Long-Range Diagnosis of and Support for Skin Conditions in Field Settings
Abstract
1. Introduction
2. Types of Mobile Health (mHealth) and Telemedicine Tools
3. Benefits and Practical Applications of eHealth Tools
4. Challenges and Barriers to Use of Teledermatology
5. Practical Tips for Implementation of a New Teledermatology Initiative
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Karimkhani, C.; Dellavalle, R.P.; Coffeng, L.E.; Flohr, C.; Hay, R.J.; Langan, S.M.; Nsoesie, E.O.; Ferrari, A.J.; Erskine, H.E.; Silverberg, J.I.; et al. Global skin disease morbidity and mortality: An update from the Global Burden of Disease Study 2013. JAMA Dermatol. 2017, 153, 406. [Google Scholar] [CrossRef] [PubMed]
- Evans, T.; Chen, L.; Evans, D.; Sadana, R.; Stilwell, B.; Travis, O.; Van Lerberghe, W.; Zurn, P.; Aschwanden, C. The World Health Report 2006 - Working Together for Health; World Health Organization: Geneva, Switzerland, 2006; ISBN 978-92-4-156317-8. [Google Scholar]
- Chen, L.; Evans, T.; Anand, S.; Boufford, J.I.; Brown, H.; Chowdhury, M.; Cueto, M.; Dare, L.; Dussault, G.; Elzinga, G.; et al. Human resources for health: Overcoming the crisis. Lancet 2004, 364, 1984–1990. [Google Scholar] [CrossRef]
- Crisp, N.; Chen, L. Global supply of health professionals. N. Engl. J. Med. 2014, 370, 950–957. [Google Scholar] [CrossRef] [PubMed]
- Desai, B.; McKoy, K.; Kovarik, C. Overview of international teledermatology. Pan Afr. Med. J. 2010, 6, 3. [Google Scholar] [CrossRef] [PubMed]
- International Foundation for Dermatology International Foundation for Dermatology. Available online: http://www.ifd.org/about2.html (accessed on 20 June 2018).
- Hay, R.J.; Johns, N.E.; Williams, H.C.; Bolliger, I.W.; Dellavalle, R.P.; Margolis, D.J.; Marks, R.; Naldi, L.; Weinstock, M.A.; Wulf, S.K.; et al. The global burden of skin disease in 2010: An analysis of the prevalence and impact of skin conditions. J. Investig. Dermatol. 2014, 134, 1527–1534. [Google Scholar] [CrossRef] [PubMed]
- WHO Global Observatory for eHealth. Global Diffusion of eHealth: Making Universal Health Coverage Achievable: Report of the Third Global Survey on eHealth; World Health Organization: Geneva, Switzerland, 2016; ISBN 978-92-4-151178-0. [Google Scholar]
- Groupe Speciale Mobile Association. The Mobile Economy 2014; GSMA & International Telecomm Union: London, UK, 2014. [Google Scholar]
- Lipoff, J.B.; Cobos, G.; Kaddu, S.; Kovarik, C.L. The Africa Teledermatology Project: A retrospective case review of 1229 consultations from sub-saharan Africa. J. Am. Acad. Dermatol. 2015, 72, 1084–1085. [Google Scholar] [CrossRef] [PubMed]
- Wootton, R.; Geissbuhler, A.; Jethwani, K.; Kovarik, C.; Person, D.A.; Vladzymyrskyy, A.; Zanaboni, P.; Zolfo, M. Long-running telemedicine networks delivering humanitarian services: Experience, performance and scientific output. Bull. World Health Organ. 2012, 90, 341D–347D. [Google Scholar] [CrossRef] [PubMed]
- Kaddu, S.; Kovarik, C.; Gabler, G.; Soyer, H. Teledermatology in Developing Countries. In Telehealth in the Developing World; Royal Society of Medicine Press/IDRC: London, UK, 2009; ISBN 978-1-85315-784. [Google Scholar]
- Delaigue, S.; Morand, J.J.; Olson, D.; Wootton, R.; Bonnardot, L. Teledermatology in low-resource settings: The MSF experience with a multilingual tele-expertise platform. Front. Public Health 2014, 2. [Google Scholar] [CrossRef] [PubMed]
- Bagayoko, C.O.; Müller, H.; Geissbuhler, A. Assessment of internet-based tele-medicine in Africa (the RAFT project). Comput. Med. Imaging Graph. 2006, 30, 407–416. [Google Scholar] [CrossRef] [PubMed]
- Clickmedix. Available online: https://clickmedix.com/ (accessed on 1 July 2018).
- Azova. Available online: http://azovahealth.com/ (accessed on 1 July 2018).
- Proton Mail. Available online: https://protonmail.com/ (accessed on 1 July 2018).
- Tutanota. Available online: https://tutanota.com/ (accessed on 1 July 2018).
- Dropbox Business and HIPAA/HITECH—An Overview. Available online: https://www.dropbox.com/help/security/hipaa-hitech-overview (accessed on 20 June 2018).
- Google Drive. Available online: https://www.google.com/drive/ (accessed on 1 July 2018).
- Microsoft OneDrive. Available online: https://onedrive.live.com/about/en-us/ (accessed on 1 July 2018).
- Box. Available online: https://www.box.com/home (accessed on 1 July 2018).
- Williams, V.; Kovarik, C. WhatsApp: An innovative tool for dermatology care in limited resource settings. Telemed. e-Health 2018, 24, 464–468. [Google Scholar] [CrossRef] [PubMed]
- Mars, M.; Scott, R.E. WhatsApp in clinical practice: A literature review. Stud. Health Technol. Inform. 2016, 231, 82–90. [Google Scholar] [PubMed]
- Medtunnel. Available online: http://www.medtunnel.com/ (accessed on 1 July 2018).
- Bloomtext. Available online: https://www.bloomtext.com/#/ (accessed on 1 July 2018).
- Imprivata. Available online: https://www.imprivata.com/secure-communications (accessed on 20 June 2018).
- Tiger Connect. Available online: https://www.tigerconnect.com/ (accessed on 20 June 2018).
- Voalte. Available online: http://www.voalte.com/healthcare-communication-platform-2 (accessed on 20 June 2018).
- Qliqsoft. Available online: https://www.qliqsoft.com/ (accessed on 1 July 2018).
- Spok Mobile. Available online: https://www.spok.com/spok-mobile (accessed on 1 July 2018).
- Telederm.org. Available online: http://www.telederm.org/ (accessed on 20 June 2018).
- Sermo. Available online: http://www.sermo.com/ (accessed on 20 June 2018).
- Facebook. Available online: https://www.facebook.com/ (accessed on 20 June 2018).
- Olympus VS120-S6-W Virtual Slide Microscope. Available online: www.olympus lifescience.com/Microscopes /VC120 (accessed on 1 July 2018).
- ZEISS Axio Scan.Z1 Digital Slide Scanner. Available online: https://www.zeiss.com/microscopy/int/products/imaging-systems/axio-scan-z1.html (accessed on 1 July 2018).
- Leica Biosystems Aperio AT2 Telepathology Platform. Available online: https://www.leicabiosystems.com/digital-pathology/scan/aperio-at2/ (accessed on 1 July 2018).
- Leica Biosystems Aperio LV1 Telepathology Platform. Available online: www.leicabiosystems.com/Aperio/LV1 (accessed on 1 July 2018).
- 3DHISTECH Pannoramic DESK II DW. Available online: https://www.3dhistech.com/pannoramic_desk_II_DW (accessed on 1 July 2018).
- Lab Cam. Available online: https://www.ilabcam.com/ (accessed on 1 July 2018).
- Magnifi. Available online: http://www.arcturuslabs.com (accessed on 1 July 2018).
- Snapzoom. Available online: http://snapzooms.com (accessed on 1 July 2018).
- Ismail, A.; McMichael, J.R.; Stoff, B.K. Utility of international store-and-forward teledermatopathology among a cohort of mostly female patients at a tertiary referral center in Afghanistan. Int. J. Womens Dermatol. 2018, 4, 83–86. [Google Scholar] [CrossRef] [PubMed]
- Bobbs, M.; Bayer, M.; Frazer, T.; Humphrey, S.; Wilson, B.; Olasz, E.; Holland, K.; Kuzminski, J. Building a global teledermatology collaboration. Int. J. Dermatol. 2016, 55, 446–449. [Google Scholar] [CrossRef] [PubMed]
- Brauchli, K.; Jagilly, R.; Oberli, H.; Kunze, K.D.; Phillips, G.; Hurwitz, N.; Oberholzer, M. Telepathology on the Solomon Islands—two years’ experience with a hybrid web- and email-based telepathology System. J. Telemed. Telecare 2004, 10, 14–17. [Google Scholar] [CrossRef] [PubMed]
- Yueng, K. Whatsapp Passes 1 Billion Monthly Active Users. Venture Beat 2016. Available online: https://venturebeat.com/2016/02/01/whatsapp-passes-1-billion-monthly-active-users/ (accessed on 20 June 2018).
- Monegian, B. KLAS Names Top Secure Messaging Tools. Healthcare IT News 2015. Available online: https://www.healthcareitnews.com/news/tigertext-leads-messaging-market-now (accessed on 20 June 2018).
- Kohgadai, A. Top 5 HIPAA-Compliant Cloud Storage Services. Cloud Security Blog. Available online: https://www.skyhighnetworks.com/cloud-security-blog/top-5-hipaa-compliant-cloud-storage-services/ (accessed on 20 June 2018).
- Saleh, N.; Abdel Hay, R.; Hegazy, R.; Hussein, M.; Gomaa, D. Can teledermatology be a useful diagnostic tool in dermatology practice in remote areas? An Egyptian experience with 600 patients. J. Telemed. Telecare 2017, 23, 233–238. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Romero, M.T.; Prado, F.; Dominguez-Cherit, J.; Hojyo-Tomomka, M.T.; Arenas, R. Teledermatology via a social networking web site: A pilot study between a general hospital and a rural clinic. Telemed. e-Health 2011, 17, 652–655. [Google Scholar] [CrossRef] [PubMed]
- Meyer, J.; Paré, G. Telepathology Impacts and Implementation Challenges: A Scoping Review. Arch. Pathol. Lab. Med. 2015, 139, 1550–1557. [Google Scholar] [CrossRef] [PubMed]
- Roy, S.; Pantanowitz, L.; Amin, M.; Seethala, R.R.; Ishtiaque, A.; Yousem, S.A.; Parwani, A.V.; Cucoranu, I.; Hartman, D.J. Smartphone adapters for digital photomicrography. J. Pathol. Inform. 2014, 5, 24. [Google Scholar] [CrossRef] [PubMed]
- Bellina, L.; Missoni, E. Mobile cell-phones (M-phones) in telemicroscopy: Increasing connectivity of isolated laboratories. Diagn. Pathol. 2009, 4, 19. [Google Scholar] [CrossRef] [PubMed]
- Abdirad, A.; Sarrafpour, B.; Ghaderi-Sohi, S. Static telepathology in Cancer Institute of Tehran University: Report of the first academic experience in Iran. Diagn. Pathol. 2006, 1, 33. [Google Scholar] [CrossRef] [PubMed]
- Desai, S.; Patil, R.; Chinoy, R.; Kothari, A.; Ghosh, T.K.; Chavan, M.; Mohan, A.; Nene, B.M.; Dinshaw, K.A. Experience with telepathology at a tertiary cancer centre and a rural cancer hospital. Natl. Med. J. India 2004, 17, 17–19. [Google Scholar] [PubMed]
- Evans, A.; Garcia, B.; Godin, C.; Godlewski, M.; Jansen, G.; Kabani, A.; Louahlia, S.; Manning, L.; Maung, R.; Moore, L.; et al. Guidelines from the Canadian Association of Pathologists for establishing a telepathology service for anatomic pathology using whole-slide imaging. J. Pathol. Inform. 2014, 5, 15. [Google Scholar] [CrossRef] [PubMed]
- Kayser, K. Introduction of virtual microscopy in routine surgical pathology--a hypothesis and personal view from Europe. Diagn. Pathol. 2012, 7, 48. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, R.S.; Graham, A.R.; Richter, L.C.; Barker, G.P.; Krupinski, E.A.; Lopez, A.M.; Erps, K.A.; Bhattacharyya, A.K.; Yagi, Y.; Gilbertson, J.R. Overview of telepathology, virtual microscopy, and whole slide imaging: Prospects for the future. Hum. Pathol. 2009, 40, 1057–1069. [Google Scholar] [CrossRef] [PubMed]
- Fischer, M.K.; Kayembe, M.K.; Scheer, A.J.; Introcaso, C.E.; Binder, S.W.; Kovarik, C.L. Establishing telepathology in Africa: Lessons from Botswana. J. Am. Acad. Dermatol. 2011, 64, 986–987. [Google Scholar] [CrossRef] [PubMed]
- Pantanowitz, L.; Farahani, N.; Parwani, A. Whole Slide Imaging in Pathology: Advantages, Limitations, and Emerging Perspectives. Pathol. Lab. Med. Int. 2015, 23. [Google Scholar] [CrossRef]
- Pantanowitz, L. Digital images and the future of digital pathology. J. Pathol. Inform. 2010, 1, 15. [Google Scholar] [CrossRef] [PubMed]
- Evans, A.J.; Chetty, R.; Clarke, B.A.; Croul, S.; Ghazarian, D.M.; Kiehl, T.R.; Perez Ordonez, B.; Ilaalagan, S.; Asa, S.L. Primary frozen section diagnosis by robotic microscopy and virtual slide telepathology: The University Health Network experience. Hum. Pathol. 2009, 40, 1070–1081. [Google Scholar] [CrossRef] [PubMed]
- Al Habeeb, A.; Ghazarian, D.; Evans, A. Virtual microscopy using whole-slide imaging as an enabler for teledermatopathology: A paired consultant validation study. J. Pathol. Inform. 2012, 3, 2. [Google Scholar] [CrossRef] [PubMed]
- Al-Janabi, S.; Huisman, A.; Vink, A.; Leguit, R.J.; Offerhaus, G.J.A.; ten Kate, F.J.W.; van Dijk, M.R.; van Diest, P.J. Whole slide images for primary diagnostics in dermatopathology: A feasibility study. J. Clin. Pathol. 2012, 65, 152–158. [Google Scholar] [CrossRef] [PubMed]
- Kent, M.N.; Olsen, T.G.; Feeser, T.A.; Tesno, K.C.; Moad, J.C.; Conroy, M.P.; Kendrick, M.J.; Stephenson, S.R.; Murchland, M.R.; Khan, A.U.; et al. Diagnostic accuracy of virtual pathology vs. traditional microscopy in a large dermatopathology study. JAMA Dermatol. 2017, 153, 1285. [Google Scholar] [CrossRef] [PubMed]
- Koch, L.H.; Lampros, J.N.; Delong, L.K.; Chen, S.C.; Woosley, J.T.; Hood, A.F. Randomized comparison of virtual microscopy and traditional glass microscopy in diagnostic accuracy among dermatology and pathology residents. Hum. Pathol. 2009, 40, 662–667. [Google Scholar] [CrossRef] [PubMed]
- Molin, J.; Thorstenson, S.; Lundström, C. Implementation of large-scale routine diagnostics using whole slide imaging in Sweden: Digital pathology experiences 2006–2013. J. Pathol. Inform. 2014, 5, 14. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, P.S.; Lindebjerg, J.; Rasmussen, J.; Starklint, H.; Waldstrøm, M.; Nielsen, B. Virtual Microscopy: An Evaluation of its Validity and Diagnostic Performance in Routine Histologic Diagnosis of Skin Tumors. Hum. Pathol. 2010, 41, 1770–1776. [Google Scholar] [CrossRef] [PubMed]
- Shah, K.K.; Lehman, J.S.; Gibson, L.E.; Lohse, C.M.; Comfere, N.I.; Wieland, C.N. Validation of diagnostic accuracy with whole-slide imaging compared with glass slide review in dermatopathology. J. Am. Acad. Dermatol. 2016, 75, 1229–1237. [Google Scholar] [CrossRef] [PubMed]
- Wamala, D.; Katamba, A.; Dworak, O. Feasibility and diagnostic accuracy of internet-based dynamic telepathology between Uganda and Germany. J. Telemed. Telecare 2011, 17, 222–225. [Google Scholar] [CrossRef] [PubMed]
- Della Mea, V.; Cortolezzis, D.; Beltrami, C.A. The economics of telepathology-a case study. J. Telemed. Telecare 2000, 6 (Suppl. 1), S168–S169. [Google Scholar] [PubMed]
- Dudas, R.; VandenBussche, C.; Baras, A.; Ali, S.Z.; Olson, M.T. Inexpensive Telecytology solutions that use the Raspberry Pi and the iPhone. J. Am. Soc. Cytopathol. 2014, 3, 49–55. [Google Scholar] [CrossRef]
- Meléndez-Álvarez, B.; Robayo, O.; Gil-Guillén, V.; Carratalá-Munuera, M. Design and validation of a low-cost telepathology system. Telemedicine e-Health 2017, 23, 976–982. [Google Scholar] [CrossRef] [PubMed]
- Klock, C.; Gomes, R. Web conferencing systems: Skype and MSN in telepathology. Diagn. Pathol. 2008, 3, S13. [Google Scholar] [CrossRef] [PubMed]
- Sirintrapun, S.; Cimic, A. Dynamic nonrobotic telemicroscopy via Skype: A cost effective solution to teleconsultation. J. Pathol. Inform. 2012, 3, 28. [Google Scholar] [CrossRef] [PubMed]
- Speiser, J.J.; Hughes, I.; Mehta, V.; Wojcik, E.M.; Hutchens, K.A. Mobile teledermatopathology: Using a tablet PC as a novel and cost-efficient method to remotely diagnose dermatopathology cases. Am. J. Dermatopathol. 2014, 36, 54–57. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.; Gao, F.; Jiang, L.; Ma, S. Development of a whole slide imaging system on smartphones and evaluation with frozen section samples. JMIR mHealth uHealth 2017, 5, e132. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.N.; Peng, X.C.; Ma, S.; Yu, H.; Jin, Y.B.; Zheng, J.; Fu, G.H. Development of whole slide imaging on smartphones and evaluation with ThinPrep cytology test samples: Follow-up study. JMIR mHealth uHealth 2018, 6, e82. [Google Scholar] [CrossRef] [PubMed]
- Randriambelonoro, M.; Bagayoko, C.O.; Geissbuhler, A. Telemedicine as a tool for digital medical education: A 15-year journey inside the RAFT network. Digital medical education using the RAFT network. Ann. N. Y. Acad. Sci. 2018. [Google Scholar] [CrossRef] [PubMed]
- Mosa, A.S.M.; Yoo, I.; Sheets, L. A systematic review of healthcare applications for smartphones. BMC Med. Inform. Decis. Mak. 2012, 12. [Google Scholar] [CrossRef] [PubMed]
- Dynamed. Available online: https://dynamed.com/home/ (accessed on 20 June 2018).
- Epocrates. Available online: http://www.epocrates.com/ (accessed on 20 June 2018).
- Medscape. Available online: www.medscape.com (accessed on 20 June 2018).
- Visual Dx. Available online: https://www.visualdx.com/ (accessed on 20 June 2018).
- UpToDate. Available online: https://www.uptodate.com/home (accessed on 20 June 2018).
- Colven, R.; Shim, M.H.M.; Brock, D.; Todd, G. dermatological diagnostic acumen improves with use of a simple telemedicine system for underserved areas of South Africa. Telemed. e-Health 2011, 17, 363–369. [Google Scholar] [CrossRef] [PubMed]
- Osei-tutu, A.; Shih, T.; Rosen, A.; Amanquah, N.; Chowdhury, M.; Nijhawan, R.I.; Siegel, D.; Kovarik, C. Mobile teledermatology in Ghana: Sending and answering consults via mobile platform. J. Am. Acad. Dermatol. 2013, 69, e90–e91. [Google Scholar] [CrossRef] [PubMed]
- Patro, B.; Tripathy, J.; Sinha, S.; Singh, A.; De, D.; Kanwar, A. Diagnostic agreement between a primary care physician and a teledermatologist for common dermatological conditions in North India. Indian Dermatol. Online J. 2015, 6, 21. [Google Scholar] [CrossRef] [PubMed]
- Tran, K.; Ayad, M.; Weinberg, J.; Cherng, A.; Chowdhury, M.; Monir, S.; El Hariri, M.; Kovarik, C. Mobile teledermatology in the developing world: Implications of a feasibility study on 30 Egyptian patients with common skin diseases. J. Am. Acad. Dermatol. 2011, 64, 302–309. [Google Scholar] [CrossRef] [PubMed]
- Azfar, R.S.; Weinberg, J.L.; Cavric, G.; Lee-Keltner, I.A.; Bilker, W.B.; Gelfand, J.M.; Kovarik, C.L. HIV-positive patients in Botswana state that mobile teledermatology is an acceptable method for receiving dermatology care. J. Telemed. Telecare 2011, 17, 338–340. [Google Scholar] [CrossRef] [PubMed]
- Azfar, R.S.; Lee, R.A.; Castelo-Soccio, L.; Greenberg, M.S.; Bilker, W.B.; Gelfand, J.M.; Kovarik, C.L. Reliability and validity of mobile teledermatology in human immunodeficiency virus–positive patients in Botswana: A pilot study. JAMA Dermatol. 2014, 150, 601. [Google Scholar] [CrossRef] [PubMed]
- Frühauf, J.; Hofman-Wellenhof, R.; Kovarik, C.; Mulyowa, G.; Alitwala, C.; Soyer, H.; Kaddu, S. Mobile teledermatology in sub-Saharan Africa: A useful tool in supporting health workers in low-resource centres. Acta Derm. Venereol. 2013, 93, 122–123. [Google Scholar] [CrossRef] [PubMed]
- Greisman, L.; Nguyen, T.M.; Mann, R.E.; Baganizi, M.; Jacobson, M.; Paccione, G.A.; Friedman, A.J.; Lipoff, J.B. Feasibility and cost of a medical student proxy-based mobile teledermatology consult service with Kisoro, Uganda, and Lake Atitlán, Guatemala. Int. J. Dermatol. 2015, 54, 685–692. [Google Scholar] [CrossRef] [PubMed]
- Littman-Quinn, R.; Mibenge, C.; Antwi, C.; Chandra, A.; Kovarik, C.L. Implementation of m-Health applications in Botswana: Telemedicine and education on mobile devices in a low resource setting. J. Telemed. Telecare 2013, 19, 120–125. [Google Scholar] [CrossRef] [PubMed]
- Mars, M.; Scott, R.E. Being spontaneous: The future of telehealth implementation? Telemed. e-Health 2017. [Google Scholar] [CrossRef] [PubMed]
- Sáenz, J.P.; Novoa, M.P.; Correal, D.; Eapen, B.R. On using a mobile application to support teledermatology: A case study in an underprivileged area in Colombia. Int. J. Telemed. Appl. 2018, 2018, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Chansky, P.B.; Simpson, C.L.; Lipoff, J.B. Implementation of a dermatology teletriage system to improve access in an underserved clinic: A retrospective study. J. Am. Acad. Dermatol. 2017, 77, 975–977. [Google Scholar] [CrossRef] [PubMed]
- Ferrándiz, L.; Moreno-Ramírez, D.; Ruiz-de-Casas, A.; Nieto-García, A.; Moreno-Alvarez, P.; Galdeano, R.; Camacho, F.M. An economic analysis of presurgical teledermatology in patients with nonmelanoma skin cancer. Actas Dermo-Sifiliogr. 2008, 99, 795–802. [Google Scholar] [CrossRef]
- Moreno-Ramirez, D.; Ferrandiz, L.; Ruiz-de-Casas, A.; Nieto-Garcia, A.; Moreno-Alvarez, P.; Galdeano, R.; Camacho, F.M. Economic evaluation of a store-and-forward teledermatology system for skin cancer patients. J. Telemed. Telecare 2009, 15, 40–45. [Google Scholar] [CrossRef] [PubMed]
| Platform Type | Advantages | Disadvantages | Examples |
|---|---|---|---|
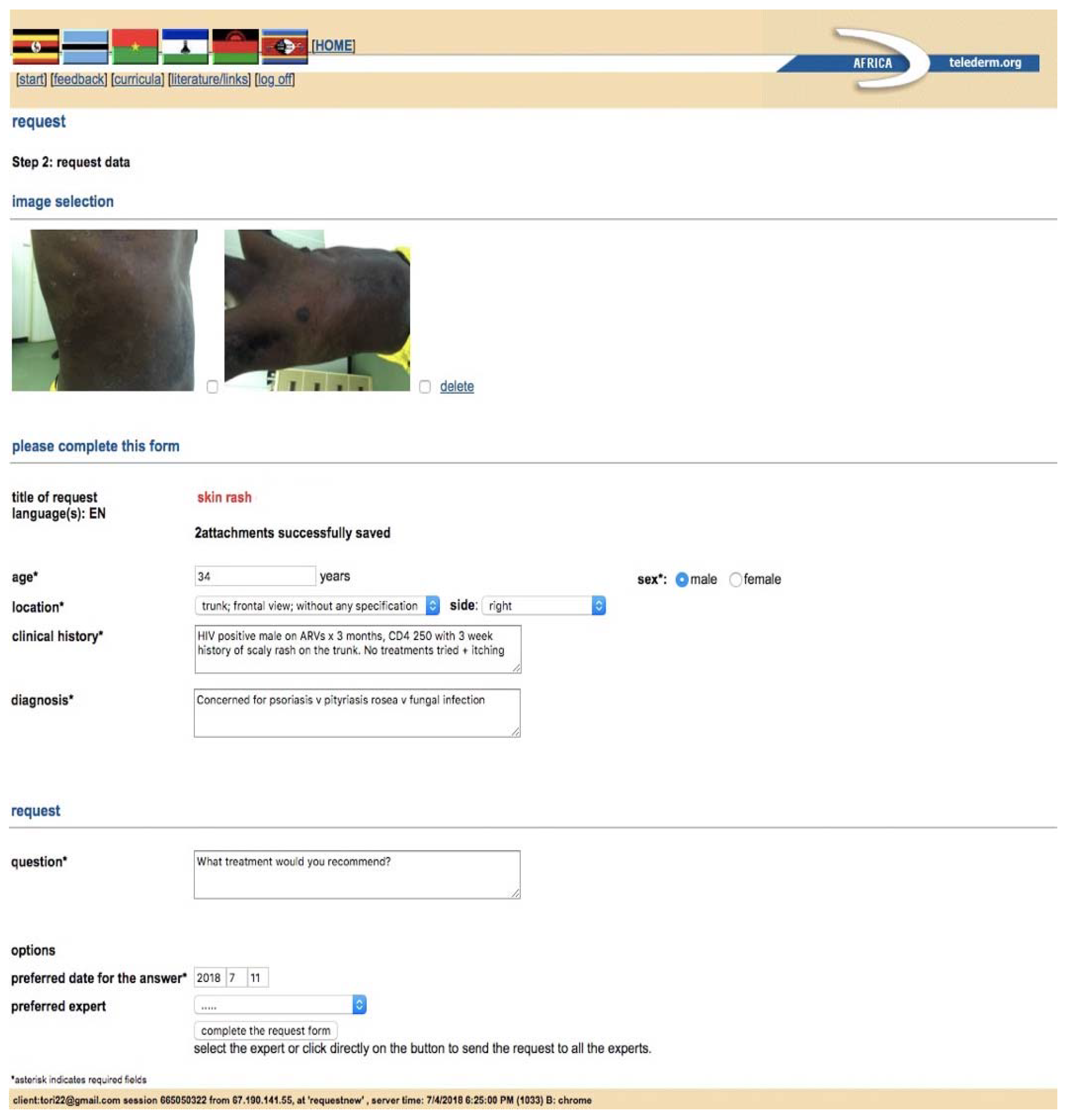
| Formal Teledermatology Platforms | |||
| Web and/or Mobile Teledermatology Applications | secure, guides referring providers through a dermatology consult, stores a record of all consults, most applications can be used on desktop or mobile device | must identify and register all users, must train all users, cost associated with creation of application or subscription to use, most time intensive for providers to utilize, difficult for providers to ask follow up questions, usually no mechanism for long term follow-up of cases, requires wifi or strong network signal | Africa Teledermatology Project [10], Swinfen Charitable Trust [11,12], MSF [13], ClickMedix [15], Azova [16] |
| Informal Teledermatology Platforms | |||
| Secure Email | can be used on desktop or mobile device, minimal training needed for users, minimally time intensive, fits into most providers daily routine, options for free access | security depends on email server, requires wifi or moderate network signal, no structure to guide consults, email accounts may have limited storage capacity, provider must identify and obtain emails of consultants to connect | free encrypted email services: Proton mail [17], Tutanota [18] |
| Secure Cloud Based File Sharing | can be used on desktop or mobile device, options for free access, provides a mechanism for organized storage of patient information, minimally time intensive | limited storage on free versions, requires some training for users, users must register, requires wifi or strong network signal, moderately secure, no structure to guide consults | Dropbox [19], Google Drive [20], OneDrive [21], Box [22] |
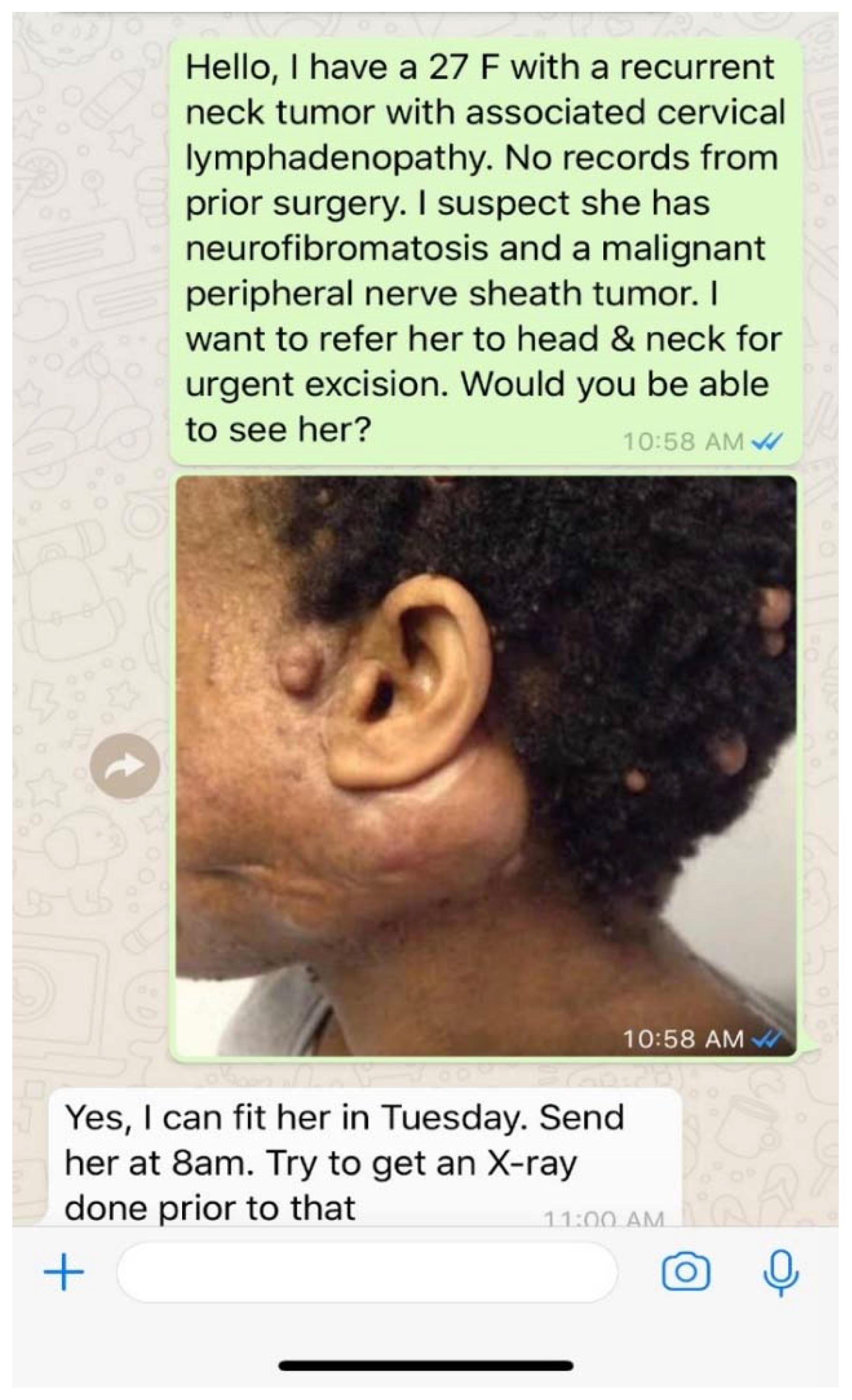
| Secure Direct Messaging Applications | fits into providers daily routine, least time intensive, minimal training needed, allows real time communication during patient visits, options for text/photos/videos/audio messaging, allows open communication for follow up questions and patient follow up, options for free access, secure end to end encryption, allows one-on-one or group chats, works well with low signal or wifi | provider must identify a consultant and obtain a phone number to connect, no structure to guide consults, no organized record of consults or communications | Free: WhatsApp [23,24], MedTunnel [25],Bloomtext [26] Paid: Imprivata [27], TigerConnect [28], Voalte [29], QliqSoft [30], Spok Mobile [31] |
| Social Networking Sites | free, low time commitment, minimal training needed, allows connection to a single provider or a global network, any provider can register and connect, works well with low signal or wifi | cannot guarantee security, difficult to guarantee credentials and expertise of consultants providing advice, no structure to guide consults, no organized record of consults or communications | Telederm.org [32], Sermo [33], Facebook [34] |
| Telepathology Platforms | |||
| Virtual Slide Microscopy (VSM) | secure, highest quality images, can view any part of the slide at any magnification, creates an organized library of cases for teaching or research, least time intensive for reviewer when slides are pre-scanned | high cost to purchase, ongoing costs to maintain equipment and software, requires significant training, needs high storage capacity for images, needs consistent and high bandwidth to function, slide scanning can be time intensive for sender | Olympus VS 120 [35], Zeiss Axio Scan.Z1 [36], Leica Aperio AT2 [37] |
| Dynamic Slide Microscopy (DSM) | secure, can view any part of the slide at any magnification, potentially lower cost to implement compared to VSM | highest bandwidth requirements which may limit image quality, requires strict program compatibility for viewing, requires significant training, ongoing costs to maintain equipment and software, most time intensive to use for sender and reviewer | Leica Aperio LV1 [38], 3dHistech Panoramic DESK II DW [39] |
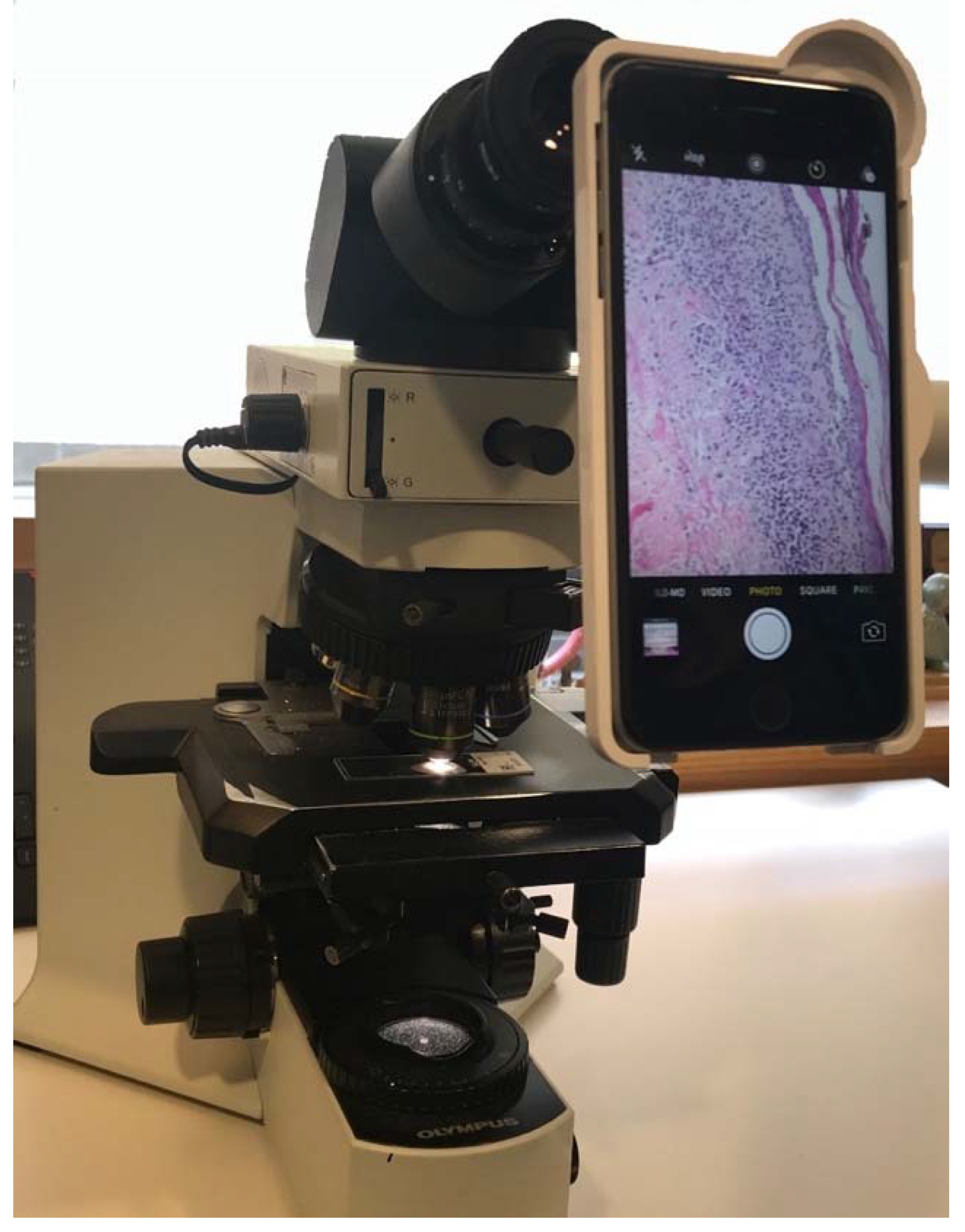
| Static Imaging | lowest cost, works with any microscope, no software requirements, does not require consistent wifi | risk of sampling error, quality of images varies based on skills of photographer, can only view areas of tissue and magnification chosen by photographer, time intensive for sender and reviewer | smartphone to eyepiece attachments: LabCam [40], Magnifi [41], Snapzoom [42]; any smartphone camera through eyepiece; any digital microscope camera |
| Applications of Teledermatology | Benefits | Recommended Platforms for Remote Providers |
|---|---|---|
| Tele-Triage | appropriate and timely scheduling of patients into dermatology clinic, timely referral of dermatology patients to other specialists | secure direct messaging |
| Primary Care to Dermatology Consultation | diagnostic and management support, building dermatology skills over time | secure direct messaging |
| Specialist to Dermatology Consultation | diagnostic and management support, care coordination, building dermatology skills over time | secure direct messaging |
| Dermatologist to Dermatologist Consultation | second opinion, subspecialty dermatologist consultation, super specialist consultation for rare diseases, decreases isolation and burnout | formal teledermatology application, secure email, secure direct messaging, cloud based file sharing |
| Telepathology | expert analysis of skin biopsy specimens, improved diagnostic accuracy of skin disease, training of local pathologists | static images via smartphone or digital microscope camera |
| Long Term Management | allows for provider to dermatologist follow up, allows patient to dermatologist follow up, improves patient compliance and patient outcomes | secure direct messaging, secure email, cloud based file sharing |
| Care Coordination | allows for group chats between various providers to save time and resources | secure direct messaging, secure email, cloud based file sharing |
| Dermatology Education | remote access to dermatology education in any setting, builds local capacity | web based learning modules, video lectures, virtual patient encounters, email or web based access to lectures/handouts/guidelines, clinical decision support tools |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Williams, V.; Kovarik, C. Long-Range Diagnosis of and Support for Skin Conditions in Field Settings. Trop. Med. Infect. Dis. 2018, 3, 84. https://doi.org/10.3390/tropicalmed3030084
Williams V, Kovarik C. Long-Range Diagnosis of and Support for Skin Conditions in Field Settings. Tropical Medicine and Infectious Disease. 2018; 3(3):84. https://doi.org/10.3390/tropicalmed3030084
Chicago/Turabian StyleWilliams, Victoria, and Carrie Kovarik. 2018. "Long-Range Diagnosis of and Support for Skin Conditions in Field Settings" Tropical Medicine and Infectious Disease 3, no. 3: 84. https://doi.org/10.3390/tropicalmed3030084
APA StyleWilliams, V., & Kovarik, C. (2018). Long-Range Diagnosis of and Support for Skin Conditions in Field Settings. Tropical Medicine and Infectious Disease, 3(3), 84. https://doi.org/10.3390/tropicalmed3030084




