4.3. Discussion
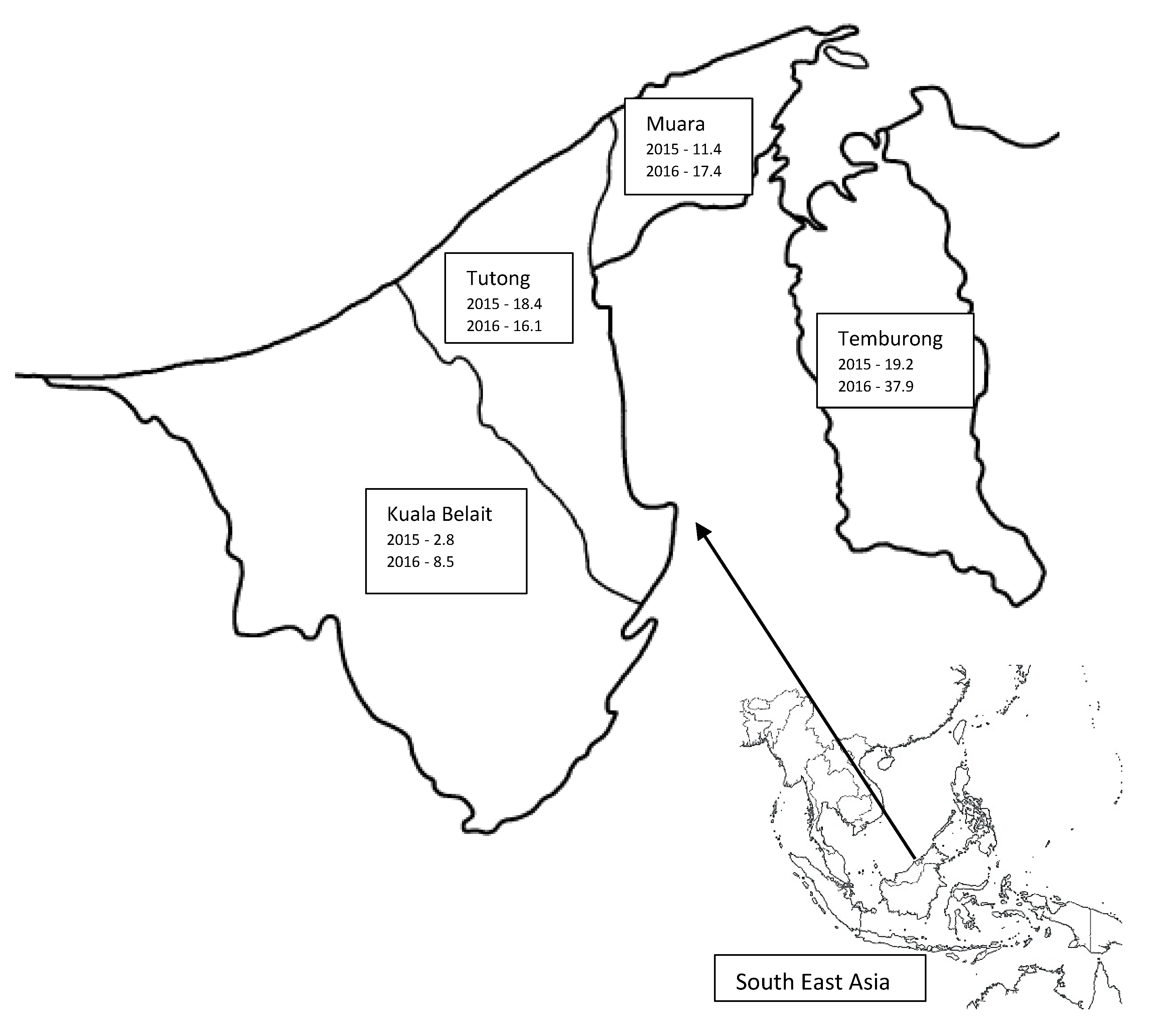
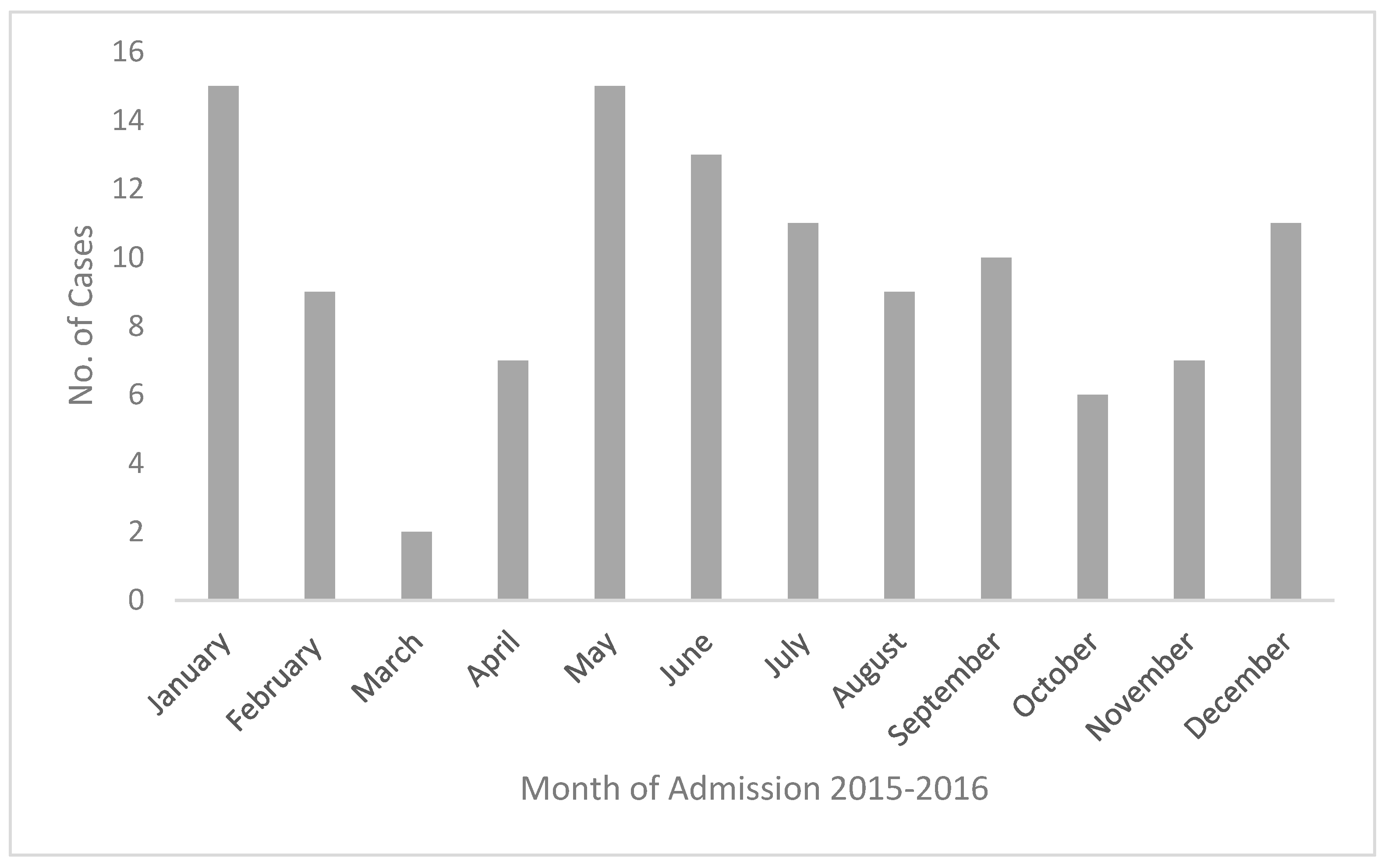
This is the first detailed epidemiological study of melioidosis from Brunei Darussalam. The data have revealed a slight increase in incidence from 11 to 16 per 100,000 population between 2015 and 2016. It also showed a high number of expatriate workers being affected. Diabetes mellitus and chronic renal disease were the most common risk factors, whilst pneumonia and soft tissue abscess were the most common clinical presentations. The data suggested a possible link with seasonal variation in rainfall with more cases diagnosed in the wet months. Interestingly the highest incidence rate was from the Temburong district, which has the highest annual rainfall. The mortality was 27%, being higher in women and patients presenting with septic shock.
For the purpose of discussion, we have compared our results with other large epidemiological studies from Asia-Pacific published after 2010 [
18,
19,
20,
21,
22,
23,
24,
25]. Our findings of male preponderance, the median age of patients, diabetes mellitus and chronic renal disease as the most common risk factors, and pneumonia and soft tissue abscesses as the most common presentations, are similar to the studies reviewed.
Though occupational history was not consistently recorded in the hospital notes, similar to a previous study [
8], 25 expatriate patients with varied nationalities (median age 41.5 years) were noted. Generally the majority of these were labourers working in the agriculture or construction industries, with a high chance of exposure to contaminated soil and water.
The overall incidences of 11 and 16.3 per 100,000 population in 2015 and 2016, respectively, are considerably higher than those reported from Thailand and Singapore [
22,
25]. It is important to note that, in Singapore, a recent decrease in incidence was reported [
25], while the incidence has remained constant or increased in Australia and Thailand [
18,
22]. Our rates are comparable to the rate of 16.45/100,000 reported from the state of Kedah, Malaysia by Hassan et al. [
21]. In contrast, another study based on the melioidosis registry from the Pahang state of Malaysia reported a much lower rate of 4.3/100,000 (adult 6.0/100,000 and paediatric 1.6/100,000) [
26]. This reflects geographical differences, as seen in our study, with different rates between districts, even for a small country.
The current rates reported showed marked increase compared to the incidence rates (2.9 to 5.6/100,000 for 1993 and 1994, respectively) reported by Luqman et al. [
5]. The upsurge may well be contributed to by better awareness and improvement in diagnostic facilities. Melioidosis was possibly under-diagnosed and under-reported in the past [
27]. Another plausible reason for the upward trend is the rise in the overall population along with an increase in the number of people with risk factors, such as diabetes and chronic kidney disease.
There were four patients (3.5%) under the age of 15 years, comparable to the rate reported by Hassan et al., (5.5%), and higher than the rate reported by How et al., (1.6/100,000) [
21,
26]. Consistent with reports in the literature, our paediatric patients had no risk factors, presented with soft tissue abscesses, two of them during the wet months of December and January, and recovered completely with treatment [
28]. Unlike Kingsley et al., we did not observe any cases of neonatal melioidosis [
29].
In the present study, a higher number of cases was observed in the wet months of May to July and December to February, with 64.3% being admitted during these months. The incidence was also higher in the Temburong district, which records the highest rainfall amongst the four districts. A high level of moisture in the soil during months of high rainfall has been reported to correlate with an increased incidence of melioidosis [
30,
31]. This association has been reported from Australia [
18,
20], Singapore [
25], Malaysia [
21], and India [
23]. In contrast, Limmathurotsakul et al. reported a negative association between the total annual rainfall and the number of cases in each year of their study from Thailand [
22]. However, in this study monthly rainfall data and the number of cases per month were not available. Consistent with an incubation period of a few weeks, the incidence may also be higher in the corresponding period after high rainfall [
32].
Diabetes mellitus was recorded as a risk factor in 74.8% of cases, similar to the proportion in India [
23] and Malaysia [
24]. Other studies have reported it in 39–57% of their cases [
18,
20,
21,
22,
25]. In two studies from Australia [
18,
20], excessive alcohol use was the second most common risk factor. In the present study it was noted in 5.2% of cases but could be underreported due to a reluctance to volunteer such a history. However, the sale of alcohol is banned in Brunei Darussalam and, therefore, our finding is likely to be a true reflection of the real situation.
The number of patients with melioidosis without any risk factors was lower (7.8%,
n = 9) in the present study compared to other studies (13–22%) [
18,
20,
23,
24] but similar to that reported by Kingsley et al. [
29]. It has been suggested that individuals with no risk factors have less severe symptoms and mortality is rare [
29]. However, in the present study 5/9 patients succumbed to the disease, three of whom presented with septic shock, and two with large soft tissue abscesses suggesting fulminant infection.
Consistent with the studies reviewed, pneumonia was the most common clinical presentation followed by soft tissue abscesses [
18,
20,
21,
22,
23,
24,
25]. Septic shock was the mode of presentation in 21.7% (
n = 25) cases. In a review of case reports published from Malaysia, a high frequency of primary neurological presentation was noted (7.5%) [
29]. The rates reported by other authors [
18,
21,
23,
24] and one case in the present study is much lower. This may be due to selection bias in the case reports reviewed.
Internal organ abscesses were most common in the spleen and liver, as noted in the literature [
18,
21,
23,
24]; however, the proportion was much higher in the present study. We had only one case of subdural empyema and no cases with mycotic aneurysms or pericardial involvement. The proportion of prostatic abscesses in the present study was 4.3%; there is a wide variation reported in the literature, from 0.3% in Thailand [
33], to a high of 20% in Australia [
18]. Our finding of the frequency of parotid involvement (
n = 1, 0.9%) is comparable to other studies [
23,
24,
29], but much lower than that reported in Thai children (20–30%) [
34]. We did not find any case with pancreatic involvement in the present study. The four cases previously reported were seen over a period of six years, compared to two years of the present study [
7]. Moreover, only about 50% of patients in the present study underwent CT-TAP for various reasons, which could have resulted in under-reporting of internal organ abscesses.
The overall mortality in the present study was 27%, with a higher mortality in women (41.9%) compared to men (21.4%;
p < 0.05). This association has also been reported by Kingsley et al. [
29]. Mortality was also significantly higher in patients who presented with septic shock.
There is a wide variation in the reported mortality in the literature, from 9.5% in India [
23], 42.6% in Thailand [
22], and between 32–63% in Malaysia [
19,
21,
24]. Decreasing mortality rates have been reported from Australia [
18] and Singapore [
25]. The reasons put forward for this are access to standardized health care and the institution of prompt treatment according to recommendations [
35]. In Singapore, in particular, it is thought to be due to efforts to optimise diabetes care and enhanced environmental and water management [
25]. Our current rate is slightly higher than that reported in the earlier study by Luqman et al., (20.3%) [
5], possibly due to late presentations and multiple comorbidities.
Five cases (4.3%) had recurrence of the disease, which is a similar rate to that reported by Currie et al. [
18]. One of the 31 cases that did not survive also presented with a recurrence. They had underlying risk factors of diabetes mellitus (4/6), malignancy (2/6), and chronic renal disease (1/6). Non-compliance with previous treatment was recorded in two cases. The institution of prompt treatment along international guidelines explains the lower current rate compared to relapses seen in 60% of cases in the past [
5].
The strength of the present study is that, owing to the method of data collection, it can be taken as a true reflection of the disease state in the country. A limitation of the study was its retrospective nature. Data, particularly on occupation and alcohol abuse as risk factors, were not adequately recorded.