a Tick-Borne Pathogen in Travelers to Sub-Saharan Africa. N. Engl. J. Med. 2001, 344, 1504–1510. [Google Scholar] [CrossRef]
- Jensenius, M.; Fournier, P.-E.; Kelly, P.; Myrvang, B.; Raoult, D. African tick bite fever. Lancet Infect. Dis. 2003, 3, 557–564. [Google Scholar] [CrossRef]
- Jensenius, M.; Han, P.V.; Schlagenhauf, P.; Schwartz, E.; Parola, P.; Castelli, F.; Von Sonnenburg, F.; Loutan, L.; Leder, K.; O Freedman, D. Acute and potentially life-threatening tropical diseases in western travelers—A geosentinel multicenter study, 1996–2011. Am. J. Trop. Med. Hyg. 2013, 88, 397–404. [Google Scholar] [CrossRef]
- Jensenius, M.; Davis, X.; Von Sonnenburg, F.; Schwartz, E.; Keystone, J.S.; Leder, K.; Lopéz-Véléz, R.; Caumes, E.; Cramer, J.P.; Chen, L.; et al. Multicenter GeoSentinel Analysis of Rickettsial Diseases in International Travelers, 1996–2008. Emerg. Infect. Dis. 2009, 15, 1791–1798. [Google Scholar] [CrossRef]
- Civen, R.; Ngo, V. Murine Typhus: An Unrecognized Suburban Vectorborne Disease. Clin. Infect. Dis. 2008, 46, 913–918. [Google Scholar] [CrossRef]
- Doppler, J.F.; Newton, P.N. A systematic review of the untreated mortality of murine typhus. PLoS Negl. Trop. Dis. 2020, 14, e0008641. [Google Scholar] [CrossRef] [PubMed]
- Bonell, A.; Lubell, Y.; Newton, P.N.; Crump, J.A.; Paris, D.H. Estimating the burden of scrub typhus: A systematic review. PLoS Negl. Trop. Dis. 2017, 11, e0005838. [Google Scholar] [CrossRef] [PubMed]
- Jiang, J.; Sangkasuwan, V.; Lerdthusnee, K.; Sukwit, S.; Chuenchitra, T.; Rozmajzl, P.J.; Eamsila, C.; Jones, J.W.; Richards, A.L. Human Infection with Rickettsia honei, Thailand. Emerg. Infect. Dis. 2005, 11, 1473–1475. [Google Scholar] [CrossRef] [PubMed]
- Aung, A.K.; Spelman, D.W.; Murray, R.J.; Graves, S. Rickettsial infections in Southeast Asia: Implications for local populace and febrile returned travelers. Am. J. Trop. Med. Hyg. 2014, 91, 451–460. [Google Scholar] [CrossRef] [PubMed]
- Jiang, J.; Soeatmadji, D.W.; Henry, K.M.; Ratiwayanto, S.; Bangs, M.J.; Richards, A.L. Rickettsia felis in Xenopsylla cheopis, Java, Indonesia. Emerg. Infect. Dis. 2006, 12, 1281–1283. [Google Scholar] [CrossRef]
- Fournier, P.-E.; Allombert, C.; Supputamongkol, Y.; Caruso, G.; Brouqui, P.; Raoult, D. Aneruptive Fever Associated with Antibodies to Rickettsia helvetica in Europe and Thailand. J. Clin. Microbiol. 2004, 42, 816–818. [Google Scholar] [CrossRef]
- Azad, A.F. Epidemiology of murine typhus. Annu. Rev. Entomol. 1990, 35, 553–569. [Google Scholar] [CrossRef]
- Cowan, G. Rickettsial diseases: The typhus group of fevers—A review. Postgrad. Med J. 2000, 76, 269–272. [Google Scholar] [CrossRef]
- Hendershot, E.F.; Sexton, D.J. Scrub typhus and rickettsial diseases in international travelers: A review. Curr. Infect. Dis. Rep. 2008, 11, 66–72. [Google Scholar] [CrossRef]
- Newton, P.N.; Keolouangkhot, V.; Lee, S.J.; Choumlivong, K.; Sisouphone, S.; Choumlivong, K.; Vongsouvath, M.; Mayxay, M.; Chansamouth, V.; Davong, V.; et al. A Prospective, Open-label, Randomized Trial of Doxycycline Versus Azithromycin for the Treatment of Uncomplicated Murine Typhus. Clin. Infect. Dis. 2019, 68, 738–747. [Google Scholar] [CrossRef]
- Tsioutis, C.; Zafeiri, M.; Avramopoulos, A.; Prousali, E.; Miligkos, M.; Karageorgos, S.A. Clinical and laboratory characteristics, epidemiology, and outcomes of murine typhus: A systematic review. Acta Trop. 2017, 166, 16–24. [Google Scholar] [CrossRef] [PubMed]
- Suputtamongkol, Y.; Suttinont, C.; Niwatayakul, K.; Hoontrakul, S.; Limpaiboon, R.; Chierakul, W.; Losuwanaluk, K.; Saisongkork, W. Epidemiology and Clinical Aspects of Rickettsioses in Thailand. Ann. N. Y. Acad. Sci. 2009, 1166, 172–179. [Google Scholar] [CrossRef] [PubMed]
- Watt, G.; Strickman, D. Life-Threatening Scrub Typhus in a Traveler Returning from Thailand. Clin. Infect. Dis. 1994, 18, 624–626. [Google Scholar] [CrossRef] [PubMed]
- Cracco, C.; Delafosse, C.; Baril, L.; Lefort, Y.; Morelot, C.; Derenne, J.-P.; Bricaire, F.; Similowski, T. Multiple Organ Failure Complicating Probable Scrub Typhus. Clin. Infect. Dis. 2000, 31, 191–192. [Google Scholar] [CrossRef]
- Wong, S.Y.; Lam, M.S. Rickettsioses: The new and old diseases. Singap. Med. J. 2001, 42, 546–548. [Google Scholar]
- Sekhar, W.Y.; Devi, S. The increasing prevalence of Endemic Typhus in Kuala Lumpur and an evaluation of a diagnostic ELISA dot test for the detection of antibodies to Rickettsia typhi. Singap. Med. J. 2000, 41, 226–231. [Google Scholar]
- Thitivichianlert, S.; Panichkul, S.; Bodhidatta, D.; Rodkvamtook, W.; Sukwit, S.; Boonmee, P.; Ketupanya, A. Incidence of rickettsial infection in patients with acute fever in provincial Thai army hospitals. J. Med. Assoc. Thail. 2009, 92 (Suppl. 1), S39–S46. [Google Scholar]
- Luvira, V.; Silachamroon, U.; Piyaphanee, W.; Lawpoolsri, S.; Chierakul, W.; Leaungwutiwong, P.; Thawornkuno, C.; Wattanagoon, Y. Etiologies of Acute Undifferentiated Febrile Illness in Bangkok, Thailand. Am. J. Trop. Med. Hyg. 2019, 100, 622–629. [Google Scholar] [CrossRef]
- Katoh, S.; Cuong, N.C.; Hamaguchi, S.; Thuy, P.T.; Cuong, D.D.; Anh, L.K.; Anh, N.T.H.; Anh, D.D.; Sando, E.; Suzuki, M.; et al. Challenges in diagnosing scrub typhus among hospitalized patients with undifferentiated fever at a national tertiary hospital in northern Vietnam. PLoS Negl. Trop. Dis. 2019, 13, e0007928. [Google Scholar] [CrossRef]
- Grigg, M.J.; William, T.; Clemens, E.G.; Patel, K.; Chandna, A.; Wilkes, C.S.; Barber, B.E.; Anstey, N.M.; Dumler, J.S.; Yeo, T.W.; et al. Rickettsioses as Major Etiologies of Un-recognized Acute Febrile Illness, Sabah, East Malaysia. Emerg. Infect. Dis. 2020, 26, 1409–1419. [Google Scholar] [CrossRef]
- Azuma, M.; Nishioka, Y.; Ogawa, M.; Takasaki, T.; Sone, S.; Uchiyama, T. Murine Typhus from Vietnam, Imported into Japan. Emerg. Infect. Dis. 2006, 12, 1466–1468. [Google Scholar] [CrossRef] [PubMed]
- Rahman, A.; Tegnell, A.; Vene, S.; Giesecke, J. Rickettsioses in Swedish Travellers, 1997–2001. Scand. J. Infect. Dis. 2003, 35, 247–250. [Google Scholar] [CrossRef] [PubMed]
- Rodkvamtook, W.; Gaywee, J.; Kanjanavanit, S.; Ruangareerate, T.; Richards, A.L.; Sangjun, N.; Jeamwattanalert, P.; Sirisopana, N. Scrub typhus out-break, northern Thailand, 2006–2007. Emerg. Infect. Dis. 2013, 19, 774–777. [Google Scholar] [CrossRef] [PubMed]
- Parola, P.; Vogelaers, D.; Roure, C.; Janbon, F.; Raoult, D. Murine typhus in travelers returning from Indonesia. Emerg. Infect. Dis. 1998, 4, 677–680. [Google Scholar] [CrossRef] [PubMed]
- Kelly, D.J.; Richards, A.L.; Temenak, J.; Strickman, D.; Dasch, G. The Past and Present Threat of Rickettsial Diseases to Military Medicine and International Public Health. Clin. Infect. Dis. 2002, 34, S145–S169. [Google Scholar] [CrossRef]
- Graves, S.; Stenos, J.; Unsworth, N.; Nguyen, C. Laboratory diagnosis of rickettsial infection. Aust. J. Med. Sci. 2006, 27, 39–44. [Google Scholar]
- Wilde, H.; Suankratay, C. There is Need for Antigen-Based Rapid Diagnostic Tests to Identify Common Acute Tropical Illnesses. J. Travel Med. 2007, 14, 254–258. [Google Scholar] [CrossRef]
- Olson, J.G.; Bourgeois, A.L.; Fang, R.C.; Coolbaugh, J.C.; Dennis, D.T. Prevention of scrub typhus. Prophylactic administration of doxycycline in a randomized double blind trial. Am. J. Trop. Med. Hyg. 1980, 29, 989–997. [Google Scholar] [CrossRef]
- Twartz, J.C.; Shirai, A.; Selvaraju, G.; Saunders, J.P.; Huxsoll, D.L.; Groves, M.G. Doxycycline propylaxis for human scrub typhus. J. Infect. Dis. 1982, 146, 811–818. [Google Scholar] [CrossRef]
- Osterloh, A. The neglected challenge: Vaccination against rickettsiae. PLoS Negl. Trop. Dis. 2020, 14, e0008704. [Google Scholar] [CrossRef]
- World Tourism Organization. International Tourism Highlights, 2020 Edition. 2021. Available online: https://www.e-unwto.org/doi/book/10.18111/9789284422456 (accessed on 18 December 2021).
- Chinazzi, M.; Davis, J.T.; Ajelli, M.; Gioannini, C.; Litvinova, M.; Merler, S.; Piontti, Y.; Pastore, A.; Mu, K.; Rossi, L.; et al. The Effect of Travel Restrictions on the Spread of the 2019 Novel Coronavirus (COVID-19) Outbreak. Science 2020, 368, 395–400. [Google Scholar] [CrossRef] [PubMed]
- Lin, E.-C.; Tu, H.-P.; Hong, C.-H. Halved Incidence of Scrub Typhus after Travel Restrictions to Confine a Surge of COVID-19 in Taiwan. Pathogens 2021, 10, 1386. [Google Scholar] [CrossRef] [PubMed]
- Van der Vaart, T.W.; van Thiel, P.P.; Juffermans, N.P.; van Vugt, M.; Geerlings, S.E.; Grobusch, M.P.; Goorhuis, A. Severe murine ty-phus with pulmonary system involvement. Emerg. Infect. Dis. 2014, 20, 1375–1377. [Google Scholar] [CrossRef] [PubMed]
- Sirisanthana, V.; Puthanakit, T.; Sirisanthana, T. Epidemiologic, clinical and laboratory features of scrub typhus in thirty Thai children. Pediatr. Infect. Dis. J. 2003, 22, 341–345. [Google Scholar] [CrossRef] [PubMed]
- Almutairi, N.; Schwartz, R.A. COVID-19 with dermatologic manifestations and implications: An unfolding conundrum. Dermatol. Ther. 2020, 33, e13544. [Google Scholar] [CrossRef]
- Patel, H.M. Murine typhus mistaken for COVID-19 in a young man. BMJ Case Rep. 2020, 13, e239471. [Google Scholar] [CrossRef]
- Ihara, S.; Shikino, K.; Ikusaka, M. A case of availability bias for COVID-19 causing scrub typhus diagnostic errors. J. Gen. Fam. Med. 2021, 23, 52–53. [Google Scholar] [CrossRef]
- Hazra, D.; Abhilash, K.P.; Gunasekharan, K.; Prakash, J.A. Eschar: An indispensable clue for the diagnosis of scrub typhus and COVID-19 co-infection during the ongoing pandemic. J. Postgrad. Med. 2021, 67, 117–118. [Google Scholar] [CrossRef]
- Chang, W.-H. The influences of the COVID-19 pandemic on medical service behaviors. Taiwan. J. Obstet. Gynecol. 2020, 59, 821–827. [Google Scholar] [CrossRef]
- Seilmaier, M.; Guggemos, W.; Böhme, C.C.; Löscher, T. Tsutusgamushi fever after travel to Southeast Asia. Dtsch. Med. Wochenschr. 2004, 129, 2233–2235. [Google Scholar] [CrossRef]
- Jensenius, M.; Montelius, R.; Berild, D.; Vene, S. Scrub typhus imported to Scandinavia. Scand. J. Infect. Dis. 2006, 38, 200–202. [Google Scholar] [CrossRef] [PubMed]
- Keller, C.; Fähndrich, K.; Müller, W.; Nüßlein, T.G.; Fleischer, B.; Hegasy, G. Epistaxis, Maculopapular Rash and Fever in a German Boy after a Stay in Thailand Caused by Orientia Tsutsugamushi. Klin Padiatr. 2012, 224, 270–271. [Google Scholar] [CrossRef] [PubMed]
- Edouard, S.; Subramanian, G.; Lefevre, B.; Dos Santos, A.; Pouedras, P.; Poinsignon, Y.; Mediannikov, O.; Raoult, D. Co-infection with Arsenophonus nasoniae and Orientia tsutsugamushi in a traveler. Vector Borne Zoonotic Dis. 2013, 13, 565–571. [Google Scholar] [CrossRef] [PubMed]
- Vliegenthart-Jongbloed, K.; Melo, M.D.M.; Slobbe, L.; Beersma, M.F.; van Genderen, P. Imported scrub typhus in the Netherlands. Travel Med. Infect. Dis. 2013, 11, 197–199. [Google Scholar] [CrossRef] [PubMed]
- Angelakis, E.; Patrick, G.; Peloni, J.M.; Wey, P.F.; Perreal, C.; Raoult, D. Orientia tsutsugamushi in lung of patient with acute respiratory distress syndrome, France, 2013. Emerg. Infect. Dis. 2015, 21, 373–375. [Google Scholar] [CrossRef]
- Theunissen, C.; Cnops, L.; Van Esbroeck, M.; Huits, R.; Bottieau, E. Acute-phase diagnosis of murine and scrub typhus in Belgian travelers by polymerase chain reaction: A case report. BMC Infect. Dis. 2017, 17, 273. [Google Scholar] [CrossRef] [PubMed]
- De Vries, S.G.; van Eekeren, L.E.; van der Linden, H.; Visser, B.J.; Grobusch, M.P.; Wagenaar, J.F.P.; Goris, M.G.A.; Goorhuis, A. Searching and Finding the Hidden Treasure: A Retrospective Analysis of Rickettsial Disease Among Dutch International Travelers. Clin. Infect. Dis. 2021, 72, 1171–1178. [Google Scholar] [CrossRef]
- Eisermann, P.; Rauch, J.; Reuter, S.; Eberwein, L.; Mehlhoop, U.; Allartz, P.; Muntau, B.; Tappe, D. Complex Cytokine Responses in Im-ported Scrub Typhus Cases, Germany, 2010–2018. Am. J. Trop. Med. Hyg. 2020, 102, 63–68. [Google Scholar] [CrossRef]
- Costa, C.; Ferrari, A.; Binazzi, R.; Beltrame, A.; Tacconi, D.; Moro, L.; Edouard, S.; Parola, P.; Buonfrate, D.; Gobbi, F. Imported scrub typhus in Europe: Report of three cases and a literature review. Travel Med. Infect. Dis. 2021, 42, 102062. [Google Scholar] [CrossRef]
- Slesak, G.; Döller, P.C. Fever and calf tenderness after travel in Thailand: Murine typhus and deep vein thrombosis. Dtsch. Med. Wochenschr. 2001, 126, 649–652. [Google Scholar] [CrossRef]
- Takeshita, N.; Imoto, K.; Ando, S.; Yanagisawa, K.; Ohji, G.; Kato, Y.; Sakata, A.; Hosokawa, N.; Kishimoto, T. Murine Typhus in Two Travelers Returning from Bali, Indonesia: An Underdiagnosed Disease. J. Travel Med. 2010, 17, 356–358. [Google Scholar] [CrossRef] [PubMed]
- Stockdale, A.J.; Weekes, M.P.; Kiely, B.; Lever, A.M. Case report: Severe typhus group rickettsiosis complicated by pulmonary edema in a returning traveler from Indonesia. Am. J. Trop. Med. Hyg. 2011, 85, 1121–1123. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Iacobucci, G. COVID-19: Runny nose, headache, and fatigue are commonest symptoms of omicron, early data show. BMJ 2021, 375, n3103. [Google Scholar] [CrossRef] [PubMed]
- Walter, G.; Socolovschi, C.; Raoult, D.; Parola, P.; Botelho-Nevers, E. Murine Typhus in Returned Travelers: A Report of Thirty-Two Cases. Am. J. Trop. Med. Hyg. 2012, 86, 1049–1053. [Google Scholar] [CrossRef] [PubMed]
- Raby, E.; Dyer, J.R. Endemic (Murine) Typhus in Returned Travelers from Asia, a Case Series: Clues to Early Diagnosis and Comparison with Dengue. Am. J. Trop. Med. Hyg. 2013, 88, 701–703. [Google Scholar] [CrossRef] [PubMed]
- Sakamoto, N.; Nakamura-Uchiyama, F.; Kobayashi, K.; Takasaki, T.; Ogasawara, M.Y.; Ando, D.S.; Iwabuchi, S.; Ohnishi, K. Severe Murine Typhus with Shock and Acute Respiratory Failure in a Japanese Traveler After Returning From Thailand. J. Travel Med. 2012, 20, 50–53. [Google Scholar] [CrossRef]
- Yoshimura, Y.; Sakamoto, Y.; Kwangyeol, L.; Amano, Y.; Tachikawa, N. Round Pneumonia with Murine Typhus after Travel to Indonesia. J. Travel Med. 2015, 22, 353–354. [Google Scholar] [CrossRef][Green Version]
- Rauch, J.; Eisermann, P.; Noack, B.; Mehlhoop, U.; Muntau, B.; Schäfer, J.; Tappe, D. Typhus Group Rickettsiosis, Germany, 2010–20171. Emerg. Infect. Dis. 2018, 24, 1213–1220. [Google Scholar] [CrossRef]

| Year | Age and Sex | Visited Countries | Citizenship | Risky Activities | Outcome |
|---|---|---|---|---|---|
| 2000 [24] | 32 F | Myanmar and Thailand | French | NA | Fully recovered |
| 2004 [41] | 49 M | Vietnam, Thailand and Myanmar | German | NA | Improvement |
| 2006 [42] | 40 F | Thailand | Swedish | Jungle trip in Chiang Mai | Discharged |
| 67 F | Laos | Swedish | Hiking along Mekong River | Improvement | |
| 2012 [43] | 15 M | Thailand | German | Vacation on Koh Samui | Discharged |
| 2013 [44] | 31 F | Cambodia | French | Jungle trip | Improvement |
| 2013 [45] | 27 F | Laos | Dutch | Basic travelling through SEA | Recovered |
| 2015 [46] | 50 F | Laos | French | Jungle trip | Fever resolved |
| 2017 [47] | 23 F | Cambodia and Vietnam | Belgian | Hiking through high grass, bushes, and paddy fields | NA |
| 23 F | Thailand, Laos, and Vietnam | Belgian | Hiking through woods and caves and boat trip on the Mekong River | Fever resolved | |
| 2020 [48] | 33 M 42 M | Malaysia and Borneo Thailand | Dutch Dutch | NA | NA |
| 2020 [49] | 55 M 50 F 34 M 35 M 27 F 51 M 61 M 19 M | Laos Laos and Thailand Vietnam Thailand and Malaysia Thailand Thailand Myanmar Vietnam | Data retrieved from German Reference Center for Tropical Medicine | NA | All resolved |
| 2021 [50] | 55 M 38 F 35 M | Laos Laos Laos | Italian Italian Italian | 12-day hiking and camping trip to the forest of Northern Laos | Recovered |
| Year | Age and Sex | Visited Countries | Citizenship | Risky Activities | Outcome |
|---|---|---|---|---|---|
| 2001 [51] | 37 M | Thailand | German | NA | Recovered |
| 2006 [52] | 54 M | Vietnam | Japanese | NA | NA |
| 2010 [53] | 23 M | Indonesia | Japanese | Surfing and stayed at guesthouses and local friends’ residences in Kuta and Madewi (Bali) | Improvement |
| 23 M | Indonesia | Japanese | NA | Improvement | |
| 2011 [54] | 29 M | Indonesia | NA | Visiting both urban and rural areas in Bali and Lombok; seeing rat in his accommodation; and multiple insect bites but no tick bites | Improvement |
| 2012 [55] | Retrospective 12 cases | Indonesia, Philippines, Thailand, Cambodia, Vietnam, Myanmar, or Laos | French | Tourism, business, and visiting friends and relatives | Recovered |
| 2013 [56] | 53 F | Indonesia | NA | Close contact with animals in safari park and multiple insect bites in Bali | Complete recovery |
| 59 F | Indonesia | NA | NA | Slow recovery | |
| 2013 [57] | 56 M | Thailand | Japanese | Working as a Japanese language teacher | Improvement |
| 2015 [58] | 43 M | Bali and Indonesia | Japanese | NA | Improvement |
| 2017 [47] | 37 F | Indonesia and Malaysia | Belgian | A 24-day adventurous travel staying at local accommodation for several nights | Improvement |
| 2018 [59] (only R. typhi confirmation) | 57 M | Cambodia | German | NA | NA |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ngamprasertchai, T.; Hanboonkunupakarn, B.; Piyaphanee, W. Rickettsiosis in Southeast Asia: Summary for International Travellers during the COVID-19 Pandemic. Trop. Med. Infect. Dis. 2022, 7, 18. https://doi.org/10.3390/tropicalmed7020018
Ngamprasertchai T, Hanboonkunupakarn B, Piyaphanee W. Rickettsiosis in Southeast Asia: Summary for International Travellers during the COVID-19 Pandemic. Tropical Medicine and Infectious Disease. 2022; 7(2):18. https://doi.org/10.3390/tropicalmed7020018
Chicago/Turabian StyleNgamprasertchai, Thundon, Borimas Hanboonkunupakarn, and Watcharapong Piyaphanee. 2022. "Rickettsiosis in Southeast Asia: Summary for International Travellers during the COVID-19 Pandemic" Tropical Medicine and Infectious Disease 7, no. 2: 18. https://doi.org/10.3390/tropicalmed7020018
APA StyleNgamprasertchai, T., Hanboonkunupakarn, B., & Piyaphanee, W. (2022). Rickettsiosis in Southeast Asia: Summary for International Travellers during the COVID-19 Pandemic. Tropical Medicine and Infectious Disease, 7(2), 18. https://doi.org/10.3390/tropicalmed7020018







