Estimation of Potential HIV Transmission Risk in Recent Anal Intercourse Events among Men Who Have Sex with Men and Transgender Women in Bali, Indonesia
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- UNAIDS. Indonesia Country Data 2018; UNAIDS: Jakarta, Indonesia, 2018. [Google Scholar]
- Republic of Indonesia Ministry of Health. Integrated Biological and Behavioral Survey 2018–2019; Republic of Indonesia Ministry of Health: Jakarta, Indonesia, 2019.
- Republic of Indonesia Ministry of Health. HIV Epidemiology Review: Indonesia 2016; Republic of Indonesia Ministry of Health: Jakarta, Indonesia, 2017.
- Januraga, P.P.; Reekie, J.; Mulyani, T.; Lestari, B.W.; Iskandar, S.; Wisaksana, R.; Kusmayanti, N.A.; Subronto, Y.W.; Widyanthini, D.N.; Wirawan, D.N.; et al. The cascade of HIV care among key populations in Indonesia: A prospective cohort study. Lancet HIV 2018, 5, e560–e568. [Google Scholar] [CrossRef] [Green Version]
- Cempaka, R.; Wardhani, B.; Sawitri, A.A.S.; Januraga, P.P.; Bavinton, B.R. PrEP use, awareness and interest cascade among MSM and transgender women living in Bali, Indonesia. Trop. Med. Infect. Dis. 2020, 5, 158–169. [Google Scholar] [CrossRef] [PubMed]
- Bavinton, B.R. Scoping Paper: Where to from Here? Identifying Gaps in Social Research for Future Development of Strategic Information; Asia-Pacific Coalition on Male Sexual Health (APCOM): Bangkok, Thailand, 2013. [Google Scholar]
- Safika, I.; Johnson, T.P.; Cho, Y.I.; Praptoraharjo, I. Condom use among men who have sex with men and male-to-female transgenders in Jakarta, Indonesia. Am. J. Men’s Health 2014, 8, 278–288. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Prasetyo, A.A.; Ariapramuda, R.; Kindi, E.A.; Dirgahayu, P.; Sari, Y.; Dharmawan, R.; Kageyama, S. Men having sex with men in Surakarta, Indonesia: Demographics, behavioral characteristics and prevalence of blood borne pathogens. SE Asian J. Trop. Med. 2014, 45, 1032. [Google Scholar]
- Morineau, G.; Nugrahini, N.; Riono, P.; Girault, P.; Mustikawati, D.E.; Magnani, R. Sexual risk taking, STI and HIV prevalence among men who have sex with men in six Indonesian cities. AIDS Behav. 2011, 15, 1033–1044. [Google Scholar] [CrossRef] [PubMed]
- Zablotska, I.B.; Kippax, S.C.; Grulich, A.E.; Holt, M.; Prestage, G.P. Behavioural surveillance among gay men in Australia: Methods, findings and policy implications for the prevention of HIV and other sexually transmissible infections. Sex. Health 2011, 8, 272–279. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, Y.; Yu, B.; Jia, P.; Wang, Z.; Yang, S.; Tian, C.; Lai, W.; Yang, S.; Qian, H.Z. Association between psychological factors and condom use with regular and nonregular male sexual partners among Chinese MSM: A quantitative study based on the Health Belief Model. BioMed Res. Int. 2020, 2020, 5807162. [Google Scholar] [CrossRef] [PubMed]
- Hill, A.O.; Bavinton, B.R.; Armstrong, G. Prevalence and factors associated with inconsistent condom use among men who have sex with men (MSM) who use mobile geo-social networking applications in Greater Tokyo. Int. J. Environ. Res. Public Health 2018, 15, 2815. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lim, S.H.; Bazazi, A.R.; Sim, C.; Choo, M.; Altice, F.L.; Kamarulzaman, A. High rates of unprotected anal intercourse with regular and casual partners and associated risk factors in a sample of ethnic Malay men who have sex with men (MSM) in Penang, Malaysia. Sex. Transm. Infect. 2013, 89, 642–649. [Google Scholar] [CrossRef] [PubMed]
- Down, I.; Ellard, J.; Bavinton, B.R.; Brown, G.; Prestage, G.P. In Australia, most HIV infections among gay and bisexual men are attributable to sex with ‘new’partners. AIDS Behav. 2017, 21, 2543–2550. [Google Scholar] [CrossRef] [PubMed]
- Jin, F.; Crawford, J.; Prestage, G.; Zablotska, I.; Imrie, J.; Kippax, S.C.; Kaldor, J.M.; Grulich, A.E. Unprotected anal intercourse, risk reduction behaviours, and subsequent HIV infection in a cohort of homosexual men. AIDS 2009, 23, 243–252. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bavinton, B.R.; Prestage, G.; Jin, F.; Phanuphak, N.; Grinsztejn, B.; Fairley, C.K.; Baker, D.; Hoy, J.; Templeton, D.J.; Tee, B.K.; et al. Strategies used by gay male HIV serodiscordant couples to reduce the risk of HIV transmission from anal intercourse in three countries. J. Int. AIDS Soc. 2019, 22, e25277. [Google Scholar] [CrossRef] [PubMed]
- Gedela, K.; Wirawan, D.N.; Wignall, F.S.; Luis, H.; Merati, T.P.; Sukmaningrum, E.; Irwanto, I. Getting Indonesia’s HIV epidemic to zero? One size does not fit all. Int. J. STD AIDS 2021, 32, 290–299. [Google Scholar] [CrossRef] [PubMed]
- Melendez-Torres, G.; Bourne, A. Illicit drug use and its association with sexual risk behaviour among MSM: More questions than answers? Curr. Opin. Infect. Dis. 2016, 29, 58–63. [Google Scholar] [CrossRef] [PubMed]
- Thienkrua, W.; Van Griensven, F.; Mock, P.A.; Dunne, E.F.; Raengsakulrach, B.; Wimonsate, W.; Howteerakul, N.; Ungsedhapand, C.; Chiwarakorn, A.; Holtz, T.H. Young men who have sex with men at high risk for HIV, Bangkok MSM Cohort Study, Thailand 2006–2014. AIDS Behav. 2018, 22, 2137–2146. [Google Scholar] [CrossRef] [PubMed]
- Bavinton, B.R.; Grulich, A.E.; Broady, T.; Keen, P.; Mao, L.; Patel, P.; Chan, C.; Prestage, G.; Holt, M. Increases in HIV testing frequency in Australian gay and bisexual men are concentrated among PrEP users: An analysis of Australian behavioural surveillance data, 2013–2018. AIDS Behav. 2020, 24, 2691–2702. [Google Scholar] [CrossRef] [PubMed]
- Keen, P.; Hammoud, M.A.; Bourne, A.; Bavinton, B.R.; Holt, M.; Vaccher, S.; Haire, B.; Saxton, P.; Jin, F.; Maher, L.; et al. Use of HIV pre-exposure prophylaxis (PrEP) associated with lower HIV anxiety among gay and bisexual men in Australia who are at high risk of HIV infection: Results from the Flux Study. J. Acq. Immun. Def. Synd. 2020, 83, 119–125. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Xue, L.; Tucker, J.D.; Wei, C.; Durvasula, M.; Hu, W.; Kang, D.; Liao, M.; Tang, W.; Ma, W. Condom use peer norms and self-efficacy as mediators between community engagement and condom use among Chinese men who have sex with men. BMC Public Health 2017, 17, 641. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Review of the National Health Sector Response to HIV in the Republic of Indonesia; World Health Organization: Jakarta, Indonesia, 2017. [Google Scholar]
- Bavinton, B.R.; Hill, A.O.; Amos, N.; Lim, S.H.; Guadamuz, T.; Kaneko, N.; Holt, M.; Bourne, A. Low PrEP uptake among gay, bisexual, and other men who have sex with men in five Asian countries: Results of the Asia-Pacific MSM Internet Survey. In Proceedings of the 11th International AIDS Society Conference on HIV Science, Berlin, Germany, 18–21 July 2021. [Google Scholar]
- Holt, M.; Broady, T.R.; Mao, L.; Chan, C.; Rule, J.; Ellard, J.; O’Donnell, D.; Grulich, A.E.; Prestage, G.; Bavinton, B.R. Increasing pre-exposure prophylaxis use and “net prevention coverage” in behavioural surveillance of Australian gay and bisexual men. AIDS 2021, 35, 835–840. [Google Scholar] [CrossRef] [PubMed]
- Bavinton, B.R.; Grulich, A.E. HIV pre-exposure prophylaxis: Scaling up for impact now and in the future. Lancet HIV 2021, 6, e528–e533. [Google Scholar]
| Total Sample (n = 709) | Born in Bali (n = 239) | Born Outside Bali (n = 470) | p-Value | |
|---|---|---|---|---|
| Location of birth | NA | |||
| Bali | 239 (33.7) | 239 (100.0) | 0 (0.0%) | |
| Java | 290 (40.9) | 0 (0.0%) | 290 (61.7) | |
| Other | 180 (25.4) | 0 (0.0%) | 180 (38.3) | |
| Age—median (IQR) | 27 (24–31) | 26 (23–31) | 28 (24–31) | 0.012 |
| Strength of identification with: | ||||
| ‘Gay’ identity 1—mean (SD) | 1.94 (1.01) | 1.78 (1.09) | 2.01 (0.96) | 0.006 |
| ‘Heterosexual’ identity 1—mean (SD) | 0.75 (0.90) | 0.97 (1.00) | 0.64 (0.84) | <0.001 |
| Gender identity | <0.001 | |||
| Male | 653 (92.1) | 206 (86.2) | 447 (95.1) | |
| Waria, trans woman, or female | 56 (7.9) | 33 (13.8) | 23 (4.9) | |
| Education | 0.047 | |||
| Junior high school or less | 91 (12.9) | 25 (10.5) | 66 (14.1) | |
| Senior high school | 430 (60.7) | 138 (57.7) | 292 (62.3) | |
| University or diploma | 187 (26.4) | 76 (31.8) | 111 (23.7) | |
| Not reported | 1 | 0 | 1 | |
| Employment | <0.001 | |||
| Working | 615 (86.7) | 192 (80.3) | 423 (90.0) | |
| Studying | 28 (4.0) | 14 (5.9) | 14 (3.0) | |
| Not working | 50 (7.1) | 19 (8.0) | 31 (6.6) | |
| Other | 16 (2.3) | 14 (5.9) | 2 (0.4) | |
| Income per month | 0.011 | |||
| <2 million IDR | 204 (29.2) | 86 (36.3) | 118 (25.5) | |
| 2–3 million IDR | 217 (31.0) | 74 (31.2) | 143 (31.0) | |
| 3–5 million IDR | 215 (30.8) | 58 (24.5) | 157 (34.0) | |
| 5+ million IDR | 63 (9.0) | 19 (8.0) | 44 (9.5) | |
| Not reported | 10 | 2 | 8 | |
| Sex work in previous 6 months | 0.163 | |||
| No sex work | 510 (71.9) | 162 (67.8) | 348 (74.0) | |
| Incidental sex work | 120 (16.9) | 44 (18.4) | 76 (16.2) | |
| Sex work as main source of income | 79 (11.1) | 33 (13.8) | 46 (9.8) | |
| Recruited to the study by an outreach worker | 650 (91.7) | 223 (93.3) | 427 (90.9) | 0.091 |
| Contact with HIV outreach workers | ||||
| Face-to-face (previous 12 months) | 634 (89.4) | 212 (88.7) | 422 (89.8) | 0.657 |
| Online (previous 6 months) | 551 (77.7) | 186 (77.8) | 365 (77.7) | 0.960 |
| HIV testing | 0.001 | |||
| Never tested | 100 (14.1) | 49 (20.5) | 51 (10.9) | |
| Tested in previous 12 months | 507 (71.5) | 154 (64.4) | 353 (75.1) | |
| Tested more than 12 months ago | 102 (14.4) | 36 (15.1) | 66 (14.0) | |
| HIV status at last HIV test | 0.008 | |||
| HIV-positive | 106 (15.0) | 32 (13.4) | 74 (15.7) | |
| HIV-negative | 391 (55.1) | 125 (52.3) | 266 (56.6) | |
| Untested or did not collect result | 106 (15.0) | 51 (21.3) | 55 (11.7) | |
| Not reported | 106 (15.0) | 31 (13.0) | 75 (16.0) | |
| Sexual partners in the previous 6 months | ||||
| Any men | 613 (86.5) | 199 (83.3) | 414 (88.1) | 0.076 |
| Any waria | 67 (9.5) | 41 (17.2) | 26 (5.5) | <0.001 |
| Any women | 142 (20.0) | 74 (31.0) | 68 (14.5) | <0.001 |
| Met male/waria sex partners in the previous 6 months | ||||
| Gay mobile applications | 414 (58.4) | 125 (52.3) | 289 (61.5) | 0.019 |
| Social media | 401 (56.6) | 149 (62.3) | 252 (53.6) | 0.027 |
| Gay bar/club | 225 (31.7) | 60 (25.1) | 165 (35.1) | 0.007 |
| Other bar/club | 175 (24.7) | 56 (23.4) | 119 (25.3) | 0.581 |
| Gay sauna | 143 (20.2) | 32 (13.4) | 111 (23.6) | 0.001 |
| Public area | 188 (26.5) | 79 (33.1) | 109 (23.2) | 0.005 |
| Any use of alcohol in previous 6 months | 297 (41.9) | 89 (37.2) | 208 (44.3) | 0.073 |
| Any recreational drug use in previous 6 months 2 | 103 (14.5) | 39 (16.3) | 64 (13.6) | 0.335 |
| Any drug use for the purposes of sex in previous 6 months | 65 (9.2) | 25 (10.5) | 40 (8.5) | 0.395 |
| PrEP use in HIV-negative respondents 3 | 10 (2.6) | 4 (3.2) | 6 (2.3) | 0.581 |
| Antiretroviral therapy (ART) in HIV-positive respondents 4 | 99 (93.4) | 31 (96.9) | 68 (91.9) | 0.603 |
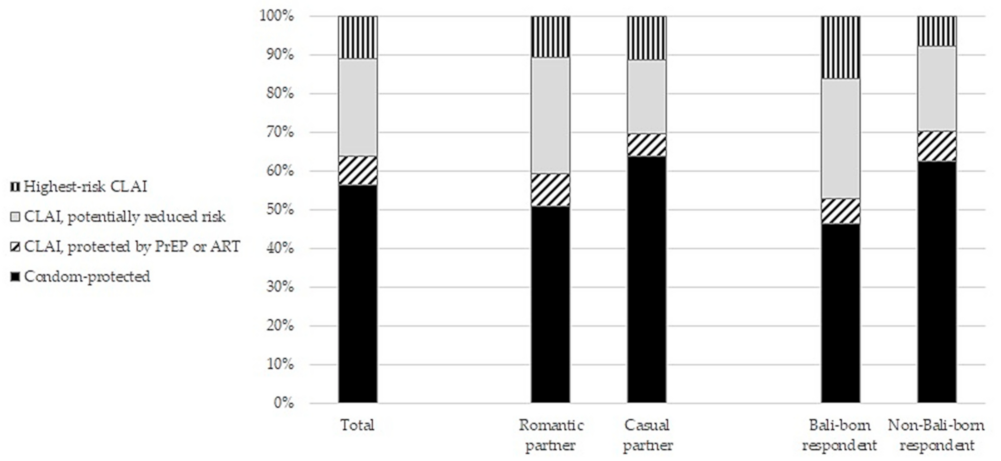
| Total (n = 703) | Romantic Partner (n = 397) | Casual Partner (n = 306) | p-Value for Partner Type Comparison | Bali-Born Respondent (n = 263) | Non-Bali-Born Respondent (n = 440) | p-Value for Place of Birth Comparison | |
|---|---|---|---|---|---|---|---|
| Condom use | 397 (56.5) | 202 (50.9) | 195 (63.7) | 0.001 | 122 (46.4) | 275 (62.5) | <0.001 |
| Condomless anal intercourse protected by ART or PrEP | 51 (7.3) | 33 (8.3) | 18 (5.9) | 0.873 | 17 (6.5) | 34 (7.7) | 0.045 |
| ART in either partner | 33 (4.7) | 19 (4.8) | 14 (4.6) | 0.437 | 11 (4.2) | 22 (5.0) | 0.120 |
| PrEP in either partner | 18 (2.6) | 14 (3.5) | 4 (1.3) | 0.201 | 6 (2.3) | 12 (2.7) | 0.263 |
| Condomless anal intercourse unprotected by ART or PrEP | 255 (36.3) | 162 (40.8) | 93 (30.4) | 0.004 | 124 (47.2) | 131 (29.8) | <0.001 |
| Any potential risk reduction | 177 (25.2) | 119 (30.0) | 58 (19.0) | 0.064 | 81 (30.8) | 96 (21.8) | 0.168 |
| Strategic positioning | 40 (5.7) | 20 (5.0) | 20 (6.5) | 0.053 | 23 (8.7) | 17 (3.9) | 0.221 |
| Concordant HIV status | 99 (14.1) | 73 (18.4) | 26 (8.5) | 0.007 | 52 (19.8) | 47 (10.7) | 0.769 |
| Withdrawal before ejaculation | 86 (12.2) | 60 (15.1) | 26 (8.5) | 0.140 | 53 (20.2) | 33 (7.5) | 0.019 |
| No potential risk reduction | 78 (11.1) | 43 (10.8) | 35 (11.4) | 0.800 | 43 (16.3) | 35 (8.0) | 0.001 |
| Protected Events (n = 448) | Unprotected CLAI Events (n = 255) | OR (95% CI) | p-Value | aOR (95%CI) | p-Value | |
|---|---|---|---|---|---|---|
| Participant characteristics | ||||||
| Age—mean (SD) | 28.4 (6.3) | 28.0 (6.8) | 1.00 (0.97–1.03) | 0.964 | ||
| Waria or transgender | 44 (9.8) | 25 (9.8) | 0.99 (0.54–1.83) | 0.972 | ||
| Born in Bali | 139 (31.0) | 124 (48.6) | 1.89 (1.32–2.70) | <0.001 | 2.04 (1.29–3.23) | 0.002 |
| Employed/working | 394 (88.0) | 211 (82.8) | 1.18 (0.90–1.57) | 0.235 | ||
| Education: University or diploma | 130 (29.0) | 59 (23.1) | 0.54 (0.30–0.97) | 0.039 | 0.40 (0.20–0.83) | 0.013 |
| Income per month is <2 million IDR | 107 (23.9) | 90 (35.3) | 1.63 (1.12–2.39) | 0.011 | 1.21 (0.76–1.92) | 0.428 |
| Gay/waria social engagement scale—mean (SD) | 3.91 (1.49) | 3.54 (1.49) | 0.87 (0.78–0.98) | 0.023 | 0.95 (0.84–1.11) | 0.611 |
| Sex work in previous 6 months | 160 (35.7) | 116 (45.5) | 1.47 (1.02–2.11) | 0.036 | 1.53 (0.99–2.35) | 0.055 |
| Sex with women and/or waria in previous 6 months | 97 (21.7) | 91 (35.7) | 1.68 (1.14–2.46) | 0.008 | 1.01 (0.63–1.62) | 0.966 |
| Any recreational drug use in previous 6 months 1 | 70 (15.6) | 40 (15.7) | 1.01 (0.62–1.64) | 0.954 | ||
| Used drugs for the purposes of sex in previous 6 months | 51 (11.4) | 33 (12.9) | 1.23 (0.72–2.12) | 0.449 | ||
| Infrequent contact with HIV outreach workers | 205 (45.8) | 148 (58.0) | 1.60 (1.12–2.28) | 0.009 | 1.29 (0.86–1.94) | 0.223 |
| Likes using condoms—mean (SD) | 3.09 (1.09) | 2.45 (1.15) | 0.61 (0.52–0.71) | <0.001 | 0.60 (0.50–0.71) | <0.001 |
| Belief that withdrawal is an effective HIV prevention method—mean (SD) | 0.87 (1.19) | 1.63 (1.21) | 1.62 (1.40–1.88) | <0.001 | 1.51 (1.26–1.82) | <0.001 |
| Likes using withdrawal—mean (SD) | 1.02 (1.30) | 1.67 (1.28) | 1.47 (1.28–1.68) | <0.001 | 1.23 (1.03–1.48) | 0.021 |
| Partner or event characteristics | ||||||
| Age—mean (SD) | 28.8 (8.6) | 29.6 (9.2) | 1.01 (0.99–1.03) | 0.211 | ||
| Waria or transgender | 27 (6.0) | 19 (7.5) | 1.07 (0.55–2.08) | 0.840 | ||
| Born in Bali | 143 (31.9) | 111 (43.5) | 1.37 (1.00–1.88) | 0.053 | 1.00 (0.66–1.52) | 0.990 |
| Romantic partner | 235 (52.5) | 162 (63.5) | 1.53 (1.23–1.90) | <0.001 | 1.77 (1.31–2.39) | <0.001 |
| Group sex event | 25 (5.6) | 25 (9.8) | 1.47 (0.84–2.58) | 0.177 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bavinton, B.R.; Mahendra, I.G.A.A.; Kaldor, J.; Law, M.; Grulich, A.E.; Januraga, P.P. Estimation of Potential HIV Transmission Risk in Recent Anal Intercourse Events among Men Who Have Sex with Men and Transgender Women in Bali, Indonesia. Trop. Med. Infect. Dis. 2021, 6, 139. https://doi.org/10.3390/tropicalmed6030139
Bavinton BR, Mahendra IGAA, Kaldor J, Law M, Grulich AE, Januraga PP. Estimation of Potential HIV Transmission Risk in Recent Anal Intercourse Events among Men Who Have Sex with Men and Transgender Women in Bali, Indonesia. Tropical Medicine and Infectious Disease. 2021; 6(3):139. https://doi.org/10.3390/tropicalmed6030139
Chicago/Turabian StyleBavinton, Benjamin R., I Gusti Agung Agus Mahendra, John Kaldor, Matthew Law, Andrew E. Grulich, and Pande Putu Januraga. 2021. "Estimation of Potential HIV Transmission Risk in Recent Anal Intercourse Events among Men Who Have Sex with Men and Transgender Women in Bali, Indonesia" Tropical Medicine and Infectious Disease 6, no. 3: 139. https://doi.org/10.3390/tropicalmed6030139
APA StyleBavinton, B. R., Mahendra, I. G. A. A., Kaldor, J., Law, M., Grulich, A. E., & Januraga, P. P. (2021). Estimation of Potential HIV Transmission Risk in Recent Anal Intercourse Events among Men Who Have Sex with Men and Transgender Women in Bali, Indonesia. Tropical Medicine and Infectious Disease, 6(3), 139. https://doi.org/10.3390/tropicalmed6030139







