Spatial and Temporal Patterns of Ross River Virus in Queensland, 2001–2020
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Area
2.2. Data Collection and Collation
2.3. Descriptive Analysis
3. Results
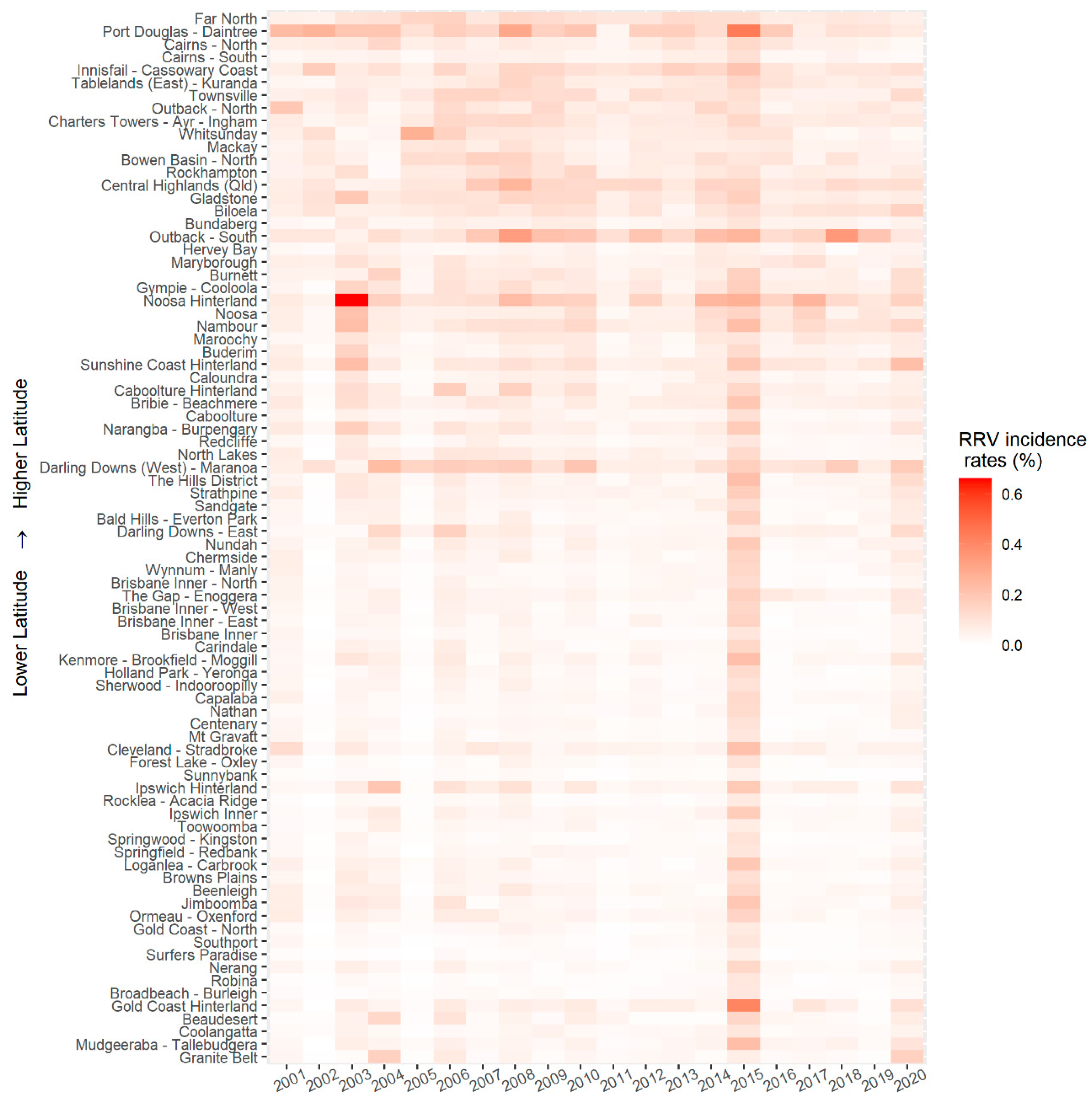
3.1. Temporal Trends
3.2. Spatial Patterns
3.3. Weather Conditions
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Liu, X.; Tharmarajah, K.; Taylor, A. Ross River virus disease clinical presentation, pathogenesis and current therapeutic strategies. Microbes Infect. 2017, 19, 496–504. [Google Scholar] [CrossRef]
- Australian Department of Health. National Notifiable Disease Surveillance System. 2021. Available online: http://www9.health.gov.au/cda/source/cda-index.cfm (accessed on 14 March 2021).
- Harley, D.; Ritchie, S.; Phillips, D.; Hurk, A.V.D. Mosquito isolates of Ross River virus from Cairns, Queensland, Australia. Am. J. Trop. Med. Hyg. 2000, 62, 561–565. [Google Scholar] [CrossRef] [Green Version]
- Harley, D.; Sleigh, A.; Ritchie, S. Ross River Virus Transmission, Infection, and Disease: A Cross-Disciplinary Review. Clin. Microbiol. Rev. 2001, 14, 909–932. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Qian, W.; Viennet, E.; Glass, K.; Harley, D. Epidemiological models for predicting Ross River virus in Australia: A systematic review. PLoS Negl. Trop. Dis. 2020, 14, e0008621. [Google Scholar] [CrossRef]
- Australian Government Department of Health. Notifiable Diseases Surveillance, 1917 to 1991. 2003. Available online: https://www1.health.gov.au/internet/main/publishing.nsf/Content/cda-pubs-annlrpt-oz_dis19_91.htm (accessed on 9 July 2021).
- Case Definitions Working Group. Revised surveillance case definitions: Barmah Forest virus infection, Ross River virus infection, congenital rubella infection. Commun Dis. Intell. 2015, 39, E599–E601. [Google Scholar]
- Australian Department of Health. Ross River Virus Infection Case Definition. 2016. Available online: https://www1.health.gov.au/internet/main/publishing.nsf/Content/cda-surveil-nndss-casedefs-cd_rrv.htm (accessed on 14 March 2021).
- Gatton, M.L.; Kelly-Hope, L.; Kay, B.H.; Ryan, P.A. Spatial-temporal analysis of ross river virus disease patterns in Queensland, Australia. Am. J. Trop. Med. Hyg. 2004, 71, 629–635. [Google Scholar] [CrossRef] [Green Version]
- Yu, W.; Mengersen, K.; Dale, P.; MacKenzie, J.S.; Toloo, G.; Wang, X.; Tong, S. Epidemiologic Patterns of Ross River Virus Disease in Queensland, Australia, 2001–2011. Am. J. Trop. Med. Hyg. 2014, 91, 109–118. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murphy, A.K.; Clennon, J.A.; Vazquez-Prokopec, G.; Jansen, C.C.; Frentiu, F.D.; Hafner, L.M.; Hu, W.; Devine, G.J. Spatial and temporal patterns of Ross River virus in south east Queensland, Australia: Identification of hot spots at the rural-urban interface. BMC Infect. Dis. 2020, 20, 722. [Google Scholar] [CrossRef] [PubMed]
- Bi, P.; Hiller, J.; Cameron, A.S.; Zhang, Y.; Givney, R. Climate variability and Ross River virus infections in Riverland, South Australia, 1992–2004. Epidemiol. Infect. 2009, 137, 1486–1493. [Google Scholar] [CrossRef] [Green Version]
- Ng, V.; Dear, K.; Harley, D.; McMichael, A. Analysis and Prediction of Ross River Virus Transmission in New South Wales, Australia. Vector-Borne Zoonotic Dis. 2014, 14, 422–438. [Google Scholar] [CrossRef]
- Woodruff, R.E.; Guest, C.S.; Garner, M.G.; Becker, N.; Lindsay, M. Early warning of Ross River virus epidemics: Combining surveillance data on climate and mosquitoes. Epidemiology 2006, 17, 569–575. [Google Scholar] [CrossRef] [PubMed]
- Tong, S.; Dale, P.; Nicholls, N.; MacKenzie, J.S.; Wolff, R.C.; McMichael, A.J. Climate Variability, Social and Environmental Factors, and Ross River Virus Transmission: Research Development and Future Research Needs. Environ. Health Perspect. 2008, 116, 1591–1597. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Queensland Government. Interesting Facts about Queensland. 2017. Available online: https://www.qld.gov.au/about/about-queensland/statistics-facts/facts (accessed on 18 May 2021).
- Australian Bureau of Statistics. National, State and Territory Population. 2021. Available online: https://www.abs.gov.au/statistics/people/population/national-state-and-territory-population/latest-release#states-and-territories (accessed on 14 March 2021).
- Queensland Government. Australian Statistical Geography Standard. 2019. Available online: https://www.qgso.qld.gov.au/about-statistics/statistical-standards-classifications/australian-statistical-geography-standard (accessed on 14 March 2021).
- Australian Building Codes Board. Climate Zone Map: Queensland. 2021. Available online: https://www.abcb.gov.au/Resources/Tools-Calculators/Climate-Zone-Map-Queensland (accessed on 14 March 2021).
- Climate-Data.org. Queensland Climate. 2021. Available online: https://en.climate-data.org/oceania/australia/queensland-899/ (accessed on 14 March 2021).
- Australia Government. The Australian Bureau of Statistics. 2019. Available online: http://www.abs.gov.au/ (accessed on 14 March 2021).
- Australian Bureau of Meteorology. Long-Range Weather and Climate. 2021. Available online: http://www.bom.gov.au/climate/ (accessed on 14 March 2021).
- R Core Team. A Language and Environment for Statistical Computing; R Core Team: Vienna, Austria, 2020. [Google Scholar]
- Environmental Systems Research Institute. ArcGIS Desktop; Environmental Systems Research Institute: Redlands, CA, USA, 2020. [Google Scholar]
- Knope, K.; Doggett, S.L.; Jansen, C.C.; Johansen, C.A.; Kurucz, N.; Feldman, R.; Lynch, S.E.; Hobby, M.P.; Sly, A.; Jardine, A.; et al. Arboviral diseases and malaria in Australia, 2014–15: Annual report of the National Arbovirus and Malaria Advisory Committee. Commun. Dis. Intell. 2019, 43, 1–69. [Google Scholar] [CrossRef]
- Selvey, L.; Donelly, J.; Lindsay, M.; Boddu, S.; D’Abrera, V.; Smith, D. Ross River virus infection surveillance in the Greater Perth Metropolitan area–has there been an increase in cases in the winter months? Natl. Cent. Biotechnol. Inf. 2014, 38, E114–E121. [Google Scholar]
- Jansen, C.C.; Shivas, M.A.; May, F.J.; Pyke, A.; Onn, M.B.; Lodo, K.; Hall-Mendelin, S.; McMahon, J.L.; Montgomery, B.L.; Darbro, J.M.; et al. Epidemiologic, Entomologic, and Virologic Factors of the 2014–15 Ross River Virus Outbreak, Queensland, Australia. Emerg. Infect. Dis. 2019, 25, 2243–2252. [Google Scholar] [CrossRef] [Green Version]
- Ewing, D.; Cobbold, C.; Purse, B.; Nunn, M.; White, S. Modelling the effect of temperature on the seasonal population dynamics of temperate mosquitoes. J. Theor. Biol. 2016, 400, 65–79. [Google Scholar] [CrossRef] [Green Version]
- Tomerini, D.M. The Impact of Local Government Mosquito Control Programs on Ross River Virus Disease in Queensland, Australia. Ph.D. Thesis, Griffith University, Brisbane, Austrilia, 2008. [Google Scholar]
- Tomerini, D.M.; Dale, P.; Sipe, N. Does Mosquito Control Have an Effect on Mosquito-Borne Disease? The Case of Ross River Virus Disease and Mosquito Management in Queensland, Australia. J. Am. Mosq. Control Assoc. 2011, 27, 39–44. [Google Scholar] [CrossRef]
- Queensland Government. Queensland Land Use Mapping Program (QLUMP). 2021. Available online: https://www.qld.gov.au/environment/land/management/mapping/statewide-monitoring/qlump (accessed on 22 March 2021).
- Aaskov, J.G.; Mataika, J.U.; Lawrence, G.W.; Rabukawaqa, V.; Tucker, M.M.; Miles, J.A.R.; Dalglish, D.A. An Epidemic of Ross River Virus Infection in Fiji, 1979. Am. J. Trop. Med. Hyg. 1981, 30, 1053–1059. [Google Scholar] [CrossRef]
- Werner, A.K.; Goater, S.; Carver, S.; Robertson, G.; Allen, G.R.; Weinstein, P. Environmental drivers of Ross River virus in southeastern Tasmania, Australia: Towards strengthening public health interventions. Epidemiol. Infect. 2011, 140, 359–371. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Queensland Government. Ross River Virus Fact Sheet. 2017. Available online: http://conditions.health.qld.gov.au/HealthCondition/condition/14/217/120/ross-river-virus (accessed on 14 March 2021).
- Gatton, M.L.; Ryan, P.A.; Kay, B.H. Environmental predictors of ross river virus disease outbreaks in Queensland, Australia. Am. J. Trop. Med. Hyg. 2005, 72, 792–799. [Google Scholar] [CrossRef]
- Stephenson, E.B.; Peel, A.J.; Reid, S.A.; Jansen, C.C.; McCallum, H. The non-human reservoirs of Ross River virus: A systematic review of the evidence. Parasites Vectors 2018, 11, 188. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jacups, S.; Kurucz, N.; Whelan, P.I.; Carter, J. A comparison of Aedes vigilax larval population densities and associated vegetation categories in a coastal wetland, Northern Territory, Australia. J. Vector Ecol. 2009, 34, 311–316. [Google Scholar] [CrossRef] [PubMed]



| SA2 * Areas with High Numbers of Cases | SA2 Areas with High Incidence Rates | SA2 Areas with Low Numbers of Cases or Low Incidence Rates | Other SA2 Areas | |||||
|---|---|---|---|---|---|---|---|---|
| Coastal Areas | Non-coastal | Coastal | Non-coastal | Coastal | Non-coastal | Coastal | Non-coastal | Coastal |
| Number of SA2 areas | 17 | 36 | 15 | 38 | 29 | 37 | 223 | 160 |
| Average total cases per SA2 | 242.5 | 267.1 | 191.0 | 202.3 | 12.2 | 8.9 | 66.1 | 82.7 |
| Average cumulative incidence per SA2 (per a population of 10,000) | 223.2 | 291.8 | 284.5 | 391.8 | 13.9 | 85.9 | 79.2 | 122.3 |
| Average daily temperature maxima and minima through seasons **, ℃, | ||||||||
| Spring | (28.0, 14.3) | (28.3, 17.6) | (30.0, 15.3) | (29.5, 18.4) | (26.5, 14.0) | (27.6, 17.3) | (27.1, 14.7) | (27.8, 17.3) |
| Summer | (31.2, 19.9) | (30.8, 22.1) | (33.7, 21.3) | (31.6, 22.7) | (29.6, 19.4) | (30.3, 21.8) | (30.2, 20.1) | (30.4, 21.9) |
| Autumn | (26.7, 14.8) | (27.7, 18.4) | (28.3, 15.2) | (28.5, 19.0) | (25.7, 14.7) | (27.2, 18.1) | (26.3, 15.4) | (27.3, 18.2) |
| Winter | (21.5, 8.0) | (23.6, 12.5) | (22.2, 7.8) | (24.6, 13.1) | (20.9, 8.1) | (23.1, 12.3) | (21.9, 8.9) | (23.2, 12.3) |
| Average daily rainfall, mm, mean (SD) | ||||||||
| Spring | 1.9 (6.1) | 1.9 (6.9) | 1.4 (4.6) | 1.6 (6.0) | 2.2 (7.2) | 2.0 (7.7) | 2.1 (7.0) | 2.1 (7.7) |
| Summer | 4.3 (11.8) | 6.9 (18.2) | 3.3 (8.7) | 7.1 (17.9) | 4.5 (13.4) | 6.7 (18.4) | 4.5 (13.1) | 6.9 (18.3) |
| Autumn | 2.5 (8.7) | 4.2 (12.9) | 1.9 (6.7) | 3.9 (12.2) | 2.6 (9.7) | 3.9 (12.4) | 2.6 (10.1) | 4.5 (13.7) |
| Winter | 1.3 (5.4) | 1.6 (6.4) | 1.0 (4.2) | 1.3 (5.5) | 1.4 (5.8) | 1.6 (7.0) | 1.4 (5.9) | 1.7 (6.9) |
| Average days having rainfall > 0 mm/>15 mm in a year | ||||||||
| Spring | 777/68 | 677/67 | 782/46 | 692/52 | 594/79 | 591/68 | 643/76 | 644/69 |
| Summer | 1052/147 | 1085/224 | 1110/108 | 1184/230 | 826/155 | 977/217 | 886/155 | 1028/224 |
| Autumn | 951/78 | 1007/130 | 851/59 | 1009/122 | 751/77 | 880/123 | 811/75 | 956/134 |
| Winter | 724/40 | 676/48 | 683/31 | 633/40 | 507/44 | 553/51 | 554/43 | 624/53 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Qian, W.; Hurst, C.; Glass, K.; Harley, D.; Viennet, E. Spatial and Temporal Patterns of Ross River Virus in Queensland, 2001–2020. Trop. Med. Infect. Dis. 2021, 6, 145. https://doi.org/10.3390/tropicalmed6030145
Qian W, Hurst C, Glass K, Harley D, Viennet E. Spatial and Temporal Patterns of Ross River Virus in Queensland, 2001–2020. Tropical Medicine and Infectious Disease. 2021; 6(3):145. https://doi.org/10.3390/tropicalmed6030145
Chicago/Turabian StyleQian, Wei, Cameron Hurst, Kathryn Glass, David Harley, and Elvina Viennet. 2021. "Spatial and Temporal Patterns of Ross River Virus in Queensland, 2001–2020" Tropical Medicine and Infectious Disease 6, no. 3: 145. https://doi.org/10.3390/tropicalmed6030145
APA StyleQian, W., Hurst, C., Glass, K., Harley, D., & Viennet, E. (2021). Spatial and Temporal Patterns of Ross River Virus in Queensland, 2001–2020. Tropical Medicine and Infectious Disease, 6(3), 145. https://doi.org/10.3390/tropicalmed6030145








