Incidence and Spatial Mapping of Tuberculosis and Multidrug-Resistant Tuberculosis in Libreville, Republic of Gabon, in 2022
Abstract
1. Introduction
2. Methods
2.1. Design and Settings
2.2. Data Sampling
2.3. Data Collection
2.4. Data Analysis
2.5. Ethical Considerations
3. Results
3.1. Study Population
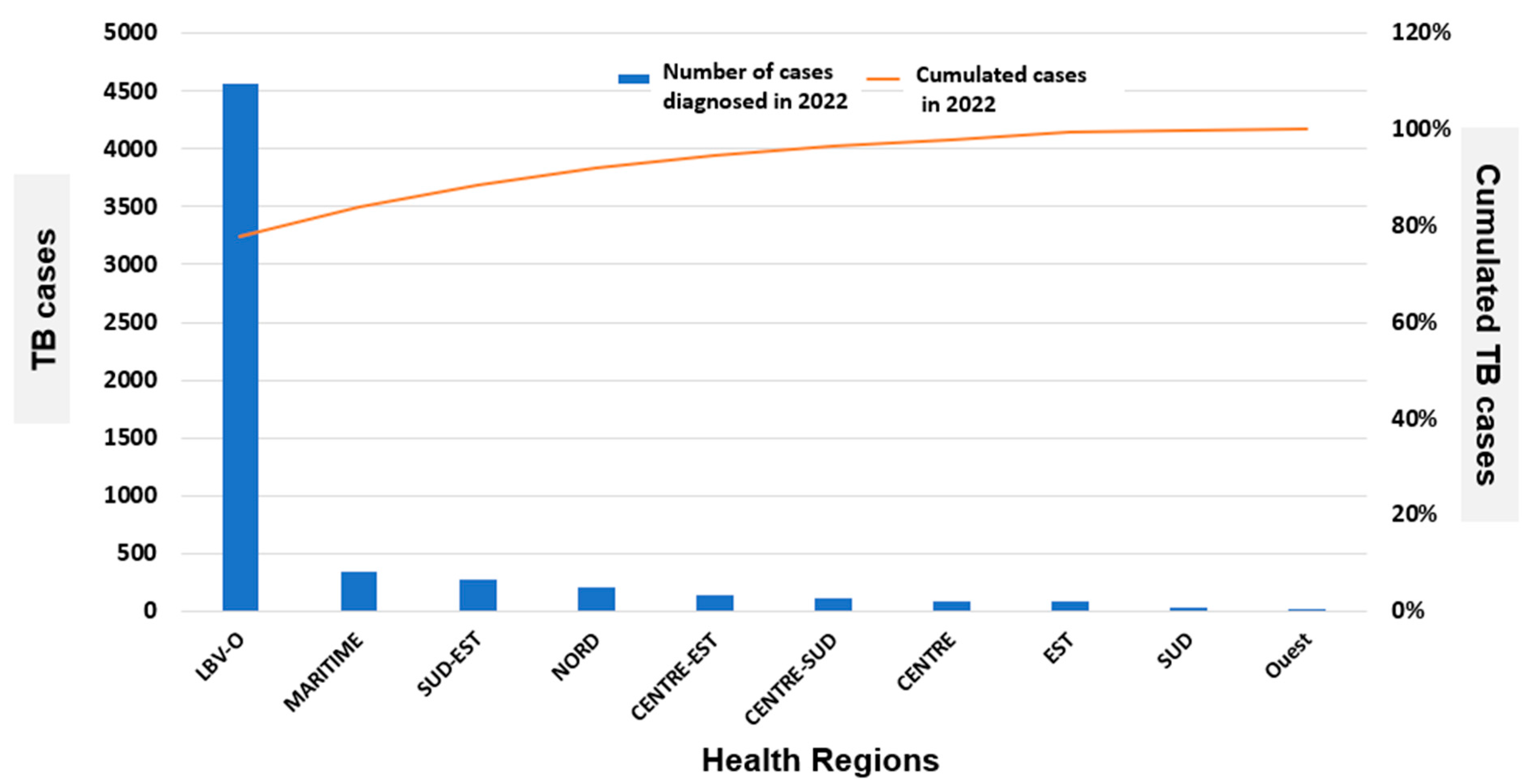
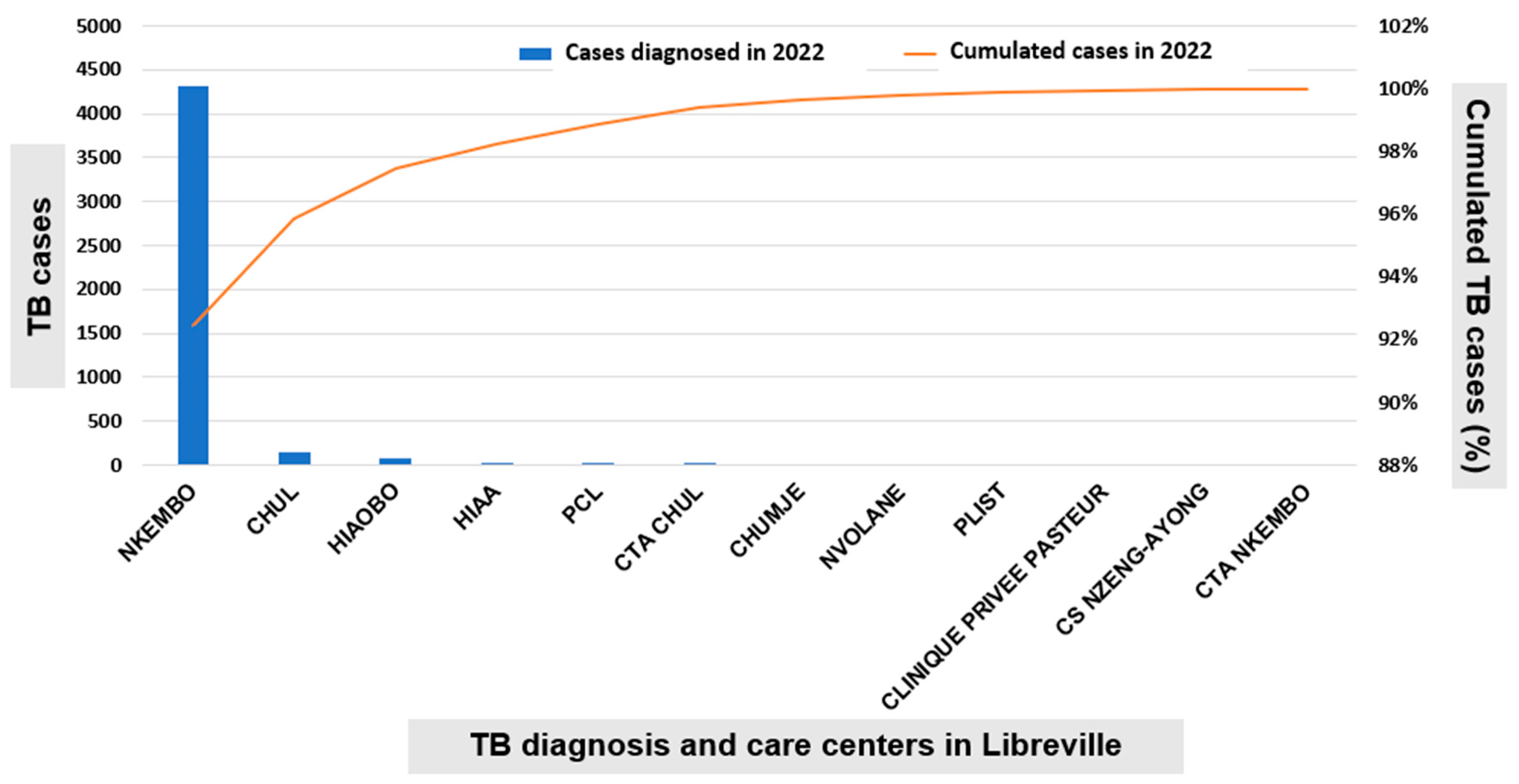
3.2. Incidence of Tuberculosis in the Republic of Gabon and Libreville in the Year 2022
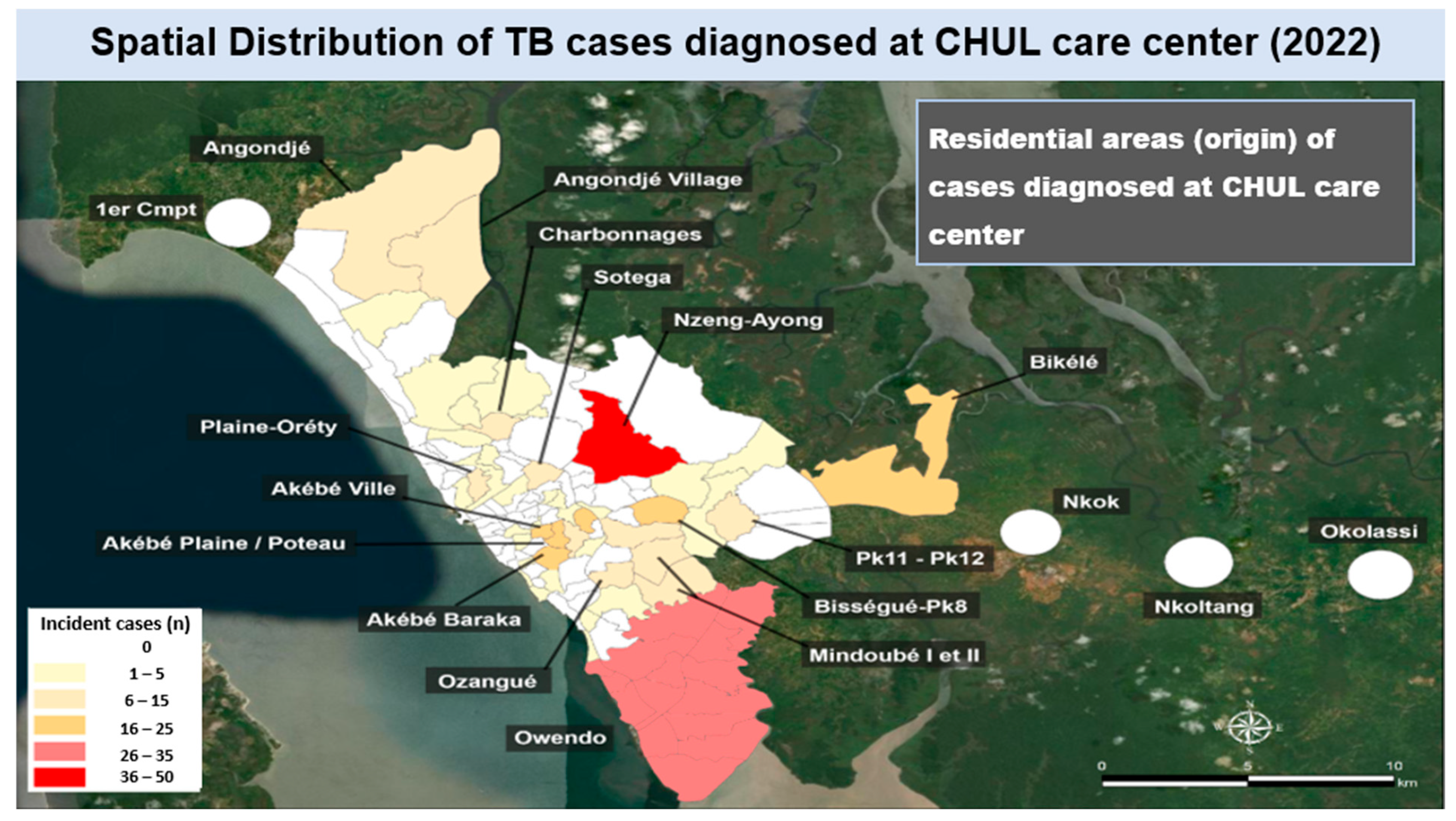
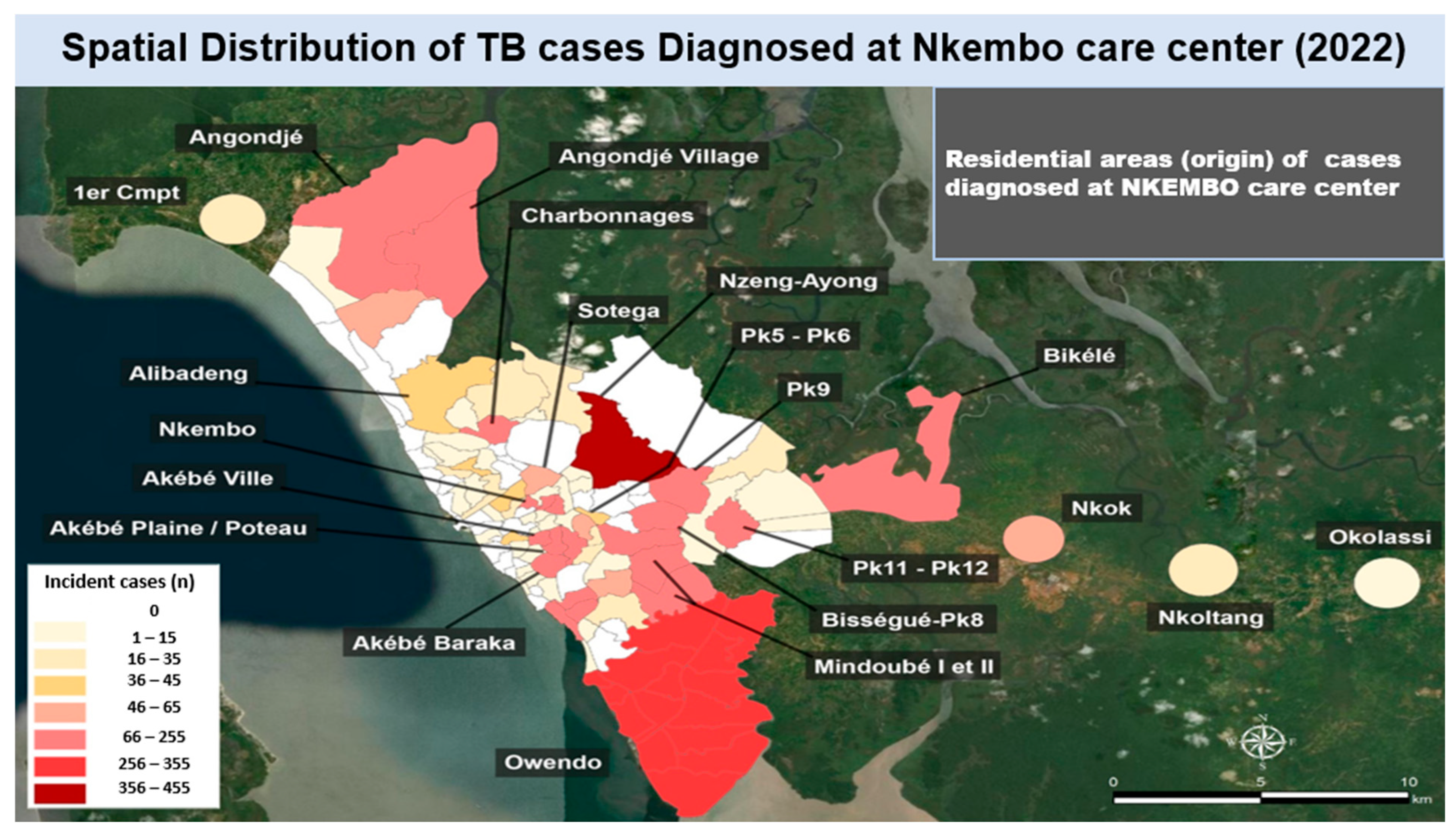
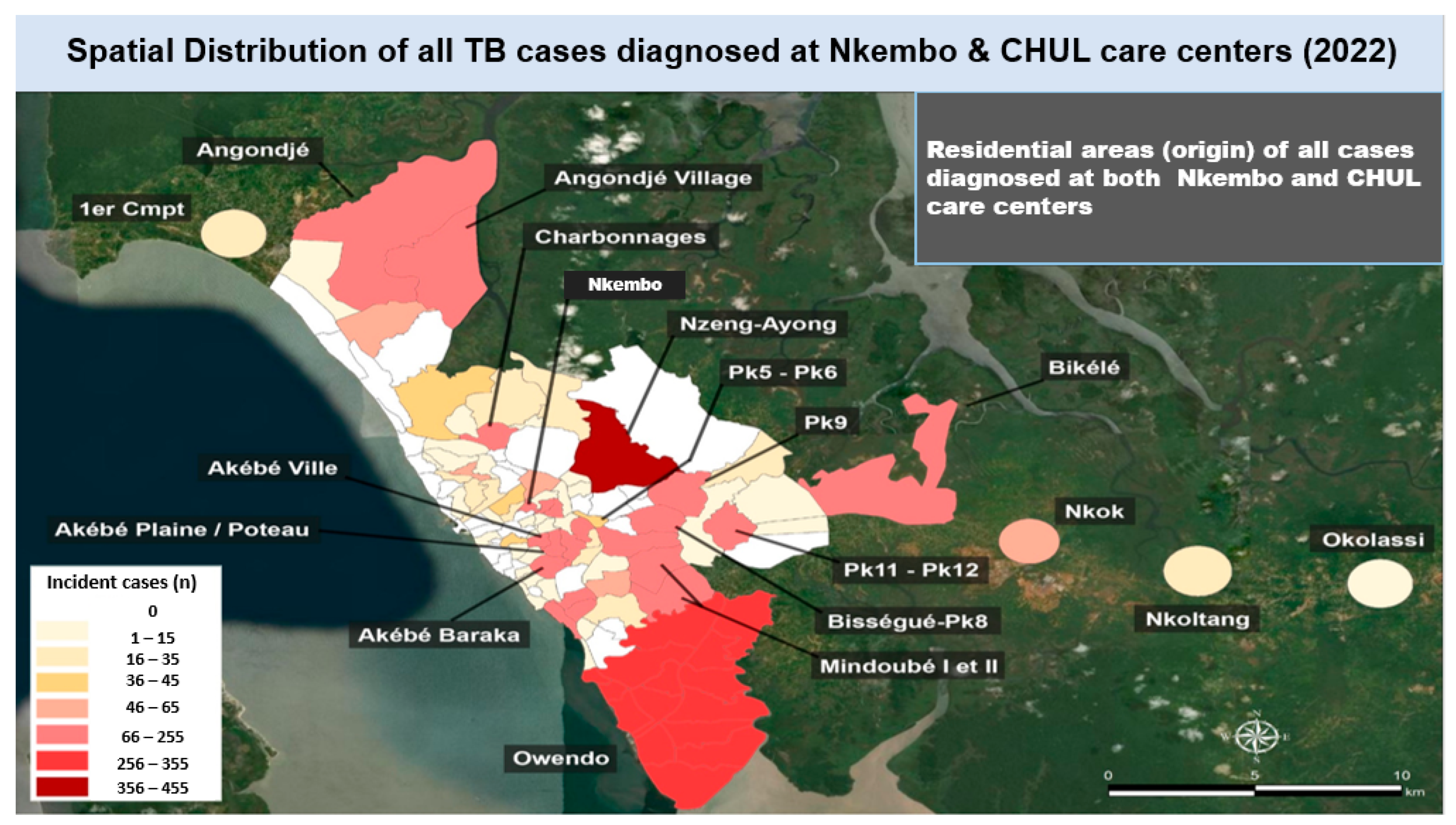
3.3. Spatial Distribution of TB Cases Diagnosed in 2022 in Libreville
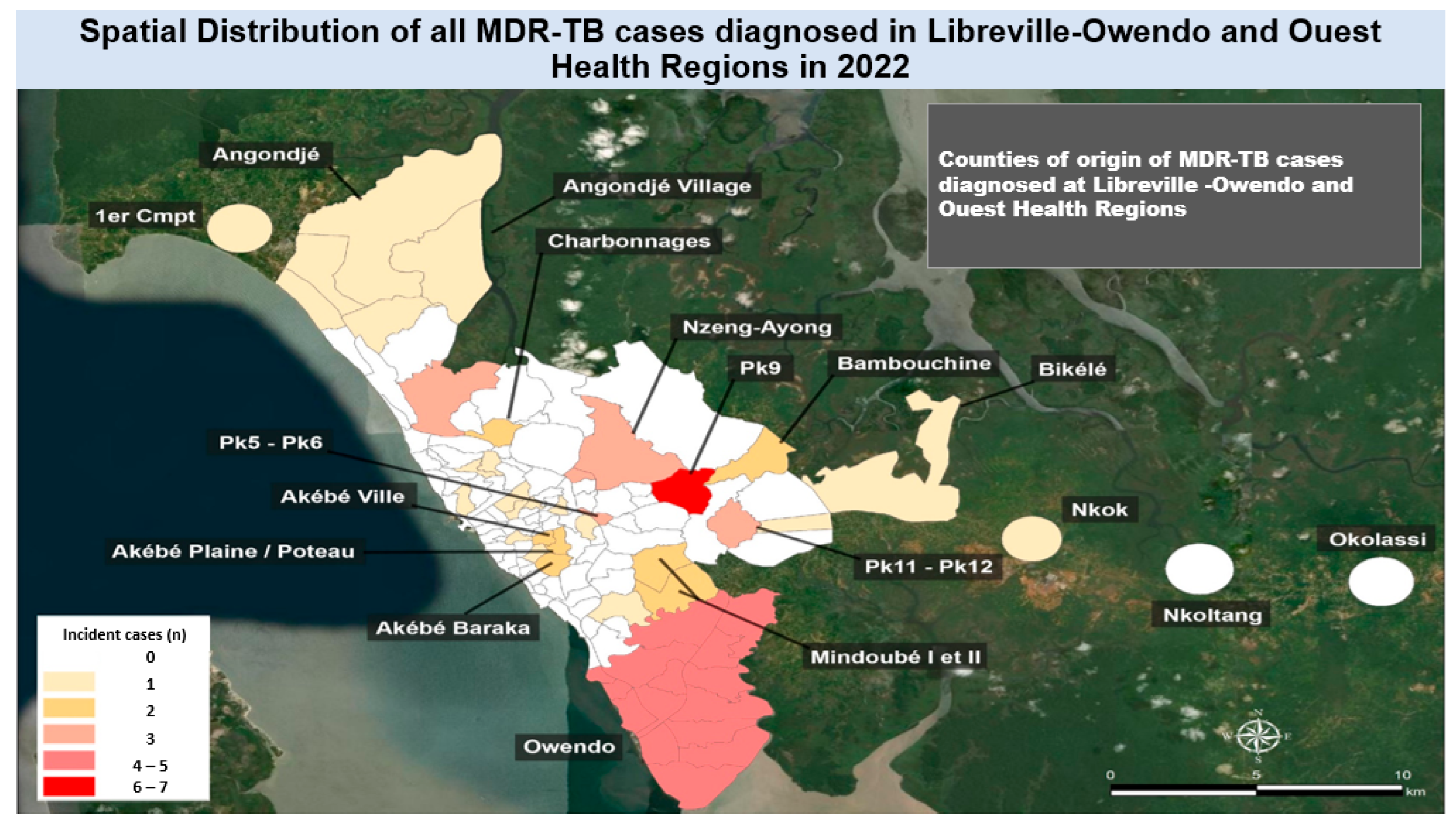
3.4. Distribution of Multi-Drug-Resistant Tuberculosis Cases in Libreville in 2022
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lange, C.; Dheda, K.; Chesov, D.; Mandalakas, A.M.; Udwadia, Z.; Horsburgh, C.R., Jr. Management of drug-resistant tuberculosis. Lancet 2019, 394, 953–966. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Tuberculosis Report 2023. Available online: https://www.who.int/teams/global-tuberculosis-programme/tb-reports/global-tuberculosis-report-2023 (accessed on 11 November 2025).
- Park, P.G.; Fatima, M.; An, T.; Moon, Y.E.; Woo, S.K.; Youn, H.; Hong, K.J. Current development of therapeutic vaccines for the treatment of chronic infectious diseases. Clin. Exp. Vaccine Res. 2024, 13, 21–27. [Google Scholar] [CrossRef] [PubMed]
- National Tuberculosis Program (PNLT). Rapport Annuel 2022. Available online: https://www.sante.gouv.gabon (accessed on 11 November 2025). (In French)
- Nasiri, M.J.; Lutfy, K.; Venketaraman, V. Challenges of multidrug-resistant tuberculosis meningitis: Current treatments and the role of glutathione as an adjunct therapy. Vaccines 2024, 12, 1397. [Google Scholar] [CrossRef] [PubMed]
- National Tuberculosis Program (PNLT) Report. Review of the National Tuberculosis Program (PNLT). 2022. Available online: https://www.sante.gouv.gabon (accessed on 11 November 2025). (In French).
- Mesquita, C.R.; Enk, M.J.; Guimarães, R.J.D.P.S. Spatial analysis studies of endemic diseases for health surveillance: Application of scan statistics for surveillance of tuberculosis among residents of a metropolitan municipality aged 60 years and above. Ciência Saúde Coletiva 2021, 26, 5149–5156. [Google Scholar] [CrossRef] [PubMed]
- Graser, A.; Sutton, T.; Bernasocchi, M. The QGIS project: Spatial without compromise. Patterns 2025, 6, 101265. [Google Scholar] [CrossRef] [PubMed]
- Longley, P.A.; Goodchild, M.F.; Maguire, D.J.; Rhind, D.W. Geographic Information Science and Systems; John Wiley & Sons: Hoboken, NJ, USA, 2015. [Google Scholar]
- Zhong, Y.; Xie, H.; Cai, F.; Liu, M.; Gan, H.; Tang, Z.; Bai, Y. Global burden of multidrug-resistant tuberculosis in children and adolescents. Pediatr Res. 2025, in press. [Google Scholar] [CrossRef] [PubMed]
- Bélard, S.; Remppis, J.; Bootsma, S.; Janssen, S.; Kombila, D.U.; Beyeme, J.O.; Rossatanga, E.G.; Kokou, C.; Osbak, K.K.; Mba, R.M.O.; et al. Tuberculosis treatment outcome and drug resistance in Lambaréné, Gabon: A prospective cohort study. Am. J. Trop. Med. Hyg. 2016, 95, 472–480. [Google Scholar] [CrossRef] [PubMed]
- Kombila, U.D.; Boulingui, C.M.; N’gomanda, F.; Mavoungou, J.V.M.; Ngea Epossi, C.B.H.; Bivigou, N.; Bivigou, N.; Tsioukaka, S.; Tshisekedi, J.D.D.; Mahoumbou, J.; et al. Pre-extensively and extensively drug-resistant tuberculosis in Libreville, Gabon. Rev. Des. Mal. Respir. 2024, 41, 542–548. (In French) [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Tuberculosis Report 2021; World Health Organization: Geneva, Switzerland, 2021; Available online: https://www.who.int/publications/i/item/9789240037021 (accessed on 30 June 2025).
- Kabir, S.; Tahir, Z.; Mukhtar, N.; Sohail, M.; Saqalein, M.; Rehman, A. Fluoroquinolone resistance and mutational profile of gyrA in pulmonary MDR tuberculosis patients. BMC Pulm. Med. 2020, 20, 138. [Google Scholar] [CrossRef] [PubMed]
- Abdul, A.J.B.P.A.; Adegbite, B.R.; Ndanga, M.E.D.; Edoa, J.R.; Mevyann, R.C.; Mfoumbi, G.R.A.I.; de Dieu, T.J.; Mahoumbou, J.; Biyogho, C.M.; Jeyaraj, S.; et al. Resistance patterns among drug-resistant tuberculosis patients and trends-over-time analysis of national surveillance data in Gabon, Central Africa. Infection 2023, 51, 697–704. [Google Scholar] [CrossRef] [PubMed]
- Assiana, D.O.E.; Abdul, J.B.P.A.; Linguissi, L.S.G.; Epola, M.; Vouvoungui, J.C.; Mabiala, A.; Biyogho, C.M.; Edoa, J.R.; Adegbite, B.R.; Adegnika, A.A.; et al. Epidemiological profile of multi-drug resistant and extensively drug-resistant Mycobacteriun tuberculosis among Congolese patients. Ann. Clin. Microbiol. Antimicrob. 2021, 20, 84. [Google Scholar] [CrossRef] [PubMed]
| Male | Female | Total | |
|---|---|---|---|
| CDT Nkembo | 3232 | 1077 | 4309 |
| CDT CHUL | 132 | 25 | 157 |
| SUM | 3364 | 1102 | 4466 |
| <15 Year | 15–49 Years | 50+ Years | |
|---|---|---|---|
| Age group | 253 | 3537 | 676 |
| % | 6% | 79% | 15% |
| Bacteriologically Confirmed | Clinically Confirmed | Extrapulmonary TB | |
|---|---|---|---|
| Number | 3266 | 764 | 436 |
| % | 73% | 17% | 10% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Manzengo, C.; Ngatu, N.R.; Manguinga-Guitouka, S.; Lignenguet, F.; Nkone-Asseko, G.; Nsimba-Miezi, M.; Miyatake, N.; Lami-Nzunzu, J.; Hirao, T. Incidence and Spatial Mapping of Tuberculosis and Multidrug-Resistant Tuberculosis in Libreville, Republic of Gabon, in 2022. Trop. Med. Infect. Dis. 2026, 11, 8. https://doi.org/10.3390/tropicalmed11010008
Manzengo C, Ngatu NR, Manguinga-Guitouka S, Lignenguet F, Nkone-Asseko G, Nsimba-Miezi M, Miyatake N, Lami-Nzunzu J, Hirao T. Incidence and Spatial Mapping of Tuberculosis and Multidrug-Resistant Tuberculosis in Libreville, Republic of Gabon, in 2022. Tropical Medicine and Infectious Disease. 2026; 11(1):8. https://doi.org/10.3390/tropicalmed11010008
Chicago/Turabian StyleManzengo, Casimir, Nlandu Roger Ngatu, Stredice Manguinga-Guitouka, Fleur Lignenguet, Ghislaine Nkone-Asseko, Marie Nsimba-Miezi, Nobuyuki Miyatake, Jose Lami-Nzunzu, and Tomohiro Hirao. 2026. "Incidence and Spatial Mapping of Tuberculosis and Multidrug-Resistant Tuberculosis in Libreville, Republic of Gabon, in 2022" Tropical Medicine and Infectious Disease 11, no. 1: 8. https://doi.org/10.3390/tropicalmed11010008
APA StyleManzengo, C., Ngatu, N. R., Manguinga-Guitouka, S., Lignenguet, F., Nkone-Asseko, G., Nsimba-Miezi, M., Miyatake, N., Lami-Nzunzu, J., & Hirao, T. (2026). Incidence and Spatial Mapping of Tuberculosis and Multidrug-Resistant Tuberculosis in Libreville, Republic of Gabon, in 2022. Tropical Medicine and Infectious Disease, 11(1), 8. https://doi.org/10.3390/tropicalmed11010008






