Contribution of Testing Strategies and Contact Tracing towards COVID-19 Outbreaks Control: A Mathematical Modeling Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Simulation Scenarios
- Symptomatic Screening: We assumed that all symptomatic cases are immediately presented to clinics for RT-PCR testing.
- We further simulated the scenarios that either 30%, 50%, 70%, or 100% of symptomatic cases are immediately presented to clinics for RT-PCR testing. We simply designated “30%, 50%, 70%, or 100% of symptomatic screening” to represent the corresponding scenarios.
- We assumed sufficient testing capacity to accommodate all cases presented to the clinics.
- Universal testing: We assumed that asymptomatic and subclinical cases have the potential to obtain universal testing based on the proportion of total testing capacity to the population size. Due to the severity of outbreaks in the United States (USA) and United Kingdom (UK), we assumed that both countries reach their maximum testing capacities each day. Current universal testing capacities are approximately 0.5% of the total population per day in the USA and 1% of the total population in the UK [26,27]. However, current universal testing capacities in some Asian settings such as Taiwan and the Republic of Korea (South Korea) are approximately 0.05% and 0.03% of the total populations per day, respectively [25,28]. We chose to analyze the 0.5% capacity in the USA as a representation of current universal testing capacity. Therefore, the current and projected universal testing capacity scenarios analyzed are as follows:
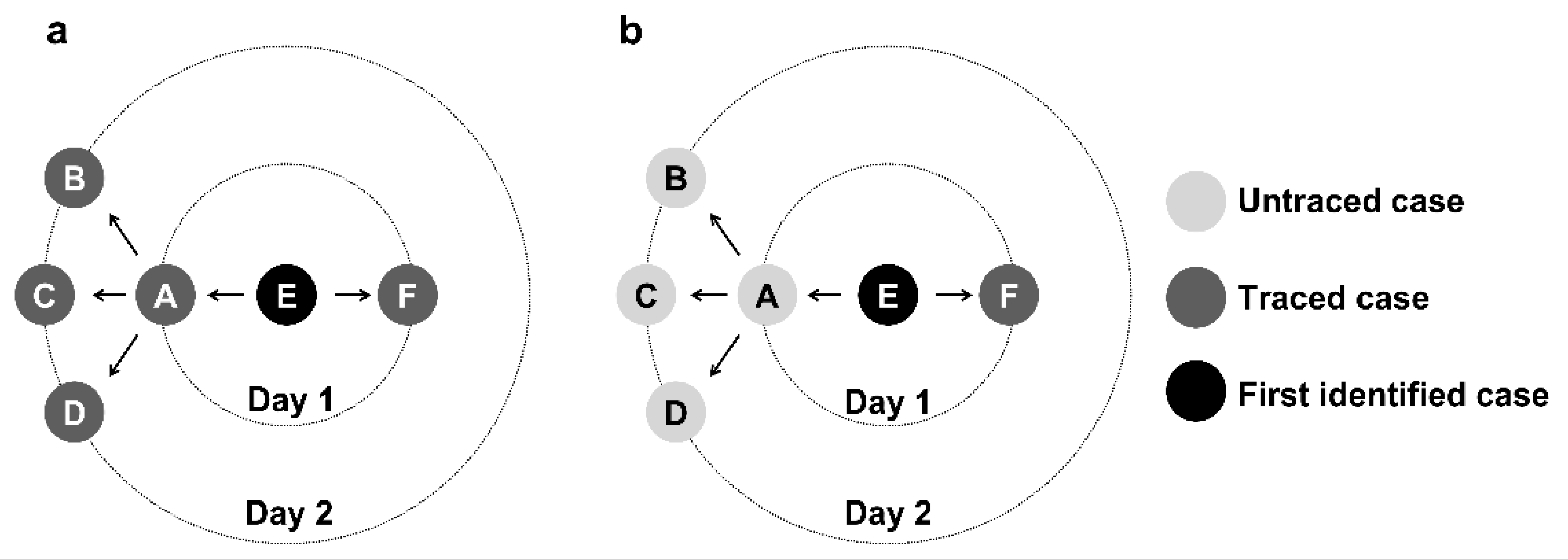
2.3. Control Strategies
2.4. Outbreak Control
2.5. Definition of High/Low Prevalence Rate Countries
2.6. Simulations
3. Results
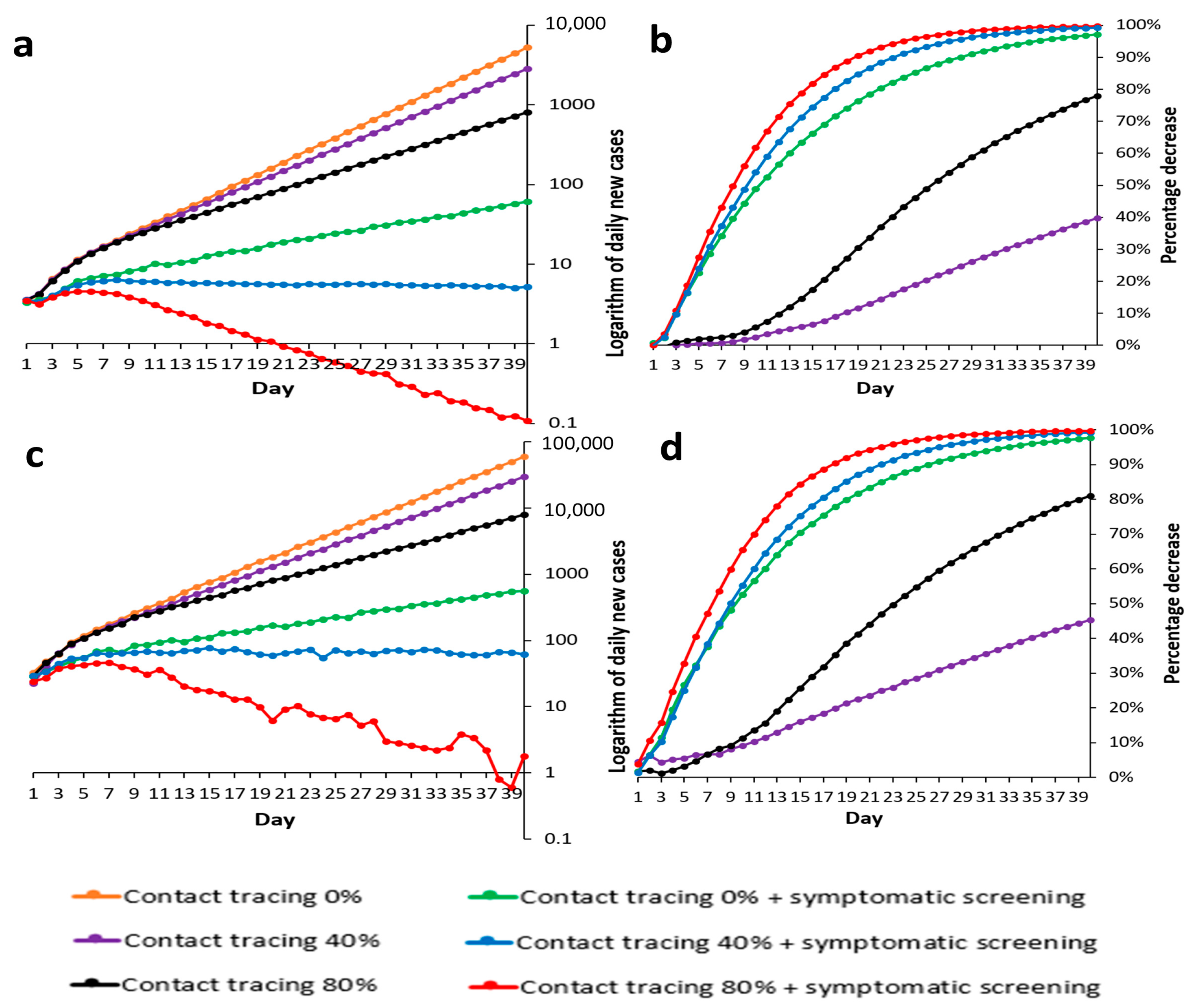
3.1. Low Prevalence Countries
3.1.1. Countries with 40–80% Contact Tracing Success Rates
3.1.2. Countries with No Contact Tracing
3.1.3. The SARS-CoV-2 Omicron Variant Scenario
3.2. High Prevalence Countries
3.2.1. Countries with 40–80% Contact Tracing Success Rates
3.2.2. Countries with No Contact Tracing
3.3. Time to Outbreak Control with 100% or 50% Symptomatic Screening
4. Discussion
5. Limitations
6. Future Work
7. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kucharski, A.J.; Russell, T.W.; Diamond, C.; Liu, Y.; Edmunds, J.; Funk, S.; Eggo, M.R. Early dynamics of transmission and control of COVID-19: A mathematical modelling study. Lancet Infect. Dis. 2020, 20, 553–558. [Google Scholar] [CrossRef]
- Cheong, K.H.; Wen, T.; Lai, J.W. Relieving cost of epidemic by parrondo’s paradox: A COVID-19 case study. Adv. Sci. 2020, 7, 2002324. [Google Scholar] [CrossRef] [PubMed]
- Lai, J.W.; Cheong, K.H. Superposition of COVID-19 waves, anticipating a sustained wave, and lessons for the future. BioEssays 2020, 42, 2000178. [Google Scholar] [CrossRef] [PubMed]
- Cheong, K.H.; Jones, M.C. Introducing the 21st century’s new four horsemen of the coronapocalypse. BioEssays 2020, 4, 2000063. [Google Scholar] [CrossRef] [PubMed]
- Kretzschmar, M.E.; Rozhnova, G.; Bootsma, M.C.; van Boven, M.; van de Wijgert, J.H.; Bonten, M.J. Impact of delays on effectiveness of contact tracing strategies for COVID-19: A modelling study. Lancet Public Health 2020, 5, e452–e459. [Google Scholar] [CrossRef]
- Aleta, A.; Martin-Corral, D.; Pastore y Piontti, A.; Ajelli, M.; Litvinova, M.; Chinazzi, M.; Dean, N.E.; Halloran, M.E.; Longini, I.M., Jr.; Merler, S.; et al. Modelling the impact of testing, contact tracing and household quarantine on second waves of COVID-19. Nat. Hum. Behav. 2020, 4, 964–971. [Google Scholar] [CrossRef]
- Jian, S.W.; Cheng, H.Y.; Huang, X.T.; Liu, D.P. Contact tracing with digital assistance in Taiwan’s COVID-19 outbreak response. Int. J. Infect. Dis. 2020, 101, 348–352. [Google Scholar] [CrossRef]
- Wang, C.J.; Ng, C.Y.; Brook, R.H. Response to COVID-19 in Taiwan. Big Data Analytics, New Technology, and Proactive Testing. JAMA 2020, 323, 1341–1342. [Google Scholar] [CrossRef]
- Libin, P.K.; Willem, L.; Verstraeten, T.; Torneri, A.; Vanderlocht, J.; Hens, N. Assessing the feasibility and effectiveness of household-pooled universal testing to control COVID-19 epidemics. PLoS Comput. Biol. 2021, 17, e1008688. [Google Scholar] [CrossRef]
- Pan, J.; Chen, Z.; He, Y.; Liu, T.; Li, Q.; Cheng, X.; Xiao, J.; Feng, H. Why Controlling the Asymptomatic Infection Is Important: A Modelling Study with Stability and Sensitivity Analysis. Fractal Fract. 2022, 6, 197. [Google Scholar] [CrossRef]
- Gao, Z.; Xu, Y.; Sun, C.; Wang, X.; Guo, Y.; Qiu, S.; Ma, K. A systematic review of asymptomatic infections with COVID-19. J. Microbiol. Immunol. Infect. 2021, 54, 12–16. [Google Scholar] [CrossRef] [PubMed]
- Larremore, D.B.; Wilder, B.; Lester, E.; Shehata, S.; Burke, J.M.; Hay, J.A.; Tambe, M.; Mina, M.J.; Parker, R. Test sensitivity is secondary to frequency and turnaround time for COVID-19 screening. Sci. Adv. 2021, 7, eabd5393. [Google Scholar] [CrossRef] [PubMed]
- BALLOTPEDIA. Arguments about Universal or Mass Testing for COVID-19 before the Economy Can Reopen. Available online: https://ballotpedia.org/Arguments_about_universal_or_mass_testing_for_COVID-19_before_the_economy_can_reopen (accessed on 29 September 2022).
- Hellewell, J.; Abbott, S.; Gimma, A.; Bosse, N.I.; Jarvis, C.I.; Russell, T.W.; Munday, J.D.; Kucharski, A.D.; Edmunds, W.J. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Glob. Health 2020, 8, e488–e496. [Google Scholar] [CrossRef]
- Tsou, H.H.; Cheng, Y.C.; Yuan, H.Y.; Hsu, Y.T.; Wu, H.Y.; Lee, F.J.; Hsiung, C.A.; Chen, W.J.; Sytwu, H.K.; Wu, S.I.; et al. The effect of preventing subclinical transmission on the containment of COVID-19: Mathematical modeling and experience in Taiwan. Contemp. Clin. Trials 2020, 96, 106101. [Google Scholar] [CrossRef] [PubMed]
- Burki, T.K. Omicron variant and booster COVID-19 vaccines. Lancet Respir. Med. 2022, 10, e17. [Google Scholar] [CrossRef]
- Liu, T.; Hu, J.; Kang, M.; Rong, Z.; Lin, L.; Zhong, H.; Huang, Q.; Deng, A.; Huang, Q.; Deng, A.; et al. Time-varying transmission dynamics of Novel Coronavirus Pneumonia in China. BioRxiv 2020. [Google Scholar] [CrossRef]
- Backer, J.A.; Klinkenberg, D.; Wallinga, J. Incubation period of 2019 novel coronavirus (2019-nCoV) infections among travellers from Wuhan, China, 20–28 January 2020. Eurosurveillance 2020, 25, 2000062. [Google Scholar] [CrossRef]
- Helmsdal, G.; Hansen, O.K.; Moller, L.F.; Christiansen, D.H.; Petersen, M.S.; Kristiansen, M.F. Omicron outbreak at a private gathering in the Faroe Islands, infecting 21 of 33 triple-vaccinated healthcare workers. Clin. Infect. Dis. 2022, 75, 893–896. [Google Scholar] [CrossRef]
- UK Health Security Agency. Omicron and Delta Serial Interval Distributions from UK Contact Tracing Data. 31 December 2021. Available online: https://www.gov.uk/government/publications/ukhsa-omicron-and-delta-serial-interval-distributions-from-uk-contact-tracing-data-31-december-2021 (accessed on 22 February 2022).
- Oran, D.P.; Topol, E.J. Prevalence of asymptomatic SARS-CoV-2 infection. Ann. Intern. Med. 2020, 173, 362–367. [Google Scholar] [CrossRef]
- Garrett, N.; Tapley, A.; Andriesen, J.; Seocharan, I.; Fisher, L.H.; Bunts, L.; Espy, N.; Wallis, C.L.; Randhawa, A.K.; Miner, M.D. High Asymptomatic Carriage with the Omicron Variant in South Africa. Clin Infect Dis. 2022, 75, e289–e292. [Google Scholar] [CrossRef]
- Casey-Bryars, M.; Griffin, J.; McAloon, C.; Byrne, A.; Madden, J.; Evoy, D.C.; Collins, A.; Hunt, K.; Barber, A.; Butler, F.; et al. Presymptomatic transmission of SARS-CoV-2 infection: A secondary analysis using published data. BMJ Open 2021, 11, e041240. [Google Scholar] [CrossRef] [PubMed]
- Padhye, N.S. Reconstructed diagnostic sensitivity and specificity of the RT-PCR test for COVID-19. MedRxiv 2021. [Google Scholar] [CrossRef]
- Ministry of Health and Welfare, Taiwan. Adequate Testing Capacity and Precisely Locate Potentially Infected Individuals. Available online: https://covid19.mohw.gov.tw/en/cp-4788-53906-206.html (accessed on 21 May 2021).
- United States Centers for Disease Control and Prevention. Data table for COVID-19 Viral (RT-PCR) Laboratory Test 30-Day Percent Positivity by State/Territory. Available online: https://covid.cdc.gov/covid-data-tracker/#testing_positivity30day (accessed on 13 January 2021).
- United Kingdom Government. Testing in United Kingdom. Available online: https://coronavirus.data.gov.uk/details/testing (accessed on 20 January 2021).
- Our World in Data. Coronavirus (COVID-19) Testing. 2021. Available online: https://ourworldindata.org/coronavirus-testing (accessed on 21 May 2021).
- Health Affairs. Universal Testing to End the Pandemic. Available online: https://www.healthaffairs.org/do/10.1377/forefront.20201102.521193/full/ (accessed on 13 January 2021).
- Covid Act Now. What Is Incidence? Covid Act Now 2020. Available online: https://blog.covidactnow.org/what-is-covid-incidence/ (accessed on 14 April 2021).
- Ferretti, L.; Wymant, C.; Kendall, M.; Zhao, L.; Nurtay, A.; Abeler-Dörner, L.; Bonsall, D.; Parker, M.; Fraser, C. Quantifying SARS-CoV-2 transmission suggests epidemic control with digital contact tracing. Science 2020, 368, eabb6936. [Google Scholar] [CrossRef] [PubMed]
- Johnson-León, M.; Caplan, A.L.; Kenny, L.; Buchan, I.; Fesi, L.; Olhava, P.; Alugnoa, D.N.; Aspinall, M.G.; Costanza, E.; Desharnais, B.; et al. Executive summary: It’s wrong not to test: The case for universal, frequent rapid COVID-19 testing. EClinicalMedicine 2021, 33, 100759. [Google Scholar] [CrossRef] [PubMed]
- United States Centers for Disease Control and Prevention. Overview of Testing for SARS-CoV-2 (COVID-19). Available online: https://www.cdc.gov/coronavirus/2019-ncov/hcp/testing-overview.html (accessed on 14 April 2021).



| Sampled | Mean (SD), n or %. | Reference |
|---|---|---|
| Delay from symptom onset to isolation | 9.76 days (7.66) | Liu et al. [17]; Tsou et al. [15] |
| Incubation period | 5.8 days (2.6) * | Backer et al. [18] |
| 3.24 days (0.8) ** | Helmsdal et al. [19] | |
| Serial interval | 5.8 days (2) * | Hellewell et al. [14] |
| 3.64 days (2.16) ** | UKHSA [20] | |
| Fixed | ||
| Initial cases | 20, 200 | Assumed |
| Contact tracing success rate | 0%, 40%, 80% | Assumed |
| Reproduction number (R0) | 2.5 * | Hellewell et al. [14] |
| 10 ** | Talha KhanBurki [16] | |
| Percentage of subclinical cases | 40% * | Oran & Topol [21] |
| 23% ** | Garrett et al. [22] | |
| Probability of pre-symptom transmission | 55% | Casey et al. [23] |
| Sensitivity of testing | 71% * | Padhye [24] |
| 97.8% ** | Taiwan CDC | |
| Current universal testing capacity (% of total population per day) | 0.05%, 0.5%, 1% | Ministry of Health and Welfare, Taiwan [25]; United States CDC [26]; United Kingdom Government [27]; OWID [28] |
| Projected universal testing capacity (% of total population per day) | 5%, 10% | Cherif et al. [29] |
| Situation | Recommendation |
|---|---|
| High populations with low COVID-19 prevalence | strategies II: contact tracing + symptomatic screening |
| Low populations with low COVID-19 prevalence | strategies II: contact tracing + symptomatic screening |
| High populations with high COVID-19 prevalence | strategies III: contact tracing + symptomatic screening+ universal testing |
| Low populations with high COVID-19 prevalence | strategies III: contact tracing + symptomatic screening+ universal testing |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuo, S.-C.; Fan, B.; Zhu, H.; Wu, M.-H.; Lee, F.-J.; Cheng, Y.-C.; Wu, H.-Y.; Hsu, Y.-T.; Hsiung, C.A.; Wu, S.-I.; et al. Contribution of Testing Strategies and Contact Tracing towards COVID-19 Outbreaks Control: A Mathematical Modeling Study. Trop. Med. Infect. Dis. 2022, 7, 376. https://doi.org/10.3390/tropicalmed7110376
Kuo S-C, Fan B, Zhu H, Wu M-H, Lee F-J, Cheng Y-C, Wu H-Y, Hsu Y-T, Hsiung CA, Wu S-I, et al. Contribution of Testing Strategies and Contact Tracing towards COVID-19 Outbreaks Control: A Mathematical Modeling Study. Tropical Medicine and Infectious Disease. 2022; 7(11):376. https://doi.org/10.3390/tropicalmed7110376
Chicago/Turabian StyleKuo, Shu-Chen, Byron Fan, Hongye Zhu, Meng-Hsuan Wu, Fang-Jing Lee, Yu-Chieh Cheng, Hsiao-Yu Wu, Ya-Ting Hsu, Chao A. Hsiung, Shiow-Ing Wu, and et al. 2022. "Contribution of Testing Strategies and Contact Tracing towards COVID-19 Outbreaks Control: A Mathematical Modeling Study" Tropical Medicine and Infectious Disease 7, no. 11: 376. https://doi.org/10.3390/tropicalmed7110376
APA StyleKuo, S.-C., Fan, B., Zhu, H., Wu, M.-H., Lee, F.-J., Cheng, Y.-C., Wu, H.-Y., Hsu, Y.-T., Hsiung, C. A., Wu, S.-I., Chen, W. J., Chiou, H.-Y., Sytwu, H.-K., & Tsou, H.-H. (2022). Contribution of Testing Strategies and Contact Tracing towards COVID-19 Outbreaks Control: A Mathematical Modeling Study. Tropical Medicine and Infectious Disease, 7(11), 376. https://doi.org/10.3390/tropicalmed7110376






