Abstract
Introduction: Diarrheal diseases are a global public health problem and one of the leading causes of mortality, morbidity and economic loss. The objective of the study is to estimate the economic cost of caregivers and cost distribution per diarrheal episodes in Bangladesh. Methods: This was a cross-sectional hospital-based study conducted in public hospitals in Bangladesh. A total of 801 diarrheal patients were randomly selected and interviewed during January to December 2015. Simple descriptive statistics including frequencies, percentage, mean with 95% CI and median are presented. Results: The overall average cost of caregivers was BDT 2243 (US$ 28.58) while only BDT 259 (US$ 3.29) was spent as out of pocket payments. Caregivers mostly spent money (US$ 1.63) for food, lodging, utility bills, and other lump sum costs followed by the transportation costs (US$ 1.57). The caregivers spent more (US$ 44.45) when they accompanied the patients who were admitted in inpatients care and almost 3.6 times higher than for out-patients care (US$ 12.42). Conclusions: The study delivers an empirical evidence to the health-care programmers and policy makers about the economic cost of caregivers during diarrheal treatment care, which should be accounted for in designing future diarrheal prevention programme.
1. Introduction
Diarrheal diseases remain one of the major causes of mortality and morbidity worldwide. Every year, approximately 2.39 billion diarrheal cases occurs globally, and in 2015 an estimated 0.53 million of under five children died due to diarrhoea [1,2] which was about nine per cent of all deaths among children under five years of age [3]. Specifically, incidence and case-fatality ratios are much higher in lower- and middle-income countries than developed economies [4]. Like many other developing countries, diarrhoea is an overwhelming public health problem in Bangladesh. Though the mortality due to diarrheal illness has significantly declined over the last decade, the morbidity remains stable in Bangladesh. In the last five years, approximately 12.9 million patients had visited health facilities for seeking care while at least 115 patients died [5]. However, numerous diarrheal cases occurred in community level and many of them were managed at household level and remain unreported, thus, the real diarrheal burden is still unknown.
Diarrhoea is one of the highly prevalent communicable diseases in Bangladesh. The diarrheal infection is common in all age groups, and children under five years of age suffer significantly in Bangladesh [6]. Bangladesh is located within a broad delta formed by the Ganges and Brahmaputra rivers of South Asia; the country is exceedingly flat, with low-lying land, subject to annual floods, and a natural disaster-prone area. Bangladesh is now undergoing a rapid urbanisation process. However, about one-third of the urban population live in urban slums, which are often considered high-risk areas for diarrheal infections [7]. Further, the diseases are highly sensitive to climate, showing seasonal variations in many places of the country [8]. Relative humidity and temperature are the other important factors that influence the rate of replication of different infectious organisms (e.g., bacteria and protozoa) and the survival of enteroviruses in the environment which cause diarrheal infections in Bangladesh [9]. diarrhoea is often referred as an alteration in normal bowel movement characterized by an increase in water content, volume, or frequency of stools [10]. A diarrheal episode is considered as the passage of three or more loose or liquid stools in 24 h prior to presentation for care, which is considered the most practicable definition among children and adults [11]. If the disease lasts “more than 7 days” and “at least 14 days” then the terms “prolonged” and “persistent” diarrhoea are used respectively [12,13]. diarrhoea is caused by many infectious organisms, including bacteria (e.g., Escherichia coli, Vibrio chollerae Shigella, Salmonella), viruses (e.g., Rotavirus, Adenovirus, Norovirus) and parasites (e.g., Entamoeba Histolytia, Giardia Lamblia). Poor sanitation systems, lack of potable water and inadequate personal hygiene are important risk factors for diarrheal disease which is accountable for up to 90% of all diarrheal cases [14], although it is the most prevalent disease that affects all irrespective of socio-economic status. The disease can be prevented and managed at household level with low cost oral rehydration therapy (ORT), however, the patient frequently visits the health facilities which imposes a substantial economic burden for the affected households [15,16]. Recent study showed that by controlling diarrheal diseases households could save approximately US$ 136.03 million in Bangladesh which usually exhausted for receiving treatment [17].
Diarrheal diseases are one of the major causes of hospitalization among under-five children in Bangladesh. According to the latest hospital-based surveillance in Bangladesh, childhood diarrheal diseases were responsible for 40% and 18% of hospital admissions in sub-district and district level hospitals respectively, while at least 7% of under-five children were admitted to the medical college hospitals [5]. Although diarrheal diseases can be managed by low-cost interventions, however, an earlier study observed that about 75% of the under five children receive treatments from formal healthcare providers [18]. However, the treatment seeking pattern for diarrheal disease varies to a greater extent for children than for adults as children frequently visit the local private practitioners before hospitalization which eventually is reflected in its treatment costs [18,19].
There are numerous studies focusing on the economics of diarrheal disease around the world however, research focusing on the caregivers’ cost during the diarrheal episode is still limited globally [20,21,22,23,24,25]. A hospital-based study captured the unit cost of inpatients and outpatients from providers’ points of view rather than household perspectives in Asia [26]. Another hospital-based study also reported the cost for treating <5 diarrheal patients in Bangladesh but failed to capture all component (e.g., laboratory cost and income loss) of costs [27]. None of the studies specifically focused on the caregivers’ point of views. Caregivers’ time and direct expenditure are important cost component and have an impact on the livelihoods of families and particularly for those who live further away from treatment facilities [17,28,29,30]. To the best of our knowledge, this is the first study to analyse the distribution of caregivers’ cost in Bangladesh, although caregivers’ time and financial resources could upturn the overall cost of treatment for household perspective. Earlier hospital-based survey indicated that approximately 44 percent of the total diarrheal patients required hospitalization and the remaining patients received outpatient services [17]. However, in both cases, the caregiver’s involvement is a common phenomenon. In this aspect, the objective of the study is to estimate the average cost of caregivers and cost distribution during diarrheal episodes in Bangladesh. Given the current focus on the treatment cost from household perspective, the study aims to analyse both the costs of outpatients and inpatients during diarrheal infections. We expect that our findings will help policy makers to evaluate and design the diarrhoea related preventive or promotive health intervention at the household level.
2. Materials and Methods
2.1. Design and Study Population
This was a cross-sectional descriptive study conducted in public hospitals in Bangladesh. Public hospitals play a major role in providing treatment to the relatively large population with low cost, as those hospitals are highly subsidized and financed by the government of Bangladesh. Thus, a large number of patients irrespective of socio-economic strata frequently seek care from public hospitals. A total of 801 diarrheal patients were randomly selected and interviewed during January to December 2015. Respondents of this study were adult caregivers or economic contributors or adult patients. The study was conducted from a caregiver’s perspective which means all types of caregiver’s costs were identified, measured and valued [31].
2.2. Cost Estimates
The aim of this study was to analyse the caregivers’ cost associated with the diarrheal treatment. In the study caregivers can be mother, father, spouses, descendants, siblings or close relative, who have no training in child health or education except their own experience and accompany during the hospitalization and aged 18 and above [19]. To estimate the cost of caregivers, both direct and indirect costs were captured. Out of pocket costs were defined as expenditure by caregivers for themselves which includes transportation, lodging, food items, informal payment, utility bills and other associated payments which was not directly linked with the treatment of patients. Indirect cost was considered as the income losses, as well as productivity losses of caregivers because of travel and stay at the health centre and costs due to absence from work. Self-reported wage rates were used for estimating the income losses. The inclusion of caregiving time based on the assumption that time dedicated to caregiving may represent foregone non-market activities such as education, household chores, child care, and leisure or domestic work [32,33]. Productivity costs were estimated using the human capital approach [34]. To capture the productivity losses for non-market activities, the minimum wage rate of Bangladesh according to the national level was considered. Caring for a patient with diarrhoea may have in negative impact on the emotional and physical conditions of the caregivers which was not captured in the previous studies [33,35]. Furthermore, time cost of visitors and extra irregular expense borne by the caregivers and visitors were not included in the analysis.
2.3. Data Collection
Data were collected by face-to-face interviews during discharge from the hospitals. Respondents were adult patients or the accompanying persons who were most familiar with the costs incurred during the treatment of the patient. A research assistant reviewed patient’s records, and data extraction forms were updated daily until the discharge of the patients. A telephone interview was also conducted for taking necessary information within one week after discharge from the hospital. Questions were asked regarding transportation, expenses during the hospitalization, and losses of wages resulting from absence from work.
2.4. Data Analysis
Data analysis was performed using Microsoft Excel and Stata/SE 13.0 (StataCorp, College Station, TX, USA). Simple descriptive statistics including frequencies, percentage, mean (95% CI) and median were presented in local currency, i.e., Bangladeshi Taka (BDT) and US dollars (US$) applying the exchange rate (US$ 1 = 78.5 BDT) during the year of the survey; mid-2014–mid-2015 [36].
2.5. Ethical Approval
The research protocol of this study, PR 13064 was approved by the Institutional Review Board of the International Centre for Diarrheal Disease Research, Bangladesh (icddr,b). Informed consent was obtained from all respondents before data collection.
3. Results
3.1. Background Characteristics of Study Participants
The background characteristics of patients and their caregivers are presented in Table 1. A higher proportion of the diarrheal patients were children aged less than five years (57%) followed by adult patients aged 20 to 64 years (25%). The proportion of male and female patients were almost same (50%), and utilization of inpatient care service was slightly higher (52%) than outpatient services. Except the children aged less than five years (57%), housewives (16%), and students (10%) were two most vulnerable occupational groups for diarrheal infection. Parents (64%) were the most common person caring for their children during diarrheal treatment, indeed most of the caregivers were housewives (90%). The monthly income and expenditure of the households were BDT 19,603 (US$ 250) and BDT 15,470 (US$ 197) respectively, while the average last three months healthcare expenditure was BDT 5191 (US$ 66) considering last three months preceding to the survey.

Table 1.
Distribution of socio-demographic characteristics of diarrheal patients (N = 801).
3.2. Average Caregivers’ Cost
The average caregivers’ economic cost and its distribution were reported in Table 2. The overall average caregivers’ cost for attending with their diarrheal patients was BDT 2, 243 (US$ 28.58) while only BDT 258.57 (US$ 3.29) was spent as out of pocket payment. Among this expenditure, caregivers spent most for food, lodging, utility bills, and other lump sum costs jointly (BDT 127.87 or US$ 1.63) followed by the transportation costs (BDT 123.29 or US$ 1.57). As with overall care, the cost distribution pattern was similar for inpatient care but different for outpatient care where caregivers spent more for transportation cost than food and lodging purpose (Table 2). Indeed, caregivers spent more when they accompanied the inpatients than the outpatients and this amount was almost 3.6 times higher than outpatients (BDT 3,490 or US$ 44.45 V/S BDT 975 or US$ 12.42).

Table 2.
Distribution of average caregivers’ cost of diarrheal treatment for tertiary level hospital (N = 801) BDT (US$).
3.3. Distribution of Caregivers’ Cost by Socio-Demographic Characteristics
Considering the age group of patients, the average total cost of caregivers ranged from BDT 2529 (US$ 32.22) to BDT 4407 (US$ 56.14) for inpatient care. For inpatient care, caregivers’ cost was significantly higher (BDT 4407 or US$ 56.14) when they accompanied under-five children followed by the older aged (64+) patients (BDT 3777 or US$ 48.11). A similar cost distributional pattern was observed regarding direct and indirect cost of caregivers for both the inpatient and outpatient care. Caregivers’ average total expenditure was slightly higher (BDT 3616 or US$ 46.06) for male patients than female patients (BDT 3357 or US$ 42.76), and a similar scenario was observed for direct and indirect cost for inpatient care (Table 3). However, this situation was quite different for outpatient care where cost of caregivers was comparatively higher for female out patients. In poorest quintile, the average total cost of caregivers for inpatients were BDT 3377 (US$ 43.02) while that for the richest quintile were BDT 3896 (US$ 49.62). The direct cost of caregivers for poorest quintile (BDT 379 or US$ 4.82) was lower than that of richest (5th) quintile (BDT 519 or US$ 6.61). A similar pattern was also observed for indirect costs (Table 3). However, such a pattern was not observed when they accompanied the patients for out-patient care.

Table 3.
Distribution of average care giver expenditure by socio-demographic characteristics (N = 801), BDT, US$.
3.4. Caregivers’ Time
The average time of caregivers during inpatient and outpatients care was 113 h and 7.8 h per episode respectively, while the caregiving time is higher when they accompanied inpatients (Figure 1). Furthermore, caregivers spent more time for caring under-five children as sometimes multiple caregivers attended during their course of treatment.
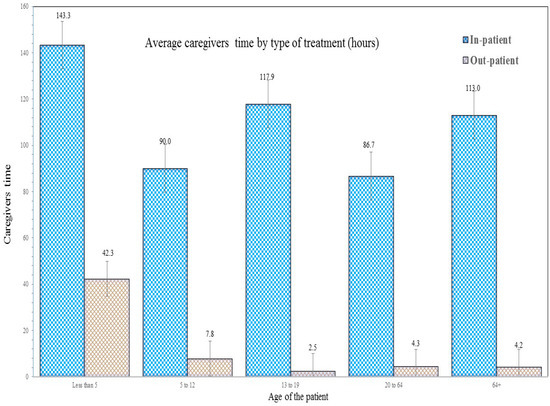
Figure 1.
Average caregivers’ time by type of treatment (h).
4. Discussion
Diarrheal diseases remain a crucial public health concern in Bangladesh as large number of people (approximately 2.7 million) utilize the healthcare facilities annually due to diarrheal infection, which leads to an excessive pressure on the country’s health system. Furthermore, households spend significant resources for the treatment purpose both directly and indirectly whereas caregivers’ expenditures and indirect cost are the important components of costs during the treatment courses. Caregivers’ support and services are vital for managing and treating patients particularly for under-five children and older aged and sometimes are especially essential when the patients felt difficulties to speak for him or herself [37]. Caregiving during diarrheal infections may help the patients for their daily assistance (e.g., dressing, toileting and child care), monitoring activities (e.g., financial transaction and administration of medication) and emotional support [38]. Caregivers’ help and support are often vital for inpatient cares which often associated with the caregivers’ burden both physically and economically [39]. In the present study we aimed to investigate the caregivers’ direct and indirect cost due to their attendance and supervision during the treatment of diarrheal patients in tertiary district public hospitals in Bangladesh.
Along with the health burden, diarrheal infections have potential economic impact on diarrhoea affected households. A number of studies focused on the economic burden of diarrheal infections in various countries [20,21,22,23,24,25], but the knowledge about caregivers costs of a full diarrheal episode are still limited in resource-poor settings, particularly in the context of Bangladesh. Various hospital-based costing studies were conducted in Bangladesh to estimate treatment cost per patients from the provider’s perspective [26,27]. However, those studies conducted either in a single public hospital or in a surveillance hospital. Further, all components of costs (e.g., income/productivity loss of patients, caregivers) were not included in their estimation. A multi-country analysis was conducted in ASEAN context focusing on childhood diarrhoea [40]. The study found that the mean household costs were US$ 1.82, US$ 6.47, and US$ 3.33 for Bangladesh, Pakistan, and India, respectively. However, the study excluded the treatment cost for adults and not explained the caregiver’s perspectives. Various slum-based diarrheal costing studies were also conducted in Bangladesh [41,42]. However, none of the above studies represented the country scenario or considered the cost burden from caregiver’s perspective. Our study demonstrated that the average total cost of caregivers was US$ 28.58 per diarrheal episode whereas the average total cost for caring inpatients and outpatient was US$ 44.45 and US$ 12.42, respectively. Our estimation suggested that annual caregivers’ cost during diarrheal infections to be US$ 74.71 million which constituted for 5.34% of the total health expenditure in Bangladesh [43]. The out of pocket cost incurred by the caregivers was mainly for purchasing foods and lodging purposes while a vast indirect cost was also incurred due to their absence from daily productive activities. An economic analysis regarding cost of caregivers of DAZT (diarrhoea alleviation through zinc and oral rehydration salts therapy) program was conducted in Gujrat, India and found that the average economic cost could be incurred up to US$ 4.04 per episode for rural under-five children [16]. Several studies also indicated that caregivers’ cost is important aspect for households which might be increased the total treatment cost during diarrheal episode from societal perspective [17,33,44,45]. An earlier study in this context observed that the additional caregiver cost could increase the average treatment costs up to US$ 110.51 per episode of diarrheal infection [17]. In our study we have found that caregivers’ cost was highest when they provided care to the under-five children as they were the most vulnerable for diarrheal infections [18,46]. In another earlier study to this context, it was shown that healthcare seeking behaviour of households were quite different regarding their young members when exposed diarrheal infections and they were often taken to the private providers or clinics (e.g., private practitioners) before hospitalization which was not observed for adult patients [33]. Furthermore, household members particularly parents became terrified and worried when they found their young family members are at risk of ill-health which is reflected in their direct and indirect costs as both the time and in-person involvement required are generally comparatively more for children than adult patients [19].
Like previous studies [17,19,33,44,45] we also observed that households from the poorest quintile spent less than richest quintile because of their affordability but faced highest cost burden than richest quintile although the diarrheal prevalence are the highest among household members of the poorest quintile [17,18]. For such consequences, many diarrheal cases are inadequately managed at household level which eventually pushes them to the point where the patients’ life is endangered [47]. An earlier study observed that during diarrheal episode households often sought care from formal (e.g., qualified doctor, hospital) and informal providers (e.g., tradition healers, unqualified village doctors), even about 23% of diarrheal patients did not seek formal care, although rapid and proper treatment is essential to avoid excessive costs of households and adverse health events [16,18]. Although we did not particularly capture the source of financing for caregivers, an earlier study indicated that regular income and borrowing were the two common coping strategies for diarrheal treatment, which is crucial for Bangladesh as the social health protection scheme not yet implemented and out-of-pocket is the main payment strategy (67%) for seeking healthcare [17,43].
There are various proven interventions for preventing diarrheal infections. However, the vast number of diarrheal cases could be prevented by implementing water, sanitation, and hygiene (WASH) strategies [48,49]. A couple of systematic reviews confirmed that hand washing [50] and point-of-use water treatment [51] were effective interventions for reducing diarrhoeal diseases. Cairncross and colleagues identified that the risk of diarrhoea could be reduced by implementing hand washing with soap (48%), improved water quality (17%) and adequate disposal of human waste (36%) in many developing countries [52]. Since diarrhoea is manifested by dehydration in most of the cases, ORS has proven as effective treatment without any significant adverse effect [53]; and as much as 69% of diarrhoea-related mortality could be prevented by administrating ORS and recommended home fluids [54] which contribute to decrease length of stay or even hospitalization thus reduces the excessive cost during diarrheal treatment. The promotion of exclusive breastfeeding [55], and complementary feeding practices [56] might strengthen the immune system of children and reduce the prevalence of childhood diarrhoea. Although WASH programs, such as improvements in water/sanitation infrastructure and personal hygiene contribute to decline the transmission of enteric pathogens, vaccine can hasten the waning of diarrhoea-related mortalities and morbidities, particularly in epidemic and endemic settings [57]. It was reported that nearly one-third of the episodes of severe diarrhoea could be prevented by introducing vaccination against rotavirus and cholera infections [58]. Policy makers should consider the caregivers cost found in our study for justifying the future diarrheal prevention programmes.
The study has some limitations when interpreting these findings. There may be some recall bias as data were collected after receiving treatment although we have tried to capture all the information within the two weeks of discharge from hospital. The limitations to this study also include the design; as a cross-sectional, hospital-based study it is unable to capture the seasonal variation of caregivers cost as the incidence of diarrheal disease usually peaks during the hot and winter seasons in Bangladesh [59]. The cost of caregivers relies heavily on households’ treatment seeking patterns, resources and ability to pay which were not captured [60]. Further, we could not compare the treatments cost using a pairwise matching approach due to the non-availability of matching data. Similarly, the present study was also unable to observe the cost of adverse effects and emotional effects (such as anxiety and tiredness) of caregivers during the diarrheal effects. All these issues should be taken into account in future research.
5. Conclusions
Diarrhoea is still an overwhelming public health issue in Bangladesh. Our study observed that the average cost of caregivers for treating each episode of diarrhoea was US$ 28.58 (BDT 2,243). Regarding the types of services, the caregivers spend almost 3.6 times higher for inpatient care than outpatients and caregivers’ cost was significantly higher when they accompanied under-five children and older aged patients. The study delivers empirical evidence for the health-care programmers and policy makers about the economic cost of caregivers during diarrheal treatment care. However, the additional caregivers’ cost is likely to be even higher than what has been observed in this empirical study. These findings should be taken into account in designing future diarrheal prevention programmes in Bangladesh and other developing countries.
Author Contributions
A.R.S. and M.S. conceptualized the study. A.R.S., M.S., N.A., and R.A. performed the data analysis and interpretation. A.R.S., M.S., N.A., R.A., K.A., J.A.M.K., and A.M. wrote the paper. A.R.S., M.S., K.A., J.A.M.K., and A.M. critically reviewed the final version. All authors approved the final version of the manuscript.
Funding
The project is a part of the SIDA young investigator award.
Acknowledgments
icddr,b is thankful to the Governments of Australia, Bangladesh, Canada, Sweden, and the U.K. for providing core/unrestricted support. We would like to thank Health Economics and Financing Research Group of icddr,b for their earlier comments on this research.
Conflicts of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Fullman, N.; Yearwood, J.; Abay, S.M.; Abbafati, C.; Abd-Allah, F.; Abdela, J.; Zuhlke, L.J.; Murray, C.J.L.; Lozano, R. Measuring performance on the Healthcare Access and Quality Index for 195 countries and territories and selected subnational locations: A systematic analysis from the Global Burden of Disease Study 2016. Lancet 2018. [Google Scholar] [CrossRef]
- Vos, T.; Allen, C.; Arora, M.; Barber, R.M.; Bhutta, Z.A.; Brown, A.; Zhou, M.; Zodpey, S.; Liesl, J.; Murray, C.J.L. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1545–1602. [Google Scholar] [CrossRef]
- UNICEF. Diarrhoea Remains a Leading Killer of Young Children, Despite the Availability of a Simple Treatment Solution. In UNICEF DATA: Monitoring the Situation of Children and Women. 2016, p. 1. Available online: http://data.unicef.org/child-health/diarrhoeal-disease.html (accessed on 28 June 2016).
- Mashoto, K.O.; Malebo, H.M.; Msisiri, E.; Peter, E. Prevalence, one week incidence and knowledge on causes of diarrhea: Household survey of under-fives and adults in Mkuranga district, Tanzania. BMC Public Health 2014, 14, 985. [Google Scholar] [CrossRef] [PubMed]
- MOHFW. Health Bulletin 2017; MOHFW: Dhaka, Bangladesh, 2017. Available online: www.dghs.gov.bd (accessed on 15 November 2018).
- Bangladesh Bureau of Statistics. Health and Morbidity Status Survey—2012; Bangladesh Bureau of Statistics: Dhaka, Bangladesh, 2013.
- Streatfield, P.K.; Baumgartner, J. Bangladesh Urban Health Survey. Dhaka, Bangladesh, 2013. Available online: http://www.niport.gov.bd/wp-content/uploads/download/1413705060-UHS2013Preliminary Results.pdf (accessed on 15 November 2018).
- Drasar, B.S.; Tomkins, A.M.; Feacham, R.G. Seasonal Aspects of Diarrhoeal Disease. Seasonal Dimensions to Rural Poverty; Report to UK Overseas Development Association; London School of Hygiene and Tropical Medicine: London, UK, 1978. [Google Scholar]
- Black, R.E.; Lanata, C.F. Epidemiology of diarrhoeal diseases in developing countries. In Infections of the Gastrointestinal Tract; Blaser, M.J., Smith, P.D., Ravdin, J.I., Greenberg, H.P., Guerrant, R.I., Eds.; Raven Press: New York, NY, USA, 1995. [Google Scholar]
- Ozguler, M. Febril Neutropenia: An Approach as an Infectious Disease Specialist; Scientific Research Publishing, Inc.: Wuhan, China, 2015; Available online: www.scirp.org (accessed on 15 November 2018).
- Deen, J.L.; Seidlein, L.; Sur, D.; Agtini, M.; Lucas, M.; Lopez, A.N.; Lopez, L.; Deok, R.K.; Ali, M.; Clemens, J.D. The High Burden of Cholera in Children: Comparison of Incidence from Endemic Areas in Asia and Africa. PLoS Negl. Trop. Dis. 2008, 2. [Google Scholar] [CrossRef] [PubMed]
- Rabbani, G.H.; Larson, C.P.; Islam, R.; Saha, U.R.; Kabir, A. Green banana-supplemented diet in the home management of acute and prolonged diarrhoea in children: A community-based trial in rural Bangladesh. Trop. Med. Int. Health 2010, 15, 1132–1139. [Google Scholar] [CrossRef] [PubMed]
- Lamberti, L.M.; Walker, F.C.L.; Black, R. Systematic review of diarrhea duration and severity in children and adults in low- and middle-income countries. BMC Public Health 2012, 12, 2–11. [Google Scholar] [CrossRef]
- Gebru, T.; Taha, M.; Kassahun, W. Risk factors of diarrhoeal disease in under-five children among health extension model and non-model families in Sheko district rural community, Southwest Ethiopia: Comparative cross-sectional study. BMC Public Health 2014, 14, 395. [Google Scholar] [CrossRef] [PubMed]
- Sultana, M.; Mahumud, R.A.; Sarker, A.R. Emerging Patterns of Mortality and Morbidity in District Level Hospitals in Bangladesh. Ann. Public Health Res. 2015, 2, 2–4. [Google Scholar]
- Shillcutt, S.D.; Lefevre, A.E.; Walker, C.L.F.; Taneja, S.; Black, R.E.; Mazumder, S. Economic costs to caregivers of diarrhoea treatment among children below 5 in rural Gujarat India: Findings from an external evaluation of the DAZT programme. Health Policy Plan. 2016, 31, 1411–1422. [Google Scholar] [CrossRef] [PubMed]
- Sarker, A.R.; Sultana, M.; Mahumud, R.A.; Ali, N.; Huda, T.M.; Salim uzzaman, M.; Haider, S.; Rahman, H.; Islam, Z.; Khan, J.A.M.; et al. Economic costs of hospitalized diarrheal disease in Bangladesh: A societal perspective. Glob. Health Res. Policy 2018, 3, 1. [Google Scholar] [CrossRef]
- Sarker, A.R.; Sultana, M.; Mahumud, R.A.; Sheikh, N.; Van Der Meer, R.; Morton, A. Prevalence and Health Care–Seeking Behavior for Childhood Diarrheal Disease in Bangladesh. Glob. Pediatr. Health 2016, 3, 2333794X1668090. [Google Scholar] [CrossRef] [PubMed]
- Yaprak, S.; Bulut, U.; Okudan, Y.E.; Gokdemir, O.; Colak, M.; Yıldırım, E.; Guldal, D. Caregiver reasons for tertiary health-care seeking for children aged ≤12 years. Pediatr. Int. 2016, 58, 1037–1041. [Google Scholar] [CrossRef] [PubMed]
- Burke, R.M.; Rebolledo, P.A.; Embrey, S.R.; Wagner, L.D.; Cowden, C.L.; Kelly, F.M.; Smith, E.R.; Iñiguez, V.; Leon, J.S. The burden of pediatric diarrhea: A cross-sectional study of incurred costs and perceptions of cost among Bolivian families. BMC Public Health 2013, 13, 708. [Google Scholar] [CrossRef] [PubMed]
- Kosek, M.; Bern, C.; Guerrant, R.L. The global burden of diarrhoeal disease, as estimated from studies published between 1992 and 2000. Bull. World Health Organ. 2003, 81, 197–204. [Google Scholar] [CrossRef] [PubMed]
- Bartsch, S.M.; Lee, B.Y. Economics and financing of vaccines for diarrheal diseases. Hum. Vaccine Immunother. 2014, 10, 1568–1581. [Google Scholar] [CrossRef]
- MacIntyre, U.; Villiers, F. Economic Burden of Diarrheal Disease in a Tertiary Level Hospital, Gauteng, South Africa. J. Infect. Dis. 2010, 202, 116–125. [Google Scholar] [CrossRef] [PubMed]
- Bhuiyan, M.U.; Luby, S.P.; Zaman, R.U.; Rahman, M.W.; Sharker, M.A.Y.; Hossain, M.J.; Rasul, C.H.; Ekram, A.R.M.S.; Rahman, M.; Sturm-Ramirez, K.; et al. Incidence of and Risk Factors for Hospital-Acquired Diarrhea in Three Tertiary Care Public Hospitals in Bangladesh. Am. J. Trop. Med. Hyg. 2014, 91, 165–172. [Google Scholar] [CrossRef] [PubMed]
- Pham-Duc, P.; Nguyen-Viet, H.; Hattendorf, J.; Cam, P.D.; Zurbrügg, C.; Zinsstag, J.; Odermatt, P. Diarrhoeal diseases among adult population in an agricultural community Hanam province, Vietnam, with high wastewater and excreta re-use. BMC Public Health 2014, 14, 978. [Google Scholar] [CrossRef]
- Ali, Q.L. Calculation of Total Unit Cost for Diarrhoeal Management at District and Thana Health Complex; Ministry of Health and Family Welfare: Dhaka, Bangladesh, 2001.
- Das, J.; Das, S.K.; Ahmed, S.; Ferdous, F.; Farzana, F.D.; Sarker, M.H.R.; Ahmed, M.S.; Chisti, M.J.; Malek, M.; Rahman, A.; et al. Determinants of percent expenditure of household income due to childhood diarrhoea in rural Bangladesh. Epidemiol. Infect. 2015, 143, 2700–2706. [Google Scholar] [CrossRef] [PubMed]
- Chitunhu, S.; Musenge, E. Direct and indirect determinants of childhood malaria morbidity in Malawi: A survey cross—Sectional analysis based on malaria indicator survey data for 2012. Malaria J. 2015, 14, 265. [Google Scholar] [CrossRef] [PubMed]
- Sur, D.; Chatterjee, S.; Riewpaiboon, A.; Manna, B.; Kanungo, S.; Bhattacharya, S.K. Treatment cost for typhoid fever at two hospitals in Kolkata, India. J. Health Popul. Nutr. 2009, 27, 725–732. [Google Scholar] [PubMed]
- Poulos, C.; Riewpaiboon, A.; Stewart, J.F.; Clemens, J.; Guh, S.; Agtini, M.; Sur, D.; Islam, Z.; Lucas, M.; Whittington, D. Costs of illness due to endemic cholera. Epidemiol. Infect. 2012, 140, 500–509. [Google Scholar] [CrossRef] [PubMed]
- Drummond, M.; Sculpher, M.J.; Laxton, K.C.; Stoddart, G.L.; Torrance, G.W. Methods for the Economic Evaluation of Health Care Programmes, 3rd ed.; Oxford University Press: Oxford, UK, 2005. [Google Scholar]
- Van Roijen, L.; Essink-Bot, M.L.; Koopmanschap, M.A.; Bonsel, G.; Rutten, F.F. Labor and health status in economic evaluation of health care. The Health and Labor Questionnaire. Int. J. Technol. Assess. Health Care 1996, 12, 405–415. [Google Scholar] [CrossRef]
- Sarker, A.R.; Islam, Z.; Khan, I.A.; Saha, A.; Chowdhury, F.; Khan, A.I.; Qadri, F.; Khan, J.A.M. Cost of illness for cholera in a high risk urban area in Bangladesh: An analysis from household perspective. BMC Infect. Dis. 2013, 13, 518. [Google Scholar] [CrossRef] [PubMed]
- Rice, D.P. Estimating cost of illness. Am. J. Public Health Nations Health 1967, 57, 424–440. [Google Scholar] [CrossRef] [PubMed]
- Chima, R.I.; Goodman, C.A.; Mills, A. The economic impact of malaria in Africa: A critical review of the evidence. Health Policy 2003, 63, 17–36. [Google Scholar] [CrossRef]
- GOB. Monthly Report on Fiscal-Macro Position. Dhaka, Bangladesh, 2016. Available online: http://www.mof.gov.bd/en/budget/mfmu/mfmu_February_16.pdf (accessed on 15 November 2018).
- Alwin, J.; Öberg, B.; Krevers, B. Support/services among family caregivers of persons with dementia—Perceived importance and services received. Int. J. Geriatr. Psychiatry 2010, 25, 240–248. [Google Scholar] [CrossRef]
- Chaudhuri, J.D.; Das, S. The role of caregivers in the management of alzheimer’s disease: Examples from Asian countries. Sultan Qaboos Univ. Med. J. 2006, 6, 11–18. [Google Scholar]
- Haro, J.M.; Kahle-Wrobleski, K.; Bruno, G.; Belger, M.; Dell’Agnello, G.; Dodel, R.; Jones, R.W.; Reed, C.C.; Vellas, B.; Wimo, A.; et al. Analysis of burden in caregivers of people with Alzheimer’s disease using self-report and supervision hours. J. Nutr. Aging 2014, 18, 677–684. [Google Scholar] [CrossRef]
- Rheingans, R.; Kukla, M.; Faruque, A.S.G.; Sur, D.; Zaidi, A.K.M.; Nasrin, D.; Farag, T H.; Levine, M.; Kotloff, K. Determinants of Household Costs Associated With Childhood Diarrhea in 3 South Asian Settings. Clin. Infect. Dis. 2012, 55, 327–335. [Google Scholar] [CrossRef]
- Sultana, S.; Ahmed, S.; Hossen, S.S. Diarrhoeal Diseases in the Slums of Khulna City: Prevalence and Cost Analysis. J. Asian Dev. Stud. 2013, 2, 60–70. [Google Scholar]
- Halim, F.B.; Haider, M.Z. Prevalence and economic costs of diarrheal illness among adult slum dwellers in Khulna City, Bangladesh. J. Health Soc. Sci. 2017, 120, 83–98. [Google Scholar] [CrossRef]
- MOHFW. Bangladesh National Health Accounts 1997–2015: Preliminary Results; MOHFW: Dhaka, Bangladesh, 2015. Available online: http://www.thedailystar.net/backpage/people-fork-out-most-1465246 (accessed on 15 November 2018).
- Poulos, C.; Riewpaiboon, A.; Stewart, J.F.; Clemens, J.; Guh, S.; Agtini, M.; Anh, D.D.; Dong, B.; Bhutta, Z.; Sur, D.; et al. Cost of illness due to typhoid fever in five Asian countries. Trop. Med. Int. Health 2011, 16, 314–323. [Google Scholar] [CrossRef] [PubMed]
- Sarker, A.R.; Sultana, M.; Mahumud, R.A.; Van Der Meer, R.; Morton, A.; Sarker, A.R. Cost-effectiveness analysis of introducing universal childhood rotavirus vaccination in Bangladesh. Hum. Vaccines Immunother. 2017, 14, 189–198. [Google Scholar] [CrossRef]
- IVI. Country Investment Case Study on Cholera Vaccination: Bangladesh; IVI: Seoul, Korea, 2013; Available online: http://www.ivi.int/web/www/0403 (accessed on 15 November 2018).
- Chowdhury, F.; Khan, I.A.; Patel, S.; Siddiq, A.U.; Saha, N.C.; Khan, A.I.; Saha, A.; Cravioto, A.; Clemens, J.; Qadri, F.; et al. Diarrheal illness and healthcare seeking behavior among a population at high risk for diarrhea in Dhaka, Bangladesh. PLoS ONE 2015, 10, e0130105. [Google Scholar] [CrossRef]
- Bhutta, Z.A.; Das, J.K.; Walker, N.; Rizvi, A.; Campbell, H.; Rudan, I.; Black, R.E. Interventions to address deaths from childhood pneumonia and diarrhoea equitably: What works and at what cost? Lancet 2013, 381, 1417–1429. [Google Scholar] [CrossRef]
- Diouf, K.; Tabatabai, P.; Rudolph, J.; Marx, M. Diarrhoea prevalence in children under five years of age in rural Burundi: An assessment of social and behavioural factors at the household level. Glob. Health Act. 2014, 7, 24895. [Google Scholar] [CrossRef]
- Ejemot-Nwadiaro, R.I.; Ehiri, J.E.; Arikpo, D.; Meremikwu, M.M.; Critchley, J.A. Hand washing promotion for preventing diarrhoea. Cochrane Database Syst Rev. 2015. [Google Scholar] [CrossRef]
- Clasen, T.; Roberts, I.; Rabie, T.; Schmidt, W.; Cairncross, S. Interventions to improve water quality for preventing diarrhoea. Cochrane Database Syst. Rev. 2006, 3, CD004794. [Google Scholar]
- Cairncross, S.; Hunt, C.; Boisson, S.; Bostoen, K.; Curtis, V.; Fung, I.C.H.; Schmidt, W.P. Water, sanitation and hygiene for the prevention of diarrhoea. Int. J. Epidemiol. 2010, 39, i193–i205. [Google Scholar] [CrossRef]
- Ruxin, J.N. Magic bullet: The history of oral rehydration therapy. Med. Hist. 1994, 38, 363–397. [Google Scholar] [CrossRef] [PubMed]
- Munos, M.K.; Fischer Walker, C.L.; Black, R.E. The effect of oral rehydration solution and recommended home fluids on diarrhoea mortality. Int. J. Epidemiol. 2010, 39, i75–i87. [Google Scholar] [CrossRef] [PubMed]
- WHO Collaborative Study Team. Effect of breastfeeding on infant and child mortality due to infectious diseases in less developed countries: A pooled analysis. Lancet 2000, 355, 451–455. [Google Scholar] [CrossRef]
- Jones, G.; Steketee, R.W.; Black, R.E.; Bhutta, Z.A.; Morris, S.S. How many child deaths can we prevent this year? Lancet 2003, 362, 65–71. [Google Scholar] [CrossRef]
- Levine, M.M.; Kotloff, K.L.; Nataro, J.P.; Muhsen, K. The Global Enteric Multicenter Study (GEMS): Impetus, rationale, and genesis. Clin. Infect. Dis. 2012, 55, 215–224. [Google Scholar] [CrossRef]
- Fischer Walker, C.L.; Rudan, I.; Liu, L.; Nair, H.; Theodoratou, E.; Bhutta, Z.A.; O’Brien, K.L.; Campbell, H.; Black, R.E. Global burden of childhood pneumonia and diarrhoea. Lancet 2013, 381, 1405–1416. [Google Scholar] [CrossRef]
- Das, S.K.; Begum, D.; Ahmed, S.; Ferdous, F.; Farzana, F.D.; Chisti, M.J.; Latham, J.R.; Talukder, K.A.; Rahman, M.M.; et al. Geographical diversity in seasonality of major diarrhoeal pathogens in Bangladesh observed between 2010 and 2012. Epidemiol. Infect. 2014, 142, 2530–2541. [Google Scholar] [CrossRef] [PubMed]
- Aikins, M.; Armah, G.; Akazili, J.; Hodgson, A. Hospital health care cost of diarrheal disease in Northern Ghana. J. Infect. Dis. 2010, 202 (Suppl. 1), S126–S130. [Google Scholar] [CrossRef]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).