Quality of Malaria Treatment Provided under ‘Better Health Together’ Project in Ethnic Communities of Myanmar: How Are We Performing?
Abstract
1. Introduction
2. Materials and Method
2.1. Study Design
2.2. Setting
2.2.1. General Setting
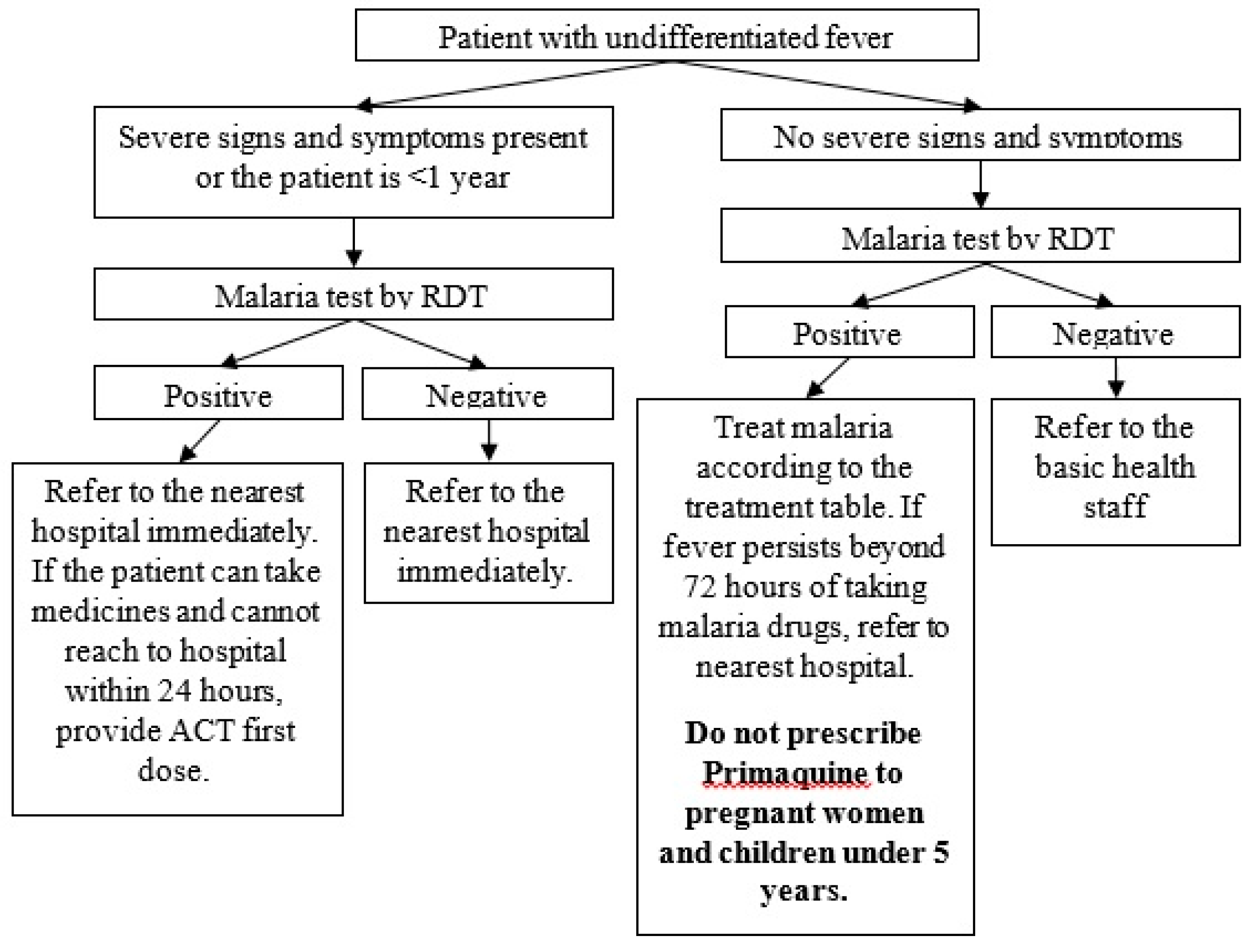
2.2.2. Malaria Diagnosis and Treatment Provided by EHOs
- -
- Generalised weakness so that the person is unable to sit, stand or walk without assistance
- -
- Unable to take medicines due to vomiting
- -
- High fever
- -
- Paleness because of severe anaemia
- -
- Jaundice, yellow sclera
- -
- Impaired consciousness
- -
- Confusion
- -
- Agitation
- -
- Drowsiness
- -
- Irritability
- -
- Breathing difficulty, tightness of chest
- -
- Cold and clammy extremities, signs and symptoms of shock
- -
- Reduced or no urine output
- -
- Fits, loss of consciousness
- -
- Passing of dark colour urine, blood tarry stool
- -
- Bleeding from various sites of body
2.2.3. Recording, Reporting and Data Verification
2.3. Study Population
2.4. Data Variables and Source of Data
2.5. Operational Definitions
2.6. Data Analysis
2.7. Ethics
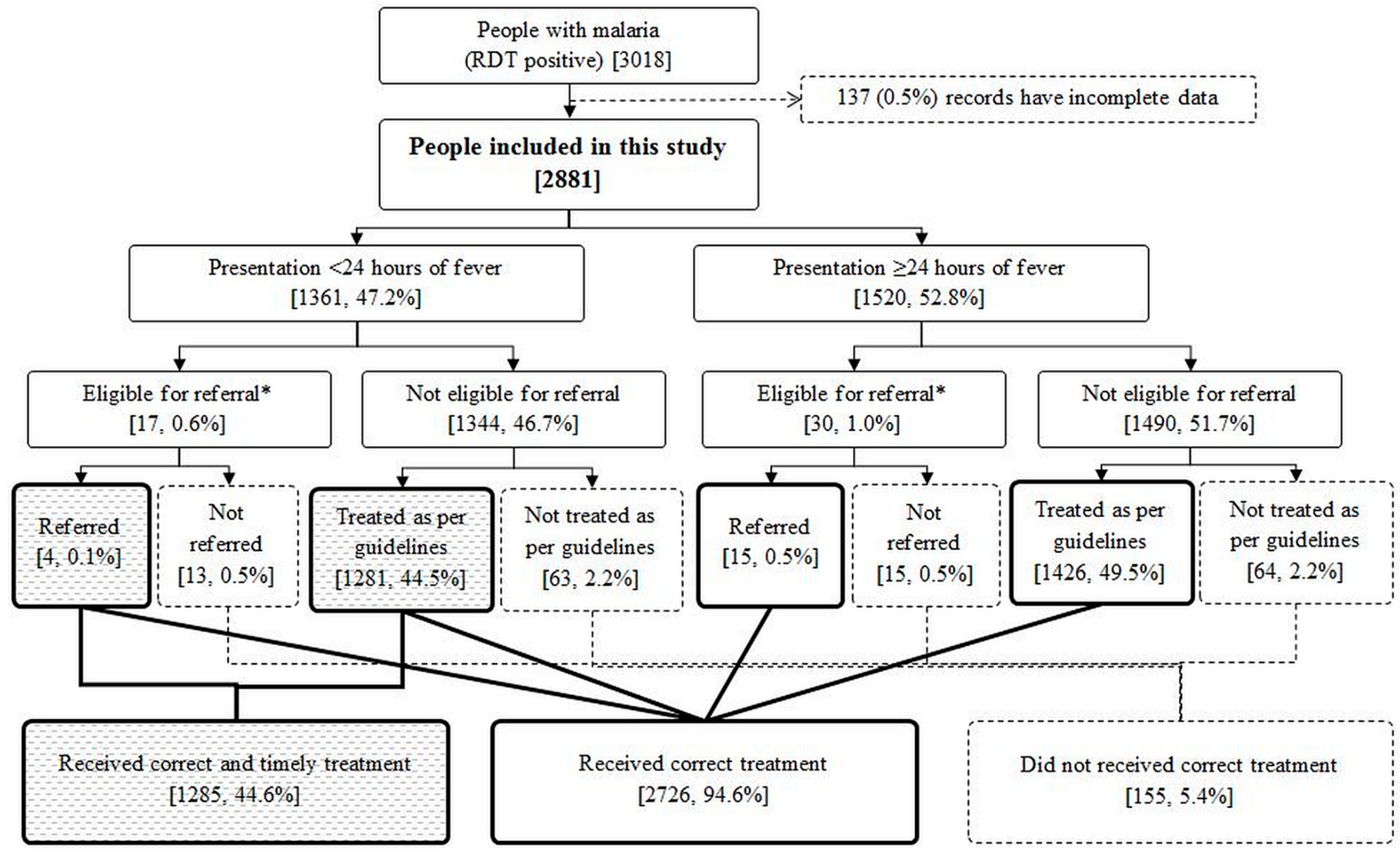
3. Results
3.1. Baseline Characteristics
3.2. Quality of Malaria Treatment and Associated Factors
4. Discussion
4.1. Strengths and Limitations
4.2. Key Findings and Implications
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Disclaimer
References
- World Health Organization. World Malaria Report 2018; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- World Health Organization. Guidelines for the Treatment of Malaria, 3rd ed.; World Health Organization: Geneva, Switzerland, 2015; ISBN 9789241549127. [Google Scholar]
- World Health Organization. Regional Action Plan 2017–2030. Towards 0. Malaria-Free South-East Asia Region; World Health Organization, Regional Office for South-East Asia: New Delhi, India, 2017; ISBN 978 92 9022 625 3. [Google Scholar]
- National Malaria Control Programme. Manual for Integrated Community Malaria Volunteer; National Malaria Control Programme: Nay Pyi Taw, Myanmar, 2017. [Google Scholar]
- National Malaria Control Programme. Guidelines for Malaria Diagnosis and Treatment; Department of Public Health, Ministry of Health and Sports: Nay Pyi Taw, Myanmar, 2015. [Google Scholar]
- Mu, T.T.; Sein, A.A.; Kyi, T.T.; Min, M.; Aung, N.M.; Anstey, N.M.; Kyaw, M.P.; Soe, C.; Kyi, M.M.; Hanson, J. Malaria incidence in Myanmar 2005–2014: Steady but fragile progress towards elimination. Malar. J. 2016, 15, 503. [Google Scholar] [CrossRef] [PubMed]
- Beyrer, C.; Suwanvanichkij, V.; Mullany, L.C.; Richards, A.K.; Franck, N.; Samuels, A.; Lee, T.J. Responding to AIDS, tuberculosis, malaria, and emerging infectious diseases in Burma: Dilemmas of policy and practice. PLoS Med. 2006, 3, e393. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.J.; Mullany, L.C.; Richards, A.K.; Kuiper, H.K.; Maung, C.; Beyrer, C. Mortality rates in conflict zones in Karen, Karenni, and Mon states in eastern Burma. Trop. Med. Int. Health 2006, 11, 1119–1127. [Google Scholar] [CrossRef] [PubMed]
- Health Information System Working Group. The Long Road to Recovery. Available online: https://hiswg.org/wp-content/uploads/2019/05/The-Long-Road-to-Recovery-2015_Eng.pdf (accessed on 6 November 2019).
- Department of Public Health. National Strategic Plan. Intensifying Malaria Control and Accelerating Progress towards Malaria Elimination 2016–2020; Department of Public Health: Nay Pyi Taw, Myanmar, 2017. [Google Scholar]
- Mae Tao Clinic About Us (Mae Tao Clinic). Available online: https://maetaoclinic.org/about-us/history/ (accessed on 26 September 2019).
- National Malaria Control Programme. National Plan for Malaria Elimination (NPME) in Myanmar; National Malaria Control Programme: Nay Pyi Taw, Myanmar, 2016. [Google Scholar]
- Hein, K.T.; Maung, T.M.; Htet, K.K.K.; Shewade, H.D.; Tripathy, J.P.; Oo, S.M.; Lin, Z.; Thi, A. Low uptake of malaria testing within 24 h of fever despite appropriate health-seeking among migrants in Myanmar: A mixed-methods study. Malar. J. 2018, 17, 396. [Google Scholar] [CrossRef] [PubMed]
- Naing, P.A.; Maung, T.M.; Tripathy, J.P.; Oo, T.; Wai, K.T.; Thi, A. Awareness of malaria and treatment-seeking behaviour among persons with acute undifferentiated fever in the endemic regions of Myanmar. Trop. Med. Health 2017, 45, 31. [Google Scholar] [CrossRef] [PubMed]
- Linn, N.Y.Y.; Kathirvel, S.; Das, M.; Thapa, B.; Rahman, M.M.; Maung, T.M.; Kyaw, A.M.M.; Thi, A.; Lin, Z. Are village health volunteers as good as basic health staffs in providing malaria care? A country wide analysis from Myanmar, 2015. Malar. J. 2018, 17, 242. [Google Scholar] [CrossRef] [PubMed]
- Linn, N.Y.Y.; Tripathy, J.P.; Maung, T.M.; Saw, K.K.; Maw, L.Y.W.; Thapa, B.; Lin, Z.; Thi, A. How are the village health volunteers deliver malaria testing and treatment services and what are the challenges they are facing? A mixed methods study in Myanmar. Trop. Med. Health 2018, 46, 28. [Google Scholar] [CrossRef] [PubMed]
- Smith Paintain, L.; Willey, B.; Kedenge, S.; Sharkey, A.; Kim, J.; Buj, V.; Webster, J.; Schellenberg, D.; Ngongo, N. Community health workers and stand-alone or integrated case management of malaria: A systematic literature review. Am. J. Trop. Med. Hyg. 2014, 91, 461–470. [Google Scholar] [CrossRef] [PubMed]
- Win, A.Y.N.; Maung, T.M.; Wai, K.T.; Oo, T.; Thi, A.; Tipmontree, R.; Soonthornworasiri, N.; Kengganpanich, M.; Kaewkungwal, J. Understanding malaria treatment-seeking preferences within the public sector amongst mobile/migrant workers in a malaria elimination scenario: A mixed-methods study. Malar. J. 2017, 16, 462. [Google Scholar] [CrossRef] [PubMed]
- Sunguya, B.F.; Mlunde, L.B.; Ayer, R.; Jimba, M. Towards eliminating malaria in high endemic countries: The roles of community health workers and related cadres and their challenges in integrated community case management for malaria: A systematic review. Malar. J. 2017, 16, 10. [Google Scholar] [CrossRef]
- Lee, J.; Kim, T.I.; Kang, J.M.; Jun, H.; Lê, H.G.; Thái, T.L.; Sohn, W.M.; Myint, M.K.; Lin, K.; Kim, T.S.; et al. Prevalence of glucose-6-phosphate dehydrogenase (G6PD) deficiency among malaria patients in Upper Myanmar. BMC Infect. Dis. 2018, 18, 1–7. [Google Scholar] [CrossRef]

| S. No. | State/Region | Project Implementation Townships | Other Malaria-Related Organisations ^ | Total ICMVs | ICMVs Trained by BHT Project | Estimated Population Covered by BHT Project |
|---|---|---|---|---|---|---|
| 1. | Kachin | Injangyang | HPA | 51 | 6 | 1500 |
| 2. | Kachin | Sumprabum | HPA/MAM | 39 | 39 | 7030 |
| 3. | Kayah | Bawlake | NMCP | 37 | 13 | 3310 |
| 4. | Kayah | Demoso | NMCP/MAM | 146 | 49 | 29,210 |
| 5. | Kayah | Hpasawng | NMCP/MAM | 85 | 22 | 4140 |
| 6. | Kayah | Hpruso | NMCP/MAM | 173 | 60 | 13,950 |
| 7. | Kayah | Loikaw | NMCP | 116 | 64 | 30,780 |
| 8. | Kayah | Mese | NMCP | 26 | 14 | 5230 |
| 9. | Kayah | Shadaw | NMCP | 49 | 16 | 4320 |
| 10. | Kayin | Hlaingbwe | NMCP/ARC/KDHW/MHAA/SCI/SMRU | 709 | 52 | 13,040 |
| 11. | Kayin | Hpa-An | 35 | 35 | 10,500 | |
| 12. | Kayin | Kawkareik | NMCP/ARC/KDHW/MAM/SMRU | 409 | 36 | 14,410 |
| 13. | Kayin | Kyainseikgyi | NMCP/ARC/KDHW/MAM | 658 | 160 | 55,530 |
| 14. | Kayin | Myawaddy | NMCP/ARC/SMRU | 239 | 20 | 42,170 |
| 15. | Kayin | Thandaunggyi | NMCP/MAM | 355 | 16 | 10,430 |
| 16. | Mon | Ye | NMCP/ARC/IOM/KDHW/MAM | 180 | 22 | 10,710 |
| 17. | Tanintharyi | Yebyu | NMCP/ARC/KDHW/MAM/PSI/URC | 245 | 8 | 1440 |
| Total | 3552 | 632 * | 257,700 |
| Age Group (yr) | Artemether 20 mg/Lumefantrine 120 mg Tablet | Primaquine 7.5 mg Tablet | |||||
|---|---|---|---|---|---|---|---|
| 1st Day | 2nd Day | 3rd Day | |||||
| 1st Dose | 2nd Dose | 3rd Dose | 4th Dose | 5th Dose | 6th Dose | Stat Dose | |
| <1 | 1/2 | 1/2 | 1/2 | 1/2 | 1/2 | 1/2 | - |
| 1–4 | 1 | 1 | 1 | 1 | 1 | 1 | - |
| 5–9 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| 10–14 | 3 | 3 | 3 | 3 | 3 | 3 | 4 |
| ≥15 | 4 | 4 | 4 | 4 | 4 | 4 | 6 |
| Age Group (yr) | Chloroquine 150 mg Tablet | Primaquine 7.5 mg Tablet | ||
|---|---|---|---|---|
| 1st Day | 2nd Day | 3rd Day | Stat Dose on 4th Day, Weekly Once for 8 Weeks | |
| <1 | 1/3 | 1/3 | 1/3 | - |
| 1–4 | 1.5 | 1.5 | 1 | - |
| 5–9 | 2 | 2 | 1 | 2 |
| 10–14 | 3 | 3 | 1.5 | 4 |
| ≥15 | 4 | 4 | 2 | 6 |
| Variables | n | (%) | |
|---|---|---|---|
| Total | 2881 | (100.0) | |
| Age in years | |||
| <1 | 25 | (0.9) | |
| 1–4 | 338 | (11.7) | |
| 5–9 | 442 | (15.3) | |
| 10–14 | 387 | (13.4) | |
| ≥15 | 1689 | (58.6) | |
| Gender | |||
| Male | 1836 | (63.7) | |
| Female | 1045 | (36.3) | |
| RDT result | |||
| Pf | 1024 | (35.6) | |
| Pv | 1730 | (60.0) | |
| Mixed | 127 | (4.4) | |
| Severe malaria | |||
| Yes | 22 | (0.8) | |
| No | 2859 | (99.2) | |
| EHO | |||
| EHO A | 912 | (31.7) | |
| EHO B | 121 | (4.2) | |
| EHO C | 202 | (7.0) | |
| EHO D | 491 | (17.0) | |
| EHO E | 886 | (30.8) | |
| EHO F | 269 | (9.3) | |
| State/Region | |||
| Kachin | 202 | (7.0) | |
| Kayah | 129 | (4.5) | |
| Kayin | 2279 | (79.1) | |
| Mon | 65 | (2.3) | |
| Tanintharyi | 206 | (7.2) | |
| Service delivery type | |||
| Health posts^ | 202 | (7.0) | |
| Mobile | 129 | (4.5) | |
| Village-based ICMV | 2279 | (79.1) | |
| Missing | 536 | (9.4) |
| Variables | N | Not Correct Treatment | PR | (95%CI) | aPR | (95%CI) | |
|---|---|---|---|---|---|---|---|
| n | (%) | ||||||
| Total | 2881 | 155 | (5.4) | - | - | ||
| Age in years | |||||||
| <1 | 25 | 19 | (76.0) | 19.75 | (14.27–27.32) | 21.17 | (12.45–35.99) * |
| 1–4 | 338 | 25 | (7.4) | 1.92 | (1.23–3.00) | 2.49 | (1.59–3.89) * |
| 5–9 | 442 | 21 | (4.8) | 1.23 | (0.76–2.00) | 1.53 | (0.96–2.43) |
| 10–14 | 387 | 25 | (6.5) | 1.68 | (1.07–2.63) | 1.71 | (1.13–2.60) * |
| ≥15 | 1689 | 65 | (3.9) | Ref | |||
| Gender | |||||||
| Male | 1836 | 99 | (5.4) | 1.01 | (0.73–1.38) | 1.17 | (0.85–1.60) |
| Female | 1045 | 56 | (5.4) | Ref | |||
| Severe malaria | |||||||
| Yes | 22 | 9 | (40.9) | 8.01 | (4.73–13.56) | 5.21 | (2.49–10.93) * |
| No | 2859 | 146 | (5.1) | Ref | |||
| RDT result | |||||||
| Pf | 1024 | 62 | (6.1) | 1.90 | (1.34–2.72) | 1.84 | (1.29–2.63) * |
| Pv | 1730 | 55 | (3.2) | Ref | |||
| Mixed | 127 | 38 | (29.9) | 9.41 | (6.49–13.65) | 5.49 | (3.57–8.44) * |
| EHO | |||||||
| EHO A | 912 | 50 | (5.5) | 4.05 | (2.17–7.55) | 2.57 | (1.37–4.82) * |
| EHO B | 121 | 12 | (9.9) | 7.32 | (3.37–15.93) | 2.35 | (0.84–6.55) |
| EHO C | 202 | 15 | (7.4) | 5.48 | (2.61–11.53) | 4.82 | (2.35–9.90) * |
| EHO D | 491 | 63 | (12.8) | 9.47 | (5.16–17.39) | 7.11 | (3.82–13.24) * |
| EHO E | 886 | 12 | (1.4) | Ref | |||
| EHO F | 269 | 3 | (1.1) | 0.82 | (0.23–2.9) | 0.00 | (0.00–0.00) |
| State/Region | |||||||
| Kachin | 202 | 15 | (7.4) | 1.38 | (0.82–2.31) | - ** | |
| Kayah | 129 | 14 | (10.9) | 2.01 | (1.19–3.39) | ||
| Kayin | 2279 | 123 | (5.4) | Ref | |||
| Mon | 65 | 0 | (0.0) | - | |||
| Tanintharyi | 206 | 3 | (1.5) | 0.27 | (0.09–0.84) | ||
| Service delivery type | |||||||
| Health posts ^ | 923 | 49 | (5.3) | Ref | |||
| Mobile | 139 | 1 | (0.7) | 0.14 | (0.02–0.97) | 0.10 | (0.01–0.73) * |
| Village-based ICMV | 1283 | 73 | (5.7) | 1.07 | (0.75–1.52) | 0.50 | (0.30–0.83) * |
| Missing | 536 | 32 | (6.0) | 1.12 | (0.73–1.73) | 0.61 | (0.36–1.04) |
| Variables | N | Not ‘Correct and Timely’ Treatment | PR | (95%CI) | aPR | (95%CI) | |
|---|---|---|---|---|---|---|---|
| n | (%) | ||||||
| Total | 2881 | 1596 | (55.4) | - | - | ||
| Age in years | |||||||
| <1 | 25 | 21 | (84.0) | 1.50 | (1.26–1.79) | 1.47 | (1.2–1.79) |
| 1–4 | 338 | 193 | (57.1) | 1.02 | (0.92–1.13) | 1.09 | (0.99–1.2) |
| 5–9 | 442 | 229 | (51.8) | 0.93 | (0.84–1.02) | 0.94 | (0.86–1.04) |
| 10–14 | 387 | 209 | (54.0) | 0.97 | (0.87–1.07) | 0.96 | (0.87–1.06) |
| ≥15 | 1689 | 944 | (55.9) | Ref | |||
| Gender | |||||||
| Male | 1836 | 1044 | (56.9) | 1.08 | (1.00–1.15) | 1.08 | (1.01–1.15) |
| Female | 1045 | 552 | (52.8) | Ref | |||
| Severity | |||||||
| Severe | 22 | 22 | (100.0) | 1.90 | (1.84–1.97) | 1.66 | (1.42–1.93)* |
| Not severe | 2859 | 1574 | (55.1) | Ref | |||
| RDT result | |||||||
| Pf | 1024 | 621 | (60.6) | 1.19 | (1.11–1.27) | 1.22 | (1.14–1.31) |
| Pv | 1730 | 881 | (50.9) | Ref | |||
| Mixed | 127 | 94 | (74.0) | 1.45 | (1.30–1.63) | 1.35 | (1.21–1.52) |
| EHO ID | |||||||
| EHO A | 912 | 558 | (61.2) | 1.28 | (1.18–1.40) | 1.14 | (1.03–1.27) |
| EHO B | 121 | 90 | (74.4) | 1.56 | (1.38–1.77) | 1.46 | (0.95–2.26) |
| EHO C | 202 | 59 | (29.2) | 0.61 | (0.49–0.77) | 0.59 | (0.47–0.74) |
| EHO D | 491 | 349 | (71.1) | 1.49 | (1.37–1.63) | 1.45 | (1.32–1.6) |
| EHO E | 886 | 422 | (47.6) | Ref | |||
| EHO F | 269 | 118 | (43.9) | 0.92 | (0.79–1.07) | 1.06 | (0.68–1.66) |
| State/Region | |||||||
| Kachin | 202 | 59 | (29.2) | 0.50 | (0.40–0.62) | 1.00 | |
| Kayah | 129 | 96 | (74.4) | 1.28 | (1.15–1.43) | 1.10 | (0.73–1.67) |
| Kayin | 2279 | 1324 | (58.1) | Ref | |||
| Mon | 65 | 23 | (35.4) | 0.61 | (0.44–0.85) | 0.74 | (0.47–1.18) |
| Tanintharyi | 206 | 94 | (45.6) | 0.79 | (0.67–0.92) | 0.94 | (0.58–1.51) |
| Service delivery type | |||||||
| Health post ^ | 923 | 569 | (61.7) | Ref | |||
| Mobile | 139 | 61 | (43.9) | 0.71 | (0.59–0.86) | 0.68 | (0.56–0.82) * |
| Village-based ICMV | 1283 | 661 | (51.5) | 0.84 | (0.78–0.90) | 0.79 | (0.71–0.88) |
| Missing | 536 | 305 | (56.9) | 0.92 | (0.84–1.01) | 0.91 | (0.82–1.01) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Minn, P.W.; Shewade, H.D.; Kyaw, N.T.T.; Phyo, K.H.; Linn, N.Y.Y.; Min, M.S.; Aung, Y.N.; Myint, Z.T.; Thi, A. Quality of Malaria Treatment Provided under ‘Better Health Together’ Project in Ethnic Communities of Myanmar: How Are We Performing? Trop. Med. Infect. Dis. 2019, 4, 140. https://doi.org/10.3390/tropicalmed4040140
Minn PW, Shewade HD, Kyaw NTT, Phyo KH, Linn NYY, Min MS, Aung YN, Myint ZT, Thi A. Quality of Malaria Treatment Provided under ‘Better Health Together’ Project in Ethnic Communities of Myanmar: How Are We Performing? Tropical Medicine and Infectious Disease. 2019; 4(4):140. https://doi.org/10.3390/tropicalmed4040140
Chicago/Turabian StyleMinn, Phyo Wai, Hemant Deepak Shewade, Nang Thu Thu Kyaw, Khaing Hnin Phyo, Nay Yi Yi Linn, Myat Sandi Min, Yan Naing Aung, Zaw Toe Myint, and Aung Thi. 2019. "Quality of Malaria Treatment Provided under ‘Better Health Together’ Project in Ethnic Communities of Myanmar: How Are We Performing?" Tropical Medicine and Infectious Disease 4, no. 4: 140. https://doi.org/10.3390/tropicalmed4040140
APA StyleMinn, P. W., Shewade, H. D., Kyaw, N. T. T., Phyo, K. H., Linn, N. Y. Y., Min, M. S., Aung, Y. N., Myint, Z. T., & Thi, A. (2019). Quality of Malaria Treatment Provided under ‘Better Health Together’ Project in Ethnic Communities of Myanmar: How Are We Performing? Tropical Medicine and Infectious Disease, 4(4), 140. https://doi.org/10.3390/tropicalmed4040140





