Impact of the 1918 Influenza Pandemic in Coastal Kenya
Abstract
1. Introduction
2. Methods
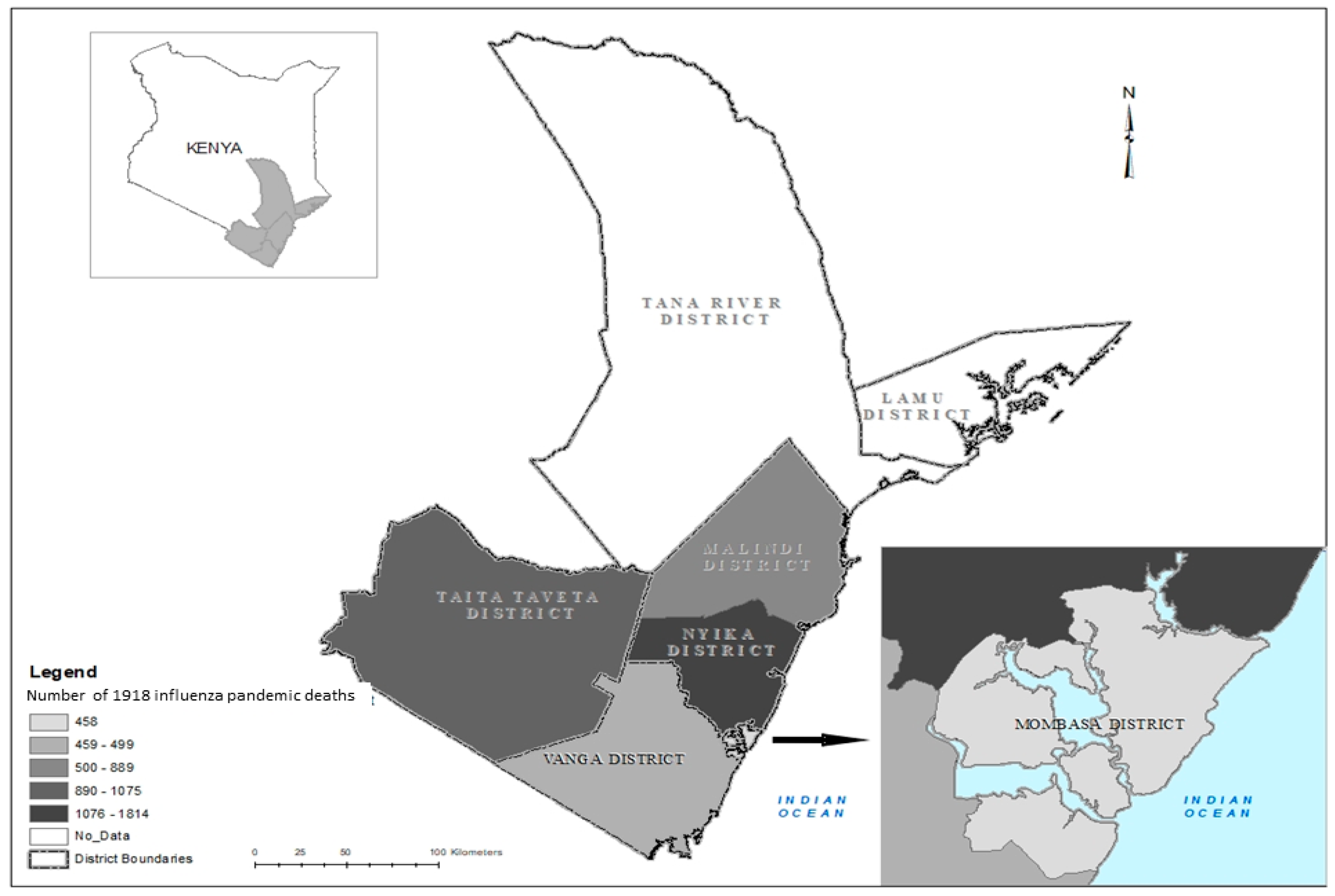
2.1. Study Area Background
2.2. Data Collection and Analysis
2.2.1. Health Information and Population Data, 1912–1925
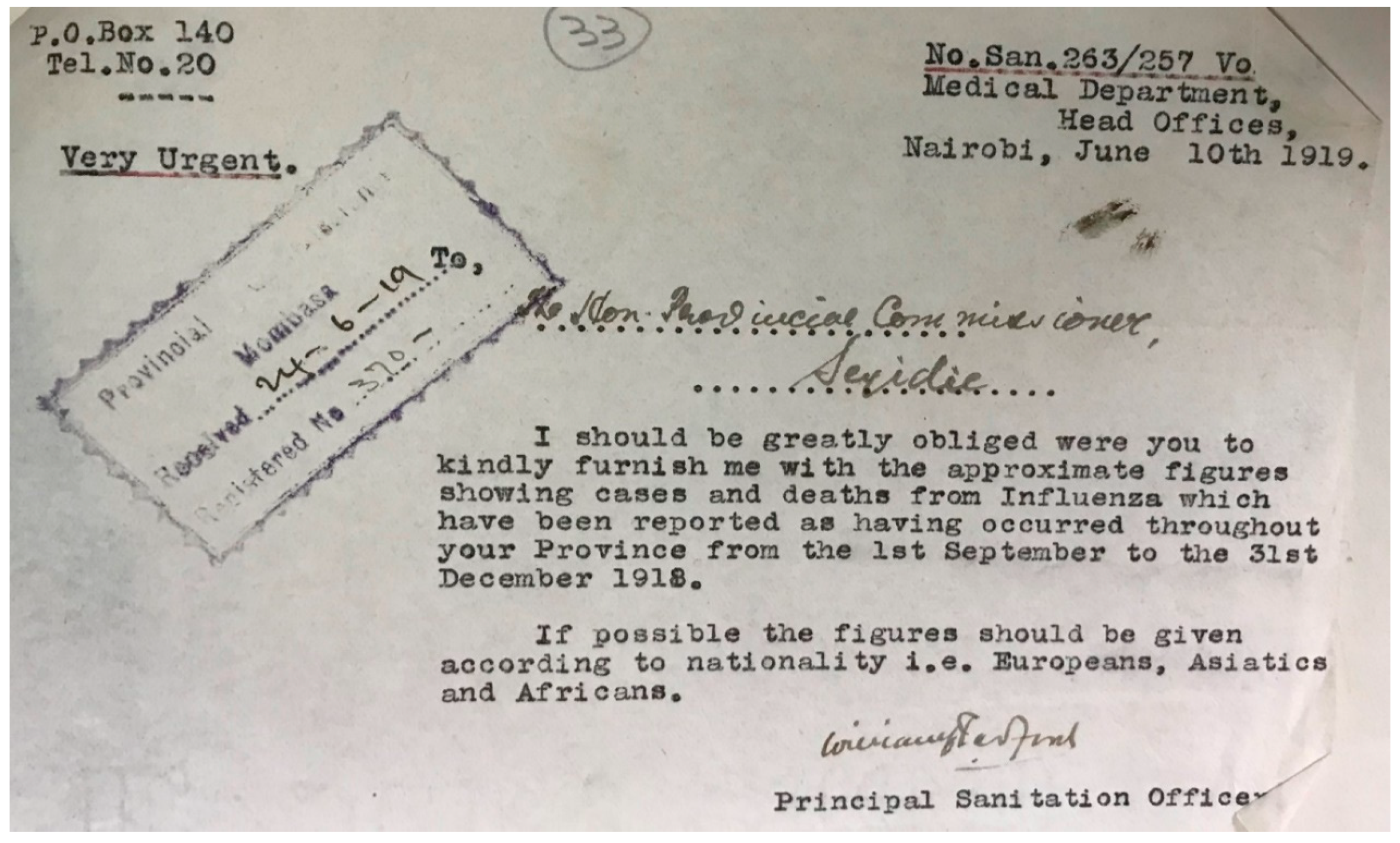
2.2.2. Pandemic Influenza Data, 1918–1919
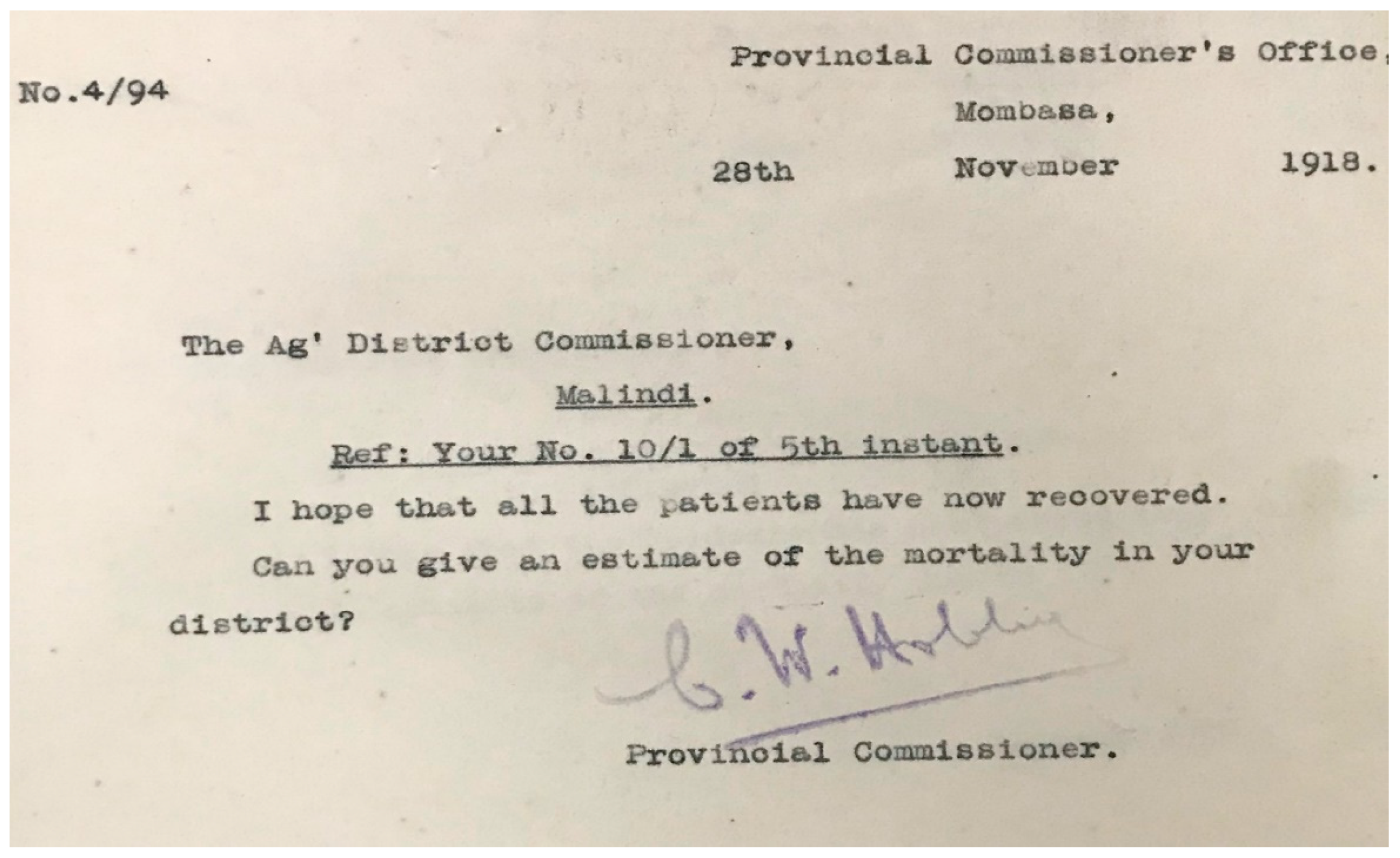
2.2.3. Officials’ Quotes on Pandemic, 1918–1919
3. Results
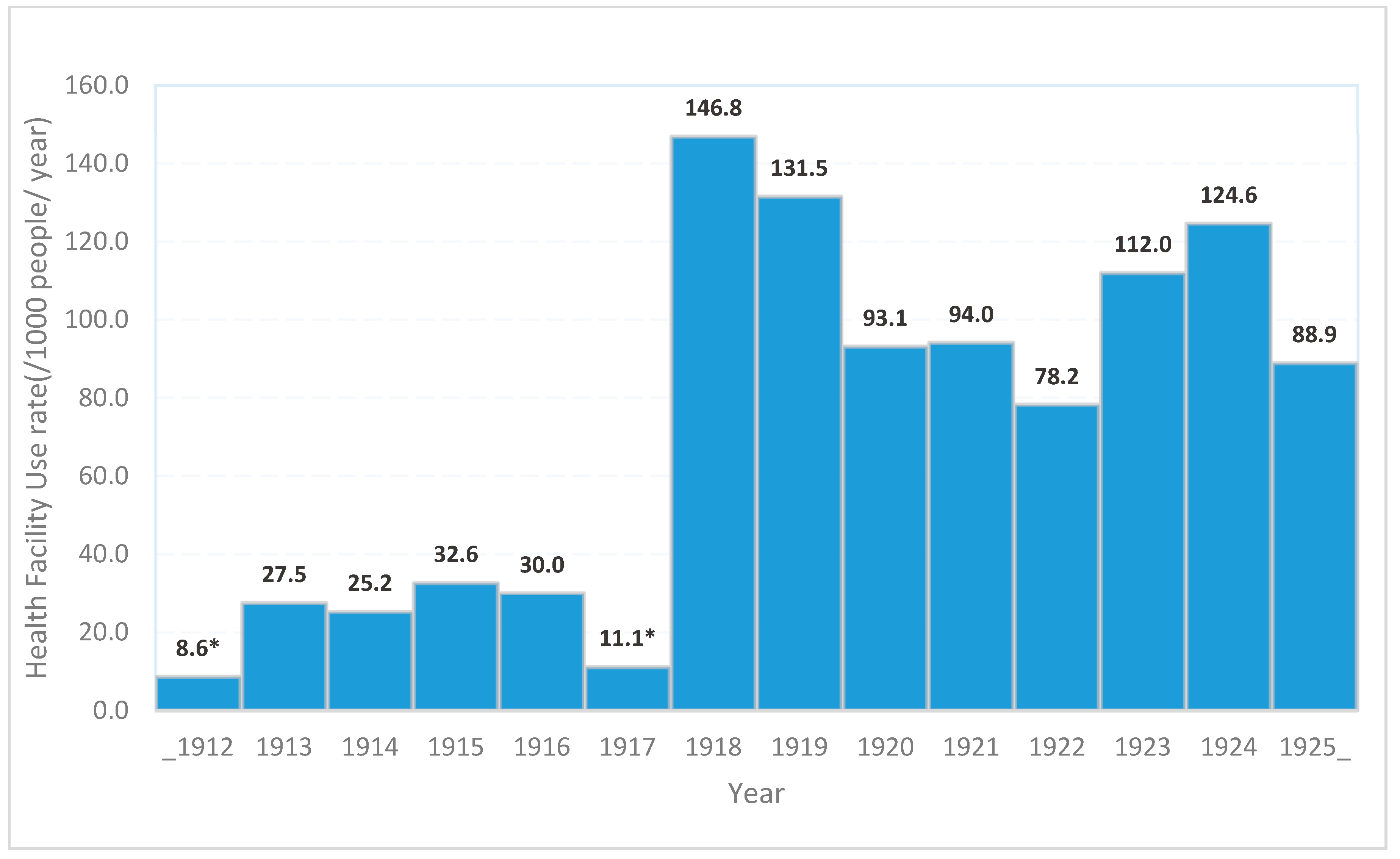
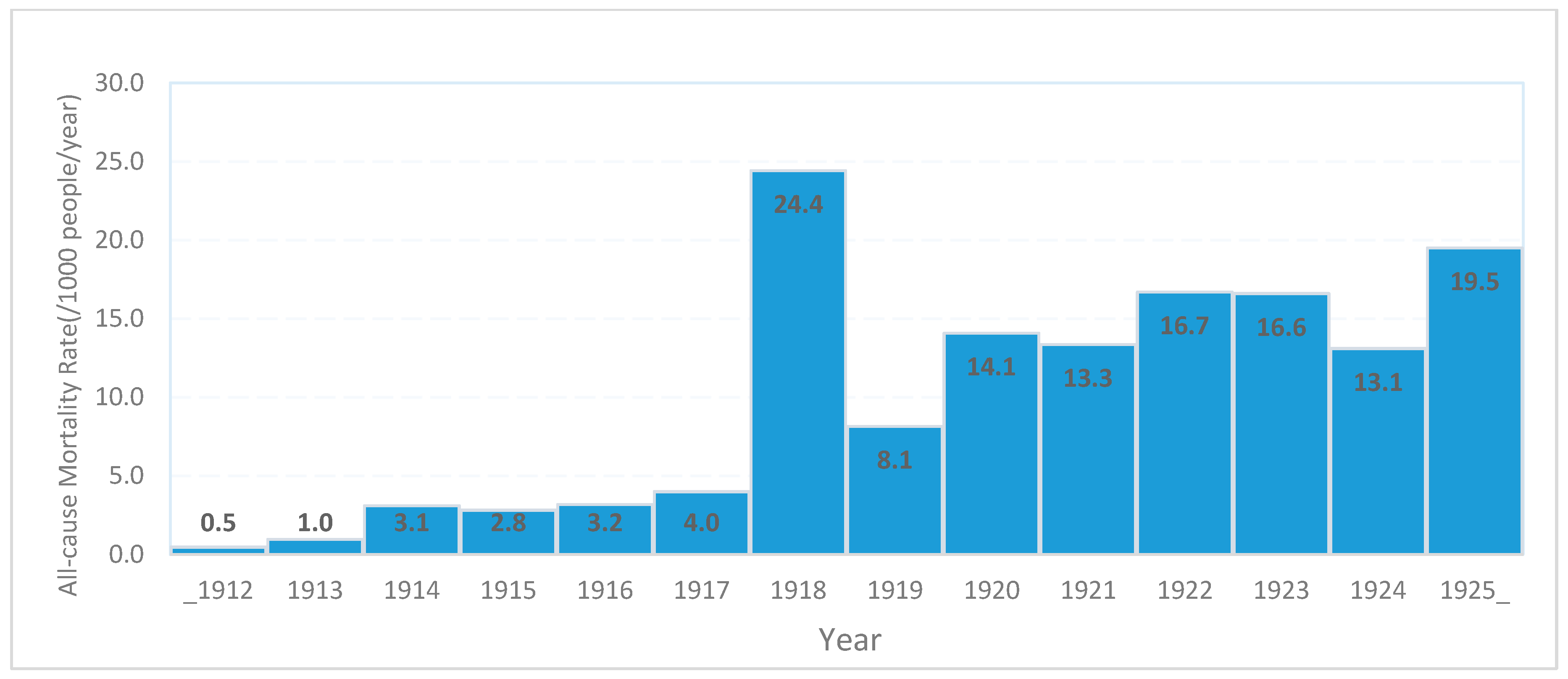
3.1. Health Facility Use and All-Cause Mortality, 1912–1925
3.2. Pandemic Influenza, 1918–1919
3.3. Burden and Clinical Syndrome of Pandemic Influenza
“Similar accounts of the prevalence of influenza with so many cases complicated by pneumonia and consequent high mortality are reported throughout the province. Further medical assistance is not at present available.”CL Chevaliers, Mombasa District. Senior Medical Officer (Civil) 27 November 1918. [Reply letter to Coast Provincial Medical Officer on Spanish flu update: List S1. Spanish Influenza (1918–1919)-KNA/PC/COAST/1/1/369]
“Death occurred mostly among the old men and women, and judging from the number of elders of council reported to have died must have run into hundreds …and … Very few of the young and middle aged …Natives are most secretive about illness and death among their people”.RW Lambert Vanga Kakoneni Asst. District Commissioner (In absence of Ag.D.C) 20 January 1919. [Reply letter to a Senior Medical Officer of Health on Spanish flu update: List S1. Spanish Influenza (1918–1919)-KNA/PC/COAST/1/1/369]
“… at modest estimate between 30% and 40% of the Taita are down with the complaint. The death rate appears during the last few days to be approximately 50 per diem, and to be on the increase. …I anticipate at the present rate if the epidemic is of only 21 days duration the deaths will amount to probably over 1000, whatever action is taken”.Talbot Smith, Taita Taveta District Commissioner on 23 November 1918. [Reply letter to Coast provincial commission on Spanish flu update: List S1. Spanish Influenza (1918–1919)-KNA/PC/COAST/1/1/369]
“I consider the deaths have been augmented when either of the following two conditions have been present. (a) Overcrowding, as in Malindi, Mambrui and Roka. (b) Normally difficult conditions of life. I mean when food has been hard to come by or water far removed from villages. …north bank of the Sabaki River and in Chonyi”.Nyika District Commissioner 1 April 1919. [Reply letter to the senior medical officer on Spanish flu update: List S1. Spanish Influenza (1918–1919)-KNA/PC/COAST/1/1/369]
3.4. Public Health Interventions and Treatment
“… As regards to precautionary measures against the diseases, the avoidance of persons suffering from it, the frequent gargling of the throat (with solutions such as permanganate of Potash (half a grain to the pint), Chlorate of Potash (five grains to the ounces), Borax (ten grains to the ounces) etc.), the taking of small doses of quinine (two grains) morning and evening, keeping of ones dwelling well ventilated, and the living of a quiet life, keeping as much in the open air as possible are useful practices”.AD Milne Principal Medical Officer East Africa Protectorate on 21 November 1918. [Memo on precautionary measures against the Spanish flu to all Provincial and District medical officers in the East Africa Protectorate: List S1. Spanish Influenza (1918–1919)-KNA/PC/COAST/1/1/369]
“… The administration of one teaspoonful of paraffin oil three times a day has been spoken of as having good result when administered to Africans suffering from this disease. As regards the dieting of the sick, milk, uji (Porridge) of wimbi (millet meal), mtama (finger millet meal), or mahindi (maize meal), and such should be given at frequent intervals.”AD Milne Principal Medical Officer East Africa Protectorate on 21 November 1918. [Memo on precautionary measures against the Spanish flu to all Provincial and District medical officers in the East Africa Protectorate: List S1. Spanish Influenza (1918–1919)-KNA/PC/COAST/1/1/369]
“Possibly simple remedies which would give confidence without doing harm could be issued to chiefs for distribution such as quinine, salts or what not. My present object is to try and secure confidence and avoid possibilities of panic which I fear and which may be stopped if harmless faith giving remedies be supplied”.Nyika District Commissioner 14 April 1919. [Memo on precautionary measures against the Spanish flu to all Provincial and District medical officers in the East Africa Protectorate: List S1. Spanish Influenza (1918–1919)-KNA/PC/COAST/1/1/369]
3.5. Social and Economic Disruption
“Sir, I regret to report that the work of the district has been much retarded for the last ten days owing to influenza. The following Govt. servants have been off duty for the whole or part of the period…”SH Jadlau Malindi Ag. District Commissioner, 5 November 1918. [Letter to Provincial Commissioner reporting on the impact of Spanish flu: List S1. Spanish Influenza (1918–1919)-KNA/PC/COAST/1/1/369]
“…Influenza is getting no better, and we are having more deaths. On account of it, it is impossible to get porters, so we have had to write this morning to put off Dr. Shepherd’s Safari. He was to have brought me up the most pressingly needed drugs now they will be delayed.”Ada Drake, Sub Assistant Surgeon, Dabida Taita Taveta District, 25 November 1918. [Letter to District Commissioner requesting administrative support following a social disruption by Spanish flu incursion: List S1. Spanish Influenza (1918–1919)-KNA/PC/COAST/1/1/369]
“Those locations where there has been a total or partial failure of crops, necessitating the inhabitants being on more or less half rations are suffering the most owing presumably to reduced vitality. …These natives are now suffering from reduced vitality and possibly cannot at least for the moment pay for assistance, as well as hut tax.”Mr Talbot Smith, Taita Taveta Voi, District Commissioner 25 November 1918. [Letter to Provincial Commissioner reporting on the impact of Spanish flu: List S1. Spanish Influenza (1918–1919)-KNA/PC/COAST/1/1/369]
“The Kedal Fibre Estate, BEA Corporation Estate (Farms) and the Haubner Estate (Farms) have virtually had to close down. The sub assistant surgeon seems to have run out of the necessary medicine owing to the abnormal drain and I trust you will find your way to supply whatever is necessary”.Mr Talbot Smith, Taita Taveta Voi, District Commissioner 23 November 1918. [Letter to Provincial Commissioner reporting the impact of Spanish flu: List S1. Spanish Influenza (1918–1919)-KNA/PC/COAST/1/1/369]
“Miss Drake to my knowledge has been treating 300 and more patients and would treat nearly 3000 if remedies had permitted”.Mr Talbot Smith, Taita Taveta Voi, District Commissioner 27 November 1918. [Letter to Provincial Commissioner reporting the impact of Spanish flu: List S1. Spanish Influenza (1918–1919)-KNA/PC/COAST/1/1/369]
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Centers for Diseases Control and Prevention. Remembering the 1918 Influenza Pandemic. CDC Features, 2018. Available online: https://www.cdc.gov/features/1918-flu-pandemic/index.html (accessed on 1 August 2018).
- Barry, J.M. The site of origin of the 1918 influenza pandemic and its public health implications. J. Transl. Med. 2004, 2, 4–7. [Google Scholar] [CrossRef] [PubMed]
- Oxford, J.S.; Sefton, A.; Jackson, R.; Johnson, N.P.A.S.; Daniels, R.S. Who’s that lady? Nat. Med. 1999, 5, 1351–1352. [Google Scholar] [CrossRef] [PubMed]
- Erkoreka, A. Origins of the Spanish Influenza pandemic (1918–1920) and its relation to the First World War. J. Mol. Genet. Med. 2009, 3, 190–194. [Google Scholar] [PubMed]
- Barry, J.M.; Viboud, C.; Simonsen, L. Cross-Protection between Successive Waves of the 1918–1919 Influenza Pandemic: Epidemiological Evidence from US Army Camps and from Britain. J. Infect. Dis. 2008, 198, 1427–1434. [Google Scholar] [CrossRef] [PubMed]
- Taubenberger, J.K.; Morens, D.M. 1918 Influenza: The mother of all pandemics. Emerg. Infect. Dis. 2006, 12, 15. [Google Scholar] [CrossRef] [PubMed]
- Chandra, S.; Kassens-Noor, E. The evolution of pandemic influenza: Evidence from India, 1918–19. BMC Infect. Dis. 2014, 14, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Ansart, S.; Pelat, C.; Boelle, P.Y.; Carrat, F.; Flahault, A.; Valleron, A.J. Mortality burden of the 1918–1919 influenza pandemic in Europe. Influenza Other Respir. Viruses 2009, 3, 99–106. [Google Scholar] [CrossRef]
- Afkhami, A. Compromised constitutions: The Iranian experience with the 1918 influenza pandemic. Bull. Hist. Med. 2003, 77, 367–392. [Google Scholar] [CrossRef]
- Chandra, S. Mortality from the influenza pandemic of 1918–19 in Indonesia. Popul. Stud. 2013, 67, 185–193. [Google Scholar] [CrossRef]
- Patterson, K.D.; Pyle, G.F. The geography and mortality of the 1918 influenza pandemic. Bull. Hist. Med. 1991, 65, 4–21. [Google Scholar]
- Johnson, N.P.; Mueller, J. Updating the accounts: Global mortality of the 1918-1920 ‘Spanish’ Influenza Pandemic. Bull. Hist. Med. 2002, 76, 105–115. [Google Scholar] [CrossRef] [PubMed]
- Mueller, J.D. The Spanish Influenza Pandemic of 1918-19 in Sub-Saharan Africa. In Patterns of Reaction to A Demographic Crisis. The Spanish Influenza Pandemic of 1918-1919 in sub-Saharan Africa. A Research Proposal and Preliminary Regional and Comparative Findings: Staff Seminar Paper No.6 (1994/95); University of Nairobi: Nairobi, Kenya, 1995. [Google Scholar]
- Ohadike, D.C. The influenza pandemic of 1918–19 and the spread of cassava cultivation on lower Niger: A case study in historical linkages. J. Afr. Hist. 1981, 22, 379–391. [Google Scholar] [CrossRef]
- Patterson, K.D.; Pyle, G.F. The diffusion of influenza in sub-saharan Africa during the 1918–1919 pandemic. Soc. Sci. Med. 1983, 17, 1299–1307. [Google Scholar] [CrossRef]
- Phillips, H. Influenza Pandemic. In 1914–1918—Online. International Encyclopedia of the First World War; Daniel, U., Gatrell, P., Janz, O., Jones, H., Keene, J., Kramer, A., Eds.; Universität Berlin: Berlin, Germany, 2014. [Google Scholar]
- Murray, C.J.; Lopez, A.D.; Chin, B.; Feehan, D.; Hill, K.H. Estimation of potential global pandemic influenza mortality on the basis of vital registry data from the 1918–20 pandemic: A quantitative analysis. Lancet 2006, 368, 2211–2218. [Google Scholar] [CrossRef]
- Tomkins, S.M. Colonial Administration in British Africa during the Influenza Epidemic of 1918–1919. Can. J. Afr. Stud. 1994, 28, 60–83. [Google Scholar]
- Dawson, M.H. Socio-Economic and Epidemiological Change in Kenya: 1880–1925. Ph.D. Thesis, The University of Wisconsin, Madison, WI, USA, 1983. [Google Scholar]
- Iuliano, A.D.; Roguski, K.M.; Chang, H.H.; Muscatello, D.J.; Palekar, R.; Tempia, S.; Cohen, C.; Gran, J.M.; Schanzer, D.; Cowling, B.J.; et al. Estimates of global seasonal influenza-associated respiratory mortality: A modelling study. Lancet 2018, 391, 1285–1300. [Google Scholar] [CrossRef]
- Widdowson, M.A.; Iuliano, A.D.; Dawood, F.S. Challenges to global pandemic mortality estimation. Lancet Infect. Dis. 2014, 14, 670–672. [Google Scholar] [CrossRef]
- Katz, M.A.; Schoub, B.D.; Heraud, J.M.; Breiman, R.F.; Njenga, M.K.; Widdowson, M.A. Influenza in Africa: Uncovering the Epidemiology of a Long-Overlooked Disease. J. Infect. Dis. 2012, 206 (Suppl. 1), S1–S4. [Google Scholar] [CrossRef]
- Morgan, W.T.W. The Ethnic Geography of Kenya on the Eve of Independence: The 1962 Census. Erdkunde 2000, 54, 76–87. [Google Scholar] [CrossRef]
- Waris, A. Taxation without Principles: A Historical Analysis of the Kenyan Taxation System. Kenya Law Rev. 2007, 1, 272–304. [Google Scholar]
- Beck, S. East Africa 1700–1950. In MidEast & Africa 1700–1950; Ethics Civ., World Peace Communication: Santa Barbara, CA, USA, 2018; p. 671. [Google Scholar]
- Phillips, H. Black October: The Impact of the Spanish Influenza Epidemic of 1918 on South Africa. Ph.D. Thesis, University of Cape Town, Cape Town, South Africa, 1984. [Google Scholar]
- Watts, M.J.; Bohle, H.G. The space of vulnerability: The causal structure of hunger and famine. Prog. Hum. Geogr. 1993, 17, 43–67. [Google Scholar] [CrossRef]
- Roberts, J.I. The Endemicity of Plague in East Africa. East. Afr. Med. J. 1935, 12, 200–219. [Google Scholar]
- Dawson, M.H. SmallPox in Kenya, 1880–1920. Soc. Sci. Med. 1979, 13, 245–259. [Google Scholar] [CrossRef]
- Samuel-Mbaekwe, I.J. Colonialism and social structure. Transafrican J. Hist. 1986, 15, 81–95. [Google Scholar]
- Short, K.R.; Kedzierska, K.; van de Sandt, C.E. Back to the Future: Lessons Learned From the 1918 Influenza Pandemic. Front. Cell. Infect. Microbiol. 2018, 8, 343. [Google Scholar] [CrossRef] [PubMed]
- Wever, P.C.; van Bergen, L. Death from 1918 pandemic influenza during the First World War: A perspective from personal and anecdotal evidence. Influenza Other Respi. Viruses 2014, 8, 538–546. [Google Scholar] [CrossRef] [PubMed]
- Mamelund, S.E. Geography may explain adult mortality from the 1918–20 influenza pandemic. Epidemics 2011, 3, 46–60. [Google Scholar] [CrossRef] [PubMed]
- Phillips, H. Why did it happen? Religious and lay explanations of the Spanish Flu epidemic of 1918 in South Africa. Hist. Speak. 2008, 9, 34–36. [Google Scholar] [CrossRef]
- Mueller, J.D. What’s in a name. Spanish Influenza in sub-Saharan Africa and what local names say about the perception of this pandemic. In The Spanish Flu 1918–1998: Reflections on the Influenza Pandemic of 1918–1919 after 80 Years; Echenberg, M., Crosby, A., Mueller, J.D., Ramanna, M., Eds.; History Department, University of Hannover: Cape Town, South Africa, 1998; pp. 1–14. [Google Scholar]
- Radin, J.M.; Katz, M.A.; Tempia, S.; Talla Nzussouo, N.; Davis, R.; Duque, J.; Adedeji, A.; Adjabeng, M.J.; Ampofo, W.K.; Ayele, W.; et al. Influenza surveillance in 15 countries in Africa, 2006–2010. J. Infect. Dis. 2012, 206 (Suppl. 1), S14–S21. [Google Scholar] [CrossRef]
| Coast Province Kenya District Name | Population Distribution by District and Race | |||
|---|---|---|---|---|
| Total N (% total) | Europeans N (%) | Asians/Arabs N (%) | Natives N (%) | |
| 1. Mombasa Island | 36,824 (20.4) | 371 (1.0) | 10,774 (29.2) | 25,679 (69.6) |
| 2. Vanga | 19,761 (10.9) | 5 (<1) | 423 (2.1) | 19,333 (97.0) |
| 3. Taita Taveta | 30,545 (16.9) | 16 (<1) | 135 (<1) | 30,394 (99.5) |
| 4. Nyika | 71,137 (39.3) | 21 (<1) | 215 (<1) | 70,901 (99.7) |
| 5. Malindi | 22,872 (12.6) | 13 (<1) | 1529 (6.7) | 21,330 (93.3) |
| Total N (%) | 181,139 (100.0) | 426 (0.3) | 13076 (7.2) | 167,637 (92.5) |
| District Name | Population Estimates | Reported Influenza Cases | Reported Influenza Mortality | Influenza Case Fatality Proportion (%) | ||
|---|---|---|---|---|---|---|
| Number | Rate (per 1000) | Number | Rate (per 1000) | |||
| 1. Mombasa Island | 36,884 | 1217 | 33.0 | 628 | 17.0 | 51.6 |
| 2. Vanga | 19,761 | - | - | 400 | 20.2 | - |
| 3. Taita Taveta | 30,545 | 10,691 | 350.0 | 1065 | 34.9 | 9.9 |
| 4. Nyika | 71,137 | 20,000 | 281.1 | 1700 | 23.9 | 8.5 |
| 5. Malindi | 22,872 | - | - | 800 | 35.0 | - |
| Total | 181,199 | 31,908 | 176.1 * | 4593 | 25.3 | 10.6 * |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Andayi, F.; Chaves, S.S.; Widdowson, M.-A. Impact of the 1918 Influenza Pandemic in Coastal Kenya. Trop. Med. Infect. Dis. 2019, 4, 91. https://doi.org/10.3390/tropicalmed4020091
Andayi F, Chaves SS, Widdowson M-A. Impact of the 1918 Influenza Pandemic in Coastal Kenya. Tropical Medicine and Infectious Disease. 2019; 4(2):91. https://doi.org/10.3390/tropicalmed4020091
Chicago/Turabian StyleAndayi, Fred, Sandra S. Chaves, and Marc-Alain Widdowson. 2019. "Impact of the 1918 Influenza Pandemic in Coastal Kenya" Tropical Medicine and Infectious Disease 4, no. 2: 91. https://doi.org/10.3390/tropicalmed4020091
APA StyleAndayi, F., Chaves, S. S., & Widdowson, M.-A. (2019). Impact of the 1918 Influenza Pandemic in Coastal Kenya. Tropical Medicine and Infectious Disease, 4(2), 91. https://doi.org/10.3390/tropicalmed4020091




