Perceived Monkeypox Concern and Risk among Men Who Have Sex with Men: Evidence and Perspectives from The Netherlands
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Measures
2.2.1. Outcome Measures
2.2.2. Socio-Demographic Determinant Measures
2.2.3. Behavioural/Health Determinant Measures
2.2.4. Psycho-Social Determinant Measures
2.3. Statistical Analyses
2.3.1. Descriptive Analysis
2.3.2. Multivariable Logistic Regression Modelling
3. Results
3.1. Study Population Characteristics
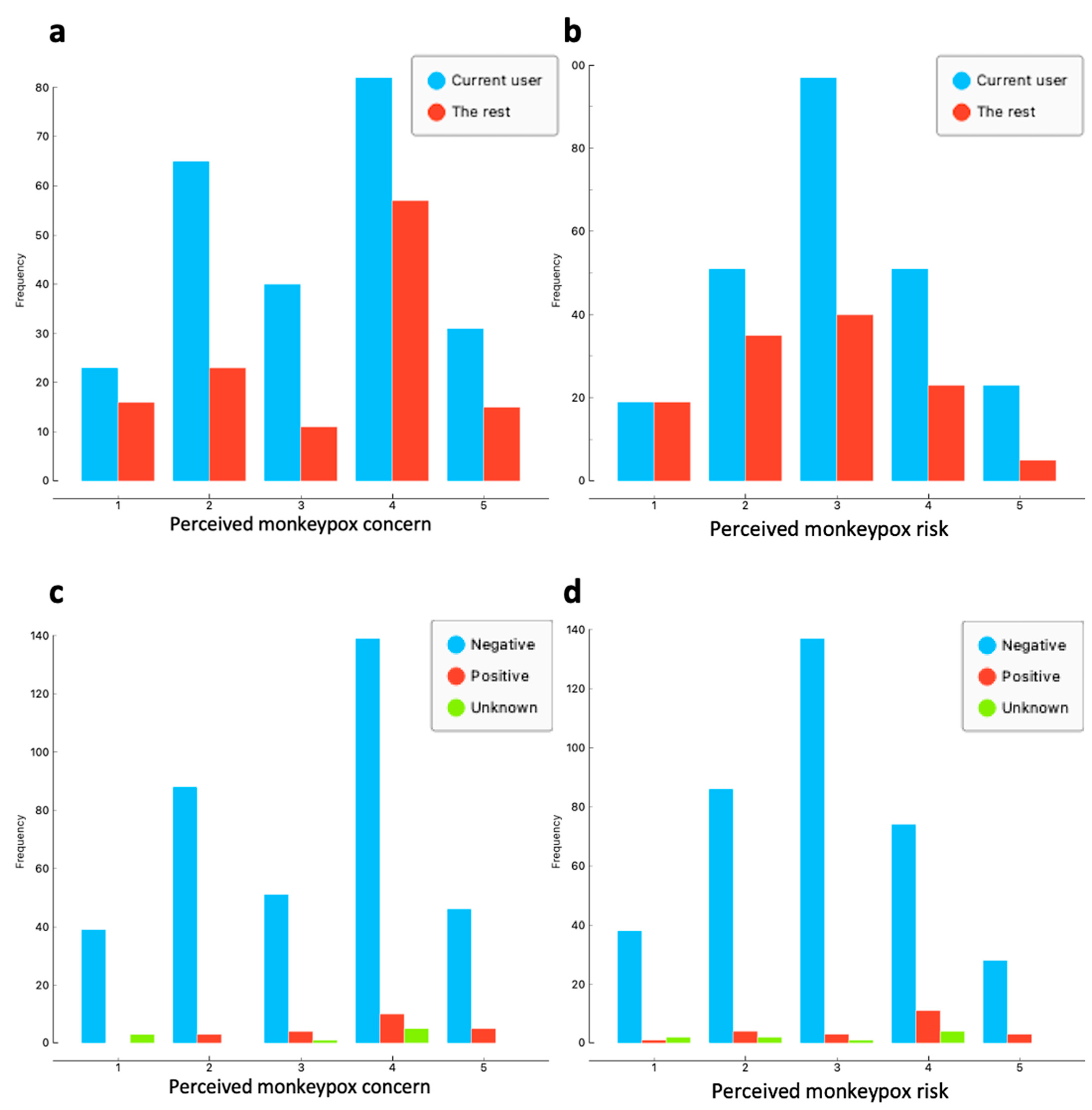
3.2. Perceived Monkeypox Concern and Risk among MSM
3.3. Determinants of Perceived Concern and Risk among MSM
4. Discussion
Limitations and Recommendations for Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bunge, E.M.; Hoet, B.; Chen, L.; Lienert, F.; Weidenthaler, H.; Baer, L.R.; Steffen, R. The changing epidemiology of human monkeypox—A potential threat? A systematic review. PLoS Negl. Trop. Dis. 2022, 16, e0010141. [Google Scholar] [CrossRef] [PubMed]
- Kozlov, M. Monkeypox goes global: Why scientists are on alert. Nature 2022, 606, 15–16. [Google Scholar] [CrossRef]
- World Health Orgnization. Responding to the Monkeypox Outbreak: Perspectives of Clinicians Treating Patients with the Disease; WHO: Geneva, Switzerland, 2022. [Google Scholar]
- RIVM. Monkeypox. 2022. Available online: https://www.rivm.nl/en/monkeypox (accessed on 6 October 2022).
- Zumla, A.; Valdoleiros, S.R.; Haider, N.; Asogun, D.; Ntoumi, F.; Petersen, E.; Kock, R. Monkeypox outbreaks outside endemic regions: Scientific and social priorities. Lancet Infect. Dis. 2022, 22, 929–931. [Google Scholar] [CrossRef]
- ECDC. Joint ECDC-WHO Regional Office for Europe Monkeypox Surveillance Bulleten. 2022. Available online: https://monkeypoxreport.ecdc.europa.eu/ (accessed on 6 October 2022).
- Gonsalves, G.S.; Mayer, K.; Beyrer, C. Déjà vu All Over Again? Emergent Monkeypox, Delayed Responses, and Stigmatized Populations. J. Urban Health. 2022, 99, 603–606. [Google Scholar] [PubMed]
- National Institute for Public Health and the Environment (RIVM). Monkeypox Vaccination. 2022. Available online: https://www.rivm.nl/en/monkeypox/vaccination (accessed on 6 October 2022).
- RIVM. Monkeypox (Apenpokken). 2022. Available online: https://lci.rivm.nl/richtlijnen/monkeypox-apenpokken (accessed on 6 October 2022).
- Nolasco, S.; Vitale, F.; Geremia, A.; Tramuto, F.; Maida, C.M.; Sciuto, A.; Coco, C.; Manuele, R.; Frasca, E.; Magliocco, S.; et al. First case of monkeypox virus, SARS-CoV-2 and HIV co-infection. J. Infect. 2022, 23, 34. Available online: https://www.journalofinfection.com/article/S0163-4453(22)00479-0/fulltext (accessed on 6 October 2022). [CrossRef] [PubMed]
- Champion, V.L.; Skinner, C.S. The health belief model. Health Behav. Health Educ. Theory Res. Pract. 2008, 4, 45–65. [Google Scholar]
- Wong, M.C.S.; Wong, E.L.Y.; Huang, J.; Cheung, A.W.L.; Law, K.; Chong, M.K.C.; Ng, R.W.Y.; Lai, C.K.C.; Boon, S.; Lau, J.T.F.; et al. Acceptance of the COVID-19 vaccine based on the health belief model: A population-based survey in Hong Kong. Vaccine 2021, 39, 1148–1156. [Google Scholar] [CrossRef] [PubMed]
- Caserotti, M.; Girardi, P.; Rubaltelli, E.; Tasso, A.; Lotto, L.; Gavaruzzi, T. Associations of COVID-19 risk perception with vaccine hesitancy over time for Italian residents. Soc. Sci. Med. 2021, 272, 113688. [Google Scholar] [CrossRef]
- Gerend, M.A.; Shepherd, J.E. Predicting human papillomavirus vaccine uptake in young adult women: Comparing the health belief model and theory of planned behavior. Ann. Behav. Med. 2012, 44, 171–180. [Google Scholar] [CrossRef] [PubMed]
- Simões, P.; Bhagani, S. A viewpoint: The 2022 monkeypox outbreak. J. Virus Erad. 2022, 8, 100078. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; apos Abreu de Paulo, K.J.I.; Gültzow, T.; Zimmermann, H.M.L.; Jonas, K.J. Monkeypox self-diagnosis abilities, determinants of vaccination and self-isolation intention after diagnosis among MSM, The Netherlands, July 2022. Eurosurveillance 2022, 27, 2200603. [Google Scholar] [CrossRef]
- Downing, M.J., Jr. Perceived likelihood of HIV and sexually transmitted infection acquisition among men who have sex with men. J. Assoc. Nurses AIDS Care 2014, 25, 98–102. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Balán, I.C.; Lopez-Rios, J.; Dolezal, C.; Rael, C.T.; Lentz, C. Low sexually transmissible infection knowledge, risk perception and concern about infection among men who have sex with men and transgender women at high risk of infection. Sex. Health 2019, 16, 580–586. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; d’Abreu de Paulo, K.J.I.; Gültzow, T.; Zimmermann, H.M.L.; Jonas, K.J. Brief report: Determinants of potential sexual activity reduction in the face of the Monkeypox epidemic. medRxiv 2022. Available online: https://www.medrxiv.org/content/10.1101/2022.08.01.22278287v1 (accessed on 6 October 2022).
- World Health Orgnization. Perceptions of Monkeypox from Those Most at Risk: Men Who Have Sex with Men Having Multiple Sexual Partners. 2022. Available online: https://www.who.int/europe/news/item/26-08-2022-perceptions-of-monkeypox-from-those-most-at-risk--men-who-have-sex-with-men-having-multiple-sexual-partners (accessed on 6 October 2022).
- Van Dijk, M.D.W.J.; Guadamuz, T.; Martinez, J.E.; Jonas, K. Quality of Sex Life and Perceived Sexual Pleasure of PrEP Users in The Netherlands. J. Sex Res. 2020, 59, 303–308. Available online: https://www.tandfonline.com/doi/full/10.1080/00224499.2021.1931653 (accessed on 6 October 2022). [CrossRef] [PubMed]
- Wang, H.; Shobowale, O.; Daas, C.D.; de Coul, E.O.; Bakker, B.; Radyowijati, A.; Vermey, K.; van Bijnen, A.; Zuilhof, W.; Jonas, K.J. Determinants of PrEP Uptake, Intention and Awareness in The Netherlands: A Socio-Spatial Analysis. Int. J. Environ. Res. Public Health 2022, 19, 8829. [Google Scholar] [CrossRef] [PubMed]
- Davido, B.; D’Anglejan, E.; Baudoin, R.; Dahmane, L.; Chaud, A.; Cortier, M.; Fellous, C.V.; De Truchis, P.; Ghosn, J. Monkeypox outbreak 2022: An unusual case of peritonsillar abscess in a person previously vaccinated against smallpox. J. Travel Med. 2022, 29, taac082. [Google Scholar] [CrossRef]
- Bragazzi, N.L.; Kong, J.D.; Mahroum, N.; Tsigalou, C.; Khamisy-Farah, R.; Converti, M.; Wu, J. Epidemiological trends and clinical features of the ongoing monkeypox epidemic: A preliminary pooled data analysis and literature review. J. Med. Virol. 2022, 1–8. [Google Scholar] [CrossRef]
- Center for Disease Control and Prevention. Clinical Considerations for Treatment and Prophylaxis of Monkeypox Virus Infection in People with HIV; CDC: New York, NY, USA, 2022. Available online: https://www.cdc.gov/poxvirus/monkeypox/clinicians/people-with-HIV.html (accessed on 6 October 2022).
- Ferrer, R.; Klein, W.M. Risk perceptions and health behavior. Curr. Opin. Psychol. 2015, 5, 85–89. [Google Scholar] [CrossRef]
- Hoornenborg, E. PrEP in The Netherlands the Introduction of HIV Pre-Exposure Prophylaxis; University of Amsterdam: Amsterdam, The Netherlands, 2020. [Google Scholar]
- Zimmermann, H.M.; Jongen, V.W.; Boyd, A.; Hoornenborg, E.; Prins, M.; De Vries, H.J.; Van Der Loeff, M.F.S.; Davidovich, U. Decision-making regarding condom use among daily and event-driven users of preexposure prophylaxis in The Netherlands. AIDS 2020, 34, 2295–2304. [Google Scholar] [CrossRef] [PubMed]
- Kalichman, S.C.; Cherry, C.; Kalichman, M.O.; Washington, C.; Grebler, T.; Hoyt, G.; Merely, C.; Welles, B. Sexual Behaviors and Transmission Risks Among People Living with HIV: Beliefs, Perceptions, and Challenges to Using Treatments as Prevention. Arch. Sex Behav. 2015, 45, 1421–1430. [Google Scholar] [CrossRef] [PubMed]
- Bourne, A.; Reid, D.; Hickson, F.; Torres-Rueda, S.; Weatherburn, P. Illicit drug use in sexual settings (‘chemsex’) and HIV/STI transmission risk behaviour among gay men in South London: Findings from a qualitative study: Table 1. Sex Transm. Infect. 2015, 91, 564–568. [Google Scholar] [CrossRef]
| Variables | Total Sample (n = 394) | |||
|---|---|---|---|---|
| N | % | |||
| Socio-demographic determinants | Age | |||
| <45 years | 171 | 43.4 | ||
| >45 years | 223 | 56.6 | ||
| Relationship | ||||
| Single | 79 | 20.05 | ||
| Single but dating | 91 | 23.1 | ||
| Monogamous relationship | 35 | 8.88 | ||
| Open/Polyamorous relationship | 189 | 47.97 | ||
| Education | ||||
| Lower than Bachelor | 89 | 22.65 | ||
| Bachelor | 131 | 33.33 | ||
| Master | 142 | 36.13 | ||
| PhD or higher | 31 | 7.89 | ||
| Employment | ||||
| Employed | 335 | 85.03 | ||
| Unemployed or receiving social welfare | 22 | 5.58 | ||
| Retired | 20 | 5.08 | ||
| Student | 17 | 4.31 | ||
| Migration status | ||||
| No migration status | 325 | 82.91 | ||
| First-generation migrant | 51 | 13.01 | ||
| Second-generation migrant | 16 | 4.08 | ||
| Residence | ||||
| The rest of the country | 154 | 39.10 | ||
| Randstad (main urban area) | 240 | 60.90 | ||
| Behavioural and Health determinants | Number of sexual partners in the previous 6 months | |||
| None | 8 | 2.03 | ||
| 1 | 46 | 11.68 | ||
| 2 to 6 | 82 | 20.81 | ||
| 7 to 15 | 159 | 40.36 | ||
| More than 15 | 99 | 25.13 | ||
| HIV status | ||||
| HIV-negative | 363 | 92.13 | ||
| HIV-positive | 22 | 5.58 | ||
| HIV status unknown or not disclosed | 9 | 2.28 | ||
| PrEP-use status | ||||
| Current PrEP users | 241 | 66.39 | ||
| PrEP-naïve or PrEP-discontinued | 122 | 30.96 | ||
| Any type of substance use in the previous 6 months | ||||
| Never | 45 | 11.42 | ||
| Ever | 349 | 88.58 | ||
| Recreational drugs use in the previous 6 months 1 | ||||
| Never | 250 | 63.45 | ||
| Ever | 144 | 36.55 | ||
| Chemsex in the previous 6 months 2 | ||||
| Never | 293 | 74.37 | ||
| Ever | 101 | 25.63 | ||
| Poppers use in the previous 6 months | ||||
| Never | 183 | 46.45 | ||
| Ever | 211 | 53.55 | ||
| Erectile dysfunction medication use in the previous 6 months 3 | ||||
| Never | 228 | 57.87 | ||
| Ever | 166 | 42.13 | ||
| Alcohol use in the previous 6 months | ||||
| Never | 93 | 23.6 | ||
| Ever | 301 | 76.4 | ||
| Visited a gay sauna in the previous 6 months | ||||
| Never | 251 | 63.71 | ||
| Ever | 143 | 36.29 | ||
| Visited a darkroom in the previous 6 months | ||||
| Never | 238 | 60.41 | ||
| Ever | 156 | 39.59 | ||
| Visited a circuit party in the previous 6 months | ||||
| Never | 283 | 71.83 | ||
| Ever | 111 | 28.17 | ||
| Visited a Pride event in the previous 6 months | ||||
| Never | 203 | 51.52 | ||
| Ever | 191 | 48.48 | ||
| Visited a gay dance club in the previous 6 months | ||||
| Never | 137 | 34.77 | ||
| Ever | 257 | 65.23 | ||
| Attended private sex parties in the previous 6 months | ||||
| Never | 277 | 70.3 | ||
| Ever | 117 | 29.7 | ||
| Visited fetish events/fairs in the previous 6 months | ||||
| Never | 308 | 78.17 | ||
| Ever | 86 | 21.83 | ||
| Psycho-social determinants | Knowing anybody who has/had monkeypox | |||
| No | 326 | 82.74 | ||
| Yes | 68 | 17.26 | ||
| Perceived problematic consequences of monkeypox * | 4 | [3,4] | ||
| Sub-Population | Perceived Monkeypox Concern (High/Very High vs. Rest of Scale) * | Perceived Monkeypox Risk (High/Very High vs. Rest of Scale) * | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | Prevalence (%) | 95%CI | SPR | 95%CI | n | Prevalence (%) | 95%CI | SPR | 95%CI | |
| Total sample (N = 394) | 205 | 52.03 | 47.10–56.92 | NA | NA | 120 | 30.46 | 26.12–35.17 | NA | NA |
| PrEP users (N = 241) | 113 | 46.89 | 40.69–53.19 | 0.83 | 0.68–0.99 | 74 | 30.71 | 25.22–36.79 | 1.09 | 0.86–1.36 |
| Non-PrEP users (N = 122) | 72 | 59.02 | 50.14–67.34 | 1.05 | 0.82–1.30 | 28 | 22.95 | 16.38–21.16 | 0.82 | 0.54–1.15 |
| HIV positive (N = 22) | 15 | 68.18 | 47.31–83.63 | 1.31 | 0.73–2.05 | 14 | 63.64 | 42.95–80.27 | 2.09 | 1.14–3.32 |
| HIV negative (N = 363) | 185 | 50.96 | 45.84–56.07 | 0.98 | 0.84–1.13 | 102 | 28.10 | 23.72–32.93 | 0.92 | 0.75–1.11 |
| HIV status unknown/undisclosed (N = 9) | 5 | 55.56 | 26.67–81.12 | 1.06 | 0.34–2.21 | 4 | 44.44 | 18.88–73.33 | 1.45 | 0.38–3.23 |
| Variables | Perceived Monkeypox Concern (High and Very High vs. Rest of Scale) ** | Perceived Monkeypox Risk (High and Very High vs. Rest of Scale) ** | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Univariable Model | Multivariable Model | Univariable Model | Multivariable Model | |||||||||||
| OR | 95%CI | p-Value | aOR | 95%CI | p-Value | OR | 95%CI | p-Value | aOR | 95%CI | p-Value | |||
| Socio-demographic determinants | Age | |||||||||||||
| <45 years | ref. | – | – | ref. | – | – | ref. | – | – | |||||
| >45 years | 0.53 | 0.36–0.79 | 0.002 | 0.93 | 0.54–1.62 | 0.806 | 0.91 | 059–1.40 | 0.672 | |||||
| Relationship | ||||||||||||||
| Single | ref. | – | – | ref. | – | – | ||||||||
| Single but dating | 1.25 | 0.68–2.29 | 0.486 | 0.99 | 0.50–1.96 | 0.975 | ||||||||
| Monogamous relationship | 0.86 | 0.39–1.92 | 0.719 | 0.69 | 0.26–1.81 | 0.453 | ||||||||
| Open/Polyamorous relationship | 1.15 | 0.68–1.95 | 0.597 | 1.55 | 0.87–2.77 | 0.138 | ||||||||
| Education | ||||||||||||||
| Lower than Bachelor | ref. | – | – | ref. | – | – | ref. | – | – | |||||
| Bachelor | 1.41 | 0.82–2.42 | 0.219 | 1.37 | 0.67–2.78 | 0.387 | 0.88 | 0.49–1.57 | 0.658 | |||||
| Master | 1.68 | 0.99–2.87 | 0.056 | 1.81 | 0.89–3.68 | 0.103 | 0.81 | 0.46–1.44 | 0.476 | |||||
| PhD or higher | 2.44 | 1.05–5.69 | 0.039 | 1.73 | 0.60–4.98 | 0.309 | 1.31 | 0.56–3.05 | 0.536 | |||||
| Employment | ||||||||||||||
| Employed | ref. | – | – | ref. | – | – | ref. | – | – | |||||
| Unemployed or receiving social welfare | 0.61 | 0.23–1.64 | 0.328 | 0.83 | 0.23–3.03 | 0.775 | 0.46 | 0.13–1.64 | 0.234 | |||||
| Retired | 0.26 | 0.09–0.71 | 0.009 | 0.23 | 0.06–0.82 | 0.002 | 0.64 | 0.23–1.77 | 0.385 | |||||
| Student | 2.04 | 0.76–5.41 | 0.156 | 1.73 | 0.54–5.49 | 0.351 | 0.93 | 0.35–2.48 | 0.878 | |||||
| Migration status | ||||||||||||||
| No migration status | ref. | – | – | ref. | – | – | ||||||||
| First-generation migrant | 1.14 | 0.63–2.05 | 0.670 | 0.94 | 0.49–1.79 | 0.845 | ||||||||
| Second-generation migrant | 0.73 | 0.26–2.00 | 0.536 | 0.75 | 0.24–2.38 | 0.626 | ||||||||
| Place of residence | ||||||||||||||
| The rest of the Country | ref. | – | – | ref. | – | – | ref. | – | – | ref. | – | – | ||
| Randstad (main urban area) | 1.92 | 1.27–2.89 | 0.002 | 1.47 | 0.87–2.49 | 0.155 | 1.67 | 1.06–2.64 | 0.027 | 1.30 | 0.74–2.29 | 0.360 | ||
| Behavioural and health determinants | Number of sexual partners in the previous 6 months | |||||||||||||
| None | ref. | – | – | ref. | – | – | ||||||||
| 1 | 1.40 | 0.30–2.51 | 0.669 | 0.30 | 0.06–1.55 | 0.150 | ||||||||
| 2 to 6 | 1.77 | 0.41–7.67 | 0.443 | 0.60 | 0.14–2.61 | 0.495 | ||||||||
| 7 to 15 | 2.00 | 0.45–8.83 | 0.360 | 0.83 | 0.19–3.70 | 0.811 | ||||||||
| More than 15 | 2.03 | 0.45–9.05 | 0.355 | 1.24 | 0.27–5.54 | 0.777 | ||||||||
| HIV status | ||||||||||||||
| HIV negative | ref. | – | – | ref. | – | – | ref. | – | – | |||||
| HIV positive | 2.06 | 0.82–5.18 | 0.123 | 4.48 | 1.82–11.00 | 0.001 | 4.29 | 1.44–12.82 | 0.009 | |||||
| HIV status unknown or not disclosed | 1.20 | 0.31–4.55 | 0.786 | 2.04 | 0.53–7.78 | 0.292 | 6.07 | 1.24–29.79 | 0.026 | |||||
| PrEP-use status | ||||||||||||||
| Current PrEP users | ref. | – | – | ref. | – | – | ref. | – | – | |||||
| PrEP-naïve or PrEP-discontinued | 1.63 | 1.04–2.53 | 0.030 | 2.55 | 1.39–4.67 | 0.002 | 0.67 | 0.41–1.11 | 0.122 | |||||
| Any type of substance use in the previous 6 months | ||||||||||||||
| Never | ref. | – | – | ref. | – | – | ||||||||
| Ever | 1.60 | 0.85–3.02 | 0.149 | 1.16 | 0.60–2.25 | 0.565 | ||||||||
| Recreational drugs use in the previous 6 months 1 | ||||||||||||||
| Never | ref. | – | – | ref. | – | – | ref. | – | – | |||||
| Ever | 1.56 | 1.03–2.36 | 0.035 | 1.50 | 0.86–2.62 | 0.156 | 1.44 | 0.92–2.33 | 0.105 | |||||
| Chemsex in the previous 6 months 2 | ||||||||||||||
| Never | ref. | – | – | ref. | – | – | ref. | – | – | ref. | – | – | ||
| Ever | 0.63 | 0.40–0.99 | 0.0491 | 0.44 | 0.22–0.88 | 0.021 | 1.55 | 0.96–2.50 | 0.071 | 1.23 | 0.60–2.71 | 0.605 | ||
| Poppers in the previous 6 months | ||||||||||||||
| Never | ref. | – | – | ref. | – | – | ||||||||
| Ever | 1.01 | 0.68–1.50 | 0.965 | 1.39 | 0.90–2.14 | 0.140 | ||||||||
| Erectile dysfunction medication use | ||||||||||||||
| in the previous 6 months 3 | ||||||||||||||
| Never | ref. | – | – | ref. | – | – | ref. | – | – | ref. | – | – | ||
| Ever | 0.70 | 0.47–1.05 | 0.088 | 1.16 | 0.63–2.15 | 0.625 | 0.98–2.32 | 0.47–1.05 | 0.062 | 1.25 | 0.67–2.34 | 0.479 | ||
| Alcohol use in the previous 6 months | ||||||||||||||
| Never | ref. | – | – | ref. | – | – | ||||||||
| Ever | 0.97 | 0.61–1.54 | 0.885 | 0.79 | 0.48–0.79 | 0.344 | ||||||||
| Visited a gay sauna in the previous 6 months | ||||||||||||||
| Never | ref. | – | – | ref. | – | – | ref. | – | – | |||||
| Ever | 1.28 | 0.84–1.93 | 0.241 | 1.28 | 0.68–2.41 | 0.439 | 1.28 | 0.68–2.41 | 0.439 | |||||
| Visited a darkroom in the previous 6 months | ||||||||||||||
| Never | ref. | – | – | ref. | – | – | ref. | – | – | |||||
| Ever | 1.08 | 0.72–1.62 | 0.706 | 1.43 | 0.74–2.76 | 0.294 | 1.43 | 0.74–2.76 | 0.294 | |||||
| Visited a circuit party in the previous 6 months | ||||||||||||||
| Never | ref. | – | – | ref. | – | – | ref. | – | – | |||||
| Ever | 1.06 | 0.69–1.65 | 0.780 | 0.89 | 0.44–0.81 | 0.749 | 0.89 | 0.44–0.81 | 0.749 | |||||
| Visited a Pride event in the previous 6 months | ||||||||||||||
| Never | ref. | – | – | |||||||||||
| Ever | 1.11 | 0.75–1.65 | 0.597 | |||||||||||
| Visited a gay dance club in the previous 6 months | ||||||||||||||
| Never | ref. | – | – | |||||||||||
| Ever | 1.16 | 0.76–1.75 | 0.487 | |||||||||||
| Attended private sex parties in the previous 6 months | ||||||||||||||
| Never | ref. | – | – | ref. | – | – | ref. | – | – | |||||
| Ever | 0.87 | 0.56–1.34 | 0.526 | 2.10 | 1.04–4.24 | 0.037 | 2.10 | 1.04–4.24 | 0.037 | |||||
| Visited fetish events/fairs in the previous 6 months | ||||||||||||||
| Never | ref. | – | – | ref. | – | – | ||||||||
| Ever | 1.08 | 0.67–1.74 | 0.760 | 1.39 | 0.84–2.29 | 0.204 | ||||||||
| Psycho-social determinants | Knowing anybody who has/had monkeypox | |||||||||||||
| No | ref. | – | – | ref. | – | – | ref. | – | – | ref. | – | – | ||
| Yes | 2.81 | 1.59–4.98 | <0.001 | 1.58 | 0.76–3.27 | 0.218 | 3.77 | 2.20–6.47 | <0.001 | 2.60 | 1.33–5.07 | 0.005 | ||
| Perceived problematic consequences of monkeypox * | 1.18 | 0.96-1.45 | 0.101 | 1.07 | 0.86–1.33 | 0.560 | ||||||||
| Perceived concern about monkeypox infection * | NA | NA | NA | NA | NA | NA | 3.13 | 2.36–4.13 | <0.001 | 3.24 | 2.40–4.38 | <0.001 | ||
| Perceived risk of monkeypox infection * | 2.97 | 2.31-3.82 | <0.001 | 3.26 | 0.81–1.36 | <0.001 | NA | NA | NA | NA | NA | NA | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, H.; d’Abreu de Paulo, K.J.I.; Gültzow, T.; Zimmermann, H.M.L.; Jonas, K.J. Perceived Monkeypox Concern and Risk among Men Who Have Sex with Men: Evidence and Perspectives from The Netherlands. Trop. Med. Infect. Dis. 2022, 7, 293. https://doi.org/10.3390/tropicalmed7100293
Wang H, d’Abreu de Paulo KJI, Gültzow T, Zimmermann HML, Jonas KJ. Perceived Monkeypox Concern and Risk among Men Who Have Sex with Men: Evidence and Perspectives from The Netherlands. Tropical Medicine and Infectious Disease. 2022; 7(10):293. https://doi.org/10.3390/tropicalmed7100293
Chicago/Turabian StyleWang, Haoyi, Kennedy J. I. d’Abreu de Paulo, Thomas Gültzow, Hanne M. L. Zimmermann, and Kai J. Jonas. 2022. "Perceived Monkeypox Concern and Risk among Men Who Have Sex with Men: Evidence and Perspectives from The Netherlands" Tropical Medicine and Infectious Disease 7, no. 10: 293. https://doi.org/10.3390/tropicalmed7100293
APA StyleWang, H., d’Abreu de Paulo, K. J. I., Gültzow, T., Zimmermann, H. M. L., & Jonas, K. J. (2022). Perceived Monkeypox Concern and Risk among Men Who Have Sex with Men: Evidence and Perspectives from The Netherlands. Tropical Medicine and Infectious Disease, 7(10), 293. https://doi.org/10.3390/tropicalmed7100293








