High Rate of Human T-Cell Lymphotropic Virus-2 in Patients with HIV in the Peruvian Amazon
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Study Population and Enrollment Criteria
2.3. Statistical Data Analysis
2.4. Ethical Considerations
3. Results
3.1. Overview of the Study Population
3.2. HTLV Subtypes
3.3. Description of HTLV-HIV Co-Existence
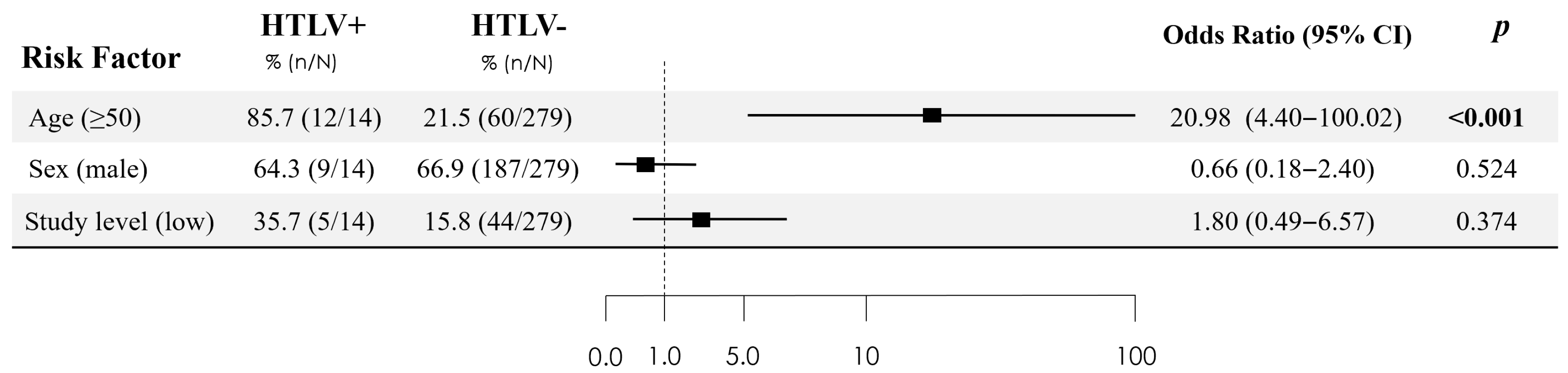
3.4. HTLV-Positive vs. HTLV-Negative Patients
| N | Type of HTLV | Age | Sex | Ethnicity | Origin of Parents | Breast-Feeding | Sexual Behavior/ Number of Sexual Partners | Non-Sterilized Procedures a | Transfusion | Living in Rural Area b | Chronic Hepatitis | STI c | CD4 Count Nadir/Last | HIV Viral Load |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | HTLV-1 | 62 | M | Mestizo | Tarapoto | Yes | Transgender/<5 | No | Yes | No | No | No | 479/677 | <20 |
| 2 | HTLV-2 | 52 | M | Mestizo | Iquitos | Yes | Homosexual/<5 | No | No | No | No | No | 218/674 | <20 |
| 3 | HTLV-2 | 56 | M | Kukuma | Marañón River | Yes | Homosexual/<5 | No | No | No | No | No | 287/684 | <20 |
| 4 | HTLV-2 | 60 | F | Mestizo | Nauta | Yes | Heterosexual/≥5 | No | No | No | No | No | 113/113 | <20 |
| 5 | HTLV-2 | 61 | M | Mestizo | Requena | Yes | Heterosexual/≥5 | No | Yes | No | No | No | 134/322 | <20 |
| 6 | HTLV-2 | 53 | M | Mestizo | Cuzco | Yes | Bisexual/≥5 | No | Yes | No | Yes | Gonorrhea Syphilis | 52/371 | <20 |
| 7 | HTLV-2 | 60 | M | Mestizo | LOF | Yes | Heterosexual/LOF | LOF | No | No | Yes | No | NA | <20 |
| 8 | Non-typable HTLV | 43 | F | Mestizo | Pebas | Yes | Heterosexual/<5 | No | No | No | No | No | 261/261 | <20 |
| 9 | Non-typable HTLV | 55 | M | Mestizo | Iquitos | Yes | Heterosexual/<5 | No | No | No | No | Gonorrhea Syphilis | 455/455 | <20 |
| 10 | HTLV-2 | 54 | F | Mestizo | Marañón River | Yes | Heterosexual/≥5 | Scarification | No | No | No | Syphilis | 76/525 | <20 |
| 11 | HTLV-2 | 64 | M | Mestizo | LOF | Yes | Heterosexual/LOF | LOF | No | No | No | No | 171/399 | <20 |
| 12 | HTLV-2 | 66 | F | Mestizo | Ucayali River | Yes | Heterosexual/<5 | No | No | No | No | No | 519/519 | <20 |
| 13 | HTLV-2 | 45 | M | Mestizo | Iquitos | Yes | Heterosexual/<5 | No | No | No | No | No | 434/434 | <20 |
| 14 | HTLV-2 | 50 | M | Mestizo | Iquitos | No | Heterosexual/<5 | No | No | No | No | Gonorrhea | 344/344 | <20 |
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| HTLV | Human T-cell lymphotropic virus |
| HIV | Human immunodeficiency virus |
| PWH | People with HIV |
| ELISA | Enzyme-linked immunosorbent assay |
| IQRs | Interquartile ranges |
| CIs | Confidence intervals |
| ART | Anti-retroviral therapy |
References
- Rockwood, N.; Cook, L.; Kagdi, H.; Basnayake, S.; Bangham, C.R.M.; Pozniak, A.L.; Taylor, G.P. Immune Compromise in HIV-1/HTLV-1 Coinfection With Paradoxical Resolution of CD4 Lymphocytosis During Antiretroviral Therapy: A Case Report. Medicine 2015, 94, e2275. [Google Scholar] [CrossRef]
- Branda, F.; Romano, C.; Pavia, G.; Bilotta, V.; Locci, C.; Azzena, I.; Deplano, I.; Pascale, N.; Perra, M.; Giovanetti, M.; et al. Human T-Lymphotropic Virus (HTLV): Epidemiology, Genetic, Pathogenesis, and Future Challenges. Viruses 2025, 17, 664. [Google Scholar] [CrossRef]
- Legrand, N.; McGregor, S.; Bull, R.; Bajis, S.; Valencia, B.M.; Ronnachit, A.; Einsiedel, L.; Gessain, A.; Kaldor, J.; Martinello, M. Clinical and Public Health Implications of Human T-Lymphotropic Virus Type 1 Infection. Clin. Microbiol. Rev. 2022, 35, e00078-21. [Google Scholar] [CrossRef] [PubMed]
- Solorzano-Salazar, D.M.; Hernández-Vásquez, A.; Visconti-Lopez, F.J.; Azañedo, D. Research on HTLV-1 and HTLV-2 in Latin America and the Caribbean over the Last Ten Years. Heliyon 2023, 9, e13800. [Google Scholar] [CrossRef]
- Carneiro-Proietti, A.B.F.; Catalan-Soares, B.; Proietti, F.A.; GIPH (Interdisciplinary HTLV-1/II Research Group). Human T Cell Lymphotropic Viruses (HTLV-I/II) in South America: Should It Be a Public Health Concern? J. Biomed. Sci. 2002, 9, 587–595. [Google Scholar] [CrossRef]
- Abreu, I.N.; Lima, C.N.C.; Sacuena, E.R.P.; Lopes, F.T.; Da Silva Torres, M.K.; Santos, B.C.D.; De Oliveira Freitas, V.; De Figueiredo, L.G.C.P.; Pereira, K.A.S.; De Lima, A.C.R.; et al. HTLV-1/2 in Indigenous Peoples of the Brazilian Amazon: Seroprevalence, Molecular Characterization and Sociobehavioral Factors Related to Risk of Infection. Viruses 2022, 15, 22. [Google Scholar] [CrossRef]
- Oliveira-Filho, A.B.; Araújo, A.P.S.; Souza, A.P.C.; Gomes, C.M.; Silva-Oliveira, G.C.; Martins, L.C.; Fischer, B.; Machado, L.F.A.; Vallinoto, A.C.R.; Ishak, R.; et al. Human T-Lymphotropic Virus 1 and 2 among People Who Used Illicit Drugs in the State of Pará, Northern Brazil. Sci. Rep. 2019, 9, 14750. [Google Scholar] [CrossRef]
- Ishak, R.; Guimarães Ishak, M.D.O.; Azevedo, V.N.; Machado, L.F.A.; Vallinoto, I.M.C.; Queiroz, M.A.F.; Costa, G.D.L.C.; Guerreiro, J.F.; Vallinoto, A.C.R. HTLV in South America: Origins of a Silent Ancient Human Infection. Virus Evol. 2020, 6, veaa053. [Google Scholar] [CrossRef]
- Islam, M.N.; Mili, M.A.; Jahan, I.; Chakma, C.; Munalisa, R. Immunological and Neurological Signatures of the Co-Infection of HIV and HTLV: Current Insights and Future Perspectives. Viruses 2025, 17, 545. [Google Scholar] [CrossRef]
- Vieira, B.A.; Bidinotto, A.B.; Dartora, W.J.; Pedrotti, L.G.; de Oliveira, V.M.; Wendland, E.M. Prevalence of Human T-Lymphotropic Virus Type 1 and 2 (HTLV-1/-2) Infection in Pregnant Women in Brazil: A Systematic Review and Meta-Analysis. Sci. Rep. 2021, 11, 15367. [Google Scholar] [CrossRef]
- Galetto, L.R.; Lunge, V.R.; Béria, J.U.; Tietzmann, D.C.; Stein, A.T.; Simon, D. Short Communication: Prevalence and Risk Factors for Human T Cell Lymphotropic Virus Infection in Southern Brazilian HIV-Positive Patients. AIDS Res. Hum. Retroviruses 2014, 30, 907–911. [Google Scholar] [CrossRef] [PubMed]
- Alencar, S.P.; de Carvalho Souza, M.; de Souza Fonseca, R.R.; Menezes, C.R.; Azevedo, V.N.; Ribeiro, A.L.R.; Lima, S.S.; Laurentino, R.V.; de Abreu Pina Barbosa, M.D.A.; Freitas, F.B.; et al. Prevalence and Molecular Epidemiology of Human T-Lymphotropic Virus (HTLV) Infection in People Living With HIV/AIDS in the Pará State, Amazon Region of Brazil. Front. Microbiol. 2020, 11, 572381. [Google Scholar] [CrossRef] [PubMed]
- Etzel, A.; Shibata, G.Y.; Rozman, M.; Jorge, M.L.; Damas, C.D.; Segurado, A.A. HTLV-1 and HTLV-2 Infections in HIV-Infected Individuals from Santos, Brazil: Seroprevalence and Risk Factors. J. Acquir. Immune Defic. Syndr. 2001, 26, 185–190. [Google Scholar] [CrossRef]
- Caterino-de-Araujo, A.; Sacchi, C.T.; Gonçalves, M.G.; Campos, K.R.; Magri, M.C.; Alencar, W.K.; Group of Surveillance and Diagnosis of HTLV of São Paulo (GSuDiHTLV-SP) Short Communication. Current Prevalence and Risk Factors Associated with Human T Lymphotropic Virus Type 1 and Human T Lymphotropic Virus Type 2 Infections Among HIV/AIDS Patients in São Paulo, Brazil. AIDS Res. Hum. Retroviruses 2015, 31, 543–549. [Google Scholar] [CrossRef]
- Tattsbridge, J.; Wiskin, C.; de Wildt, G.; Clavé Llavall, A.; Ramal-Asayag, C. HIV Understanding, Experiences and Perceptions of HIV-Positive Men Who Have Sex with Men in Amazonian Peru: A Qualitative Study. BMC Public Health 2020, 20, 728. [Google Scholar] [CrossRef]
- Zavaleta, C.; Fernández, C.; Konda, K.; Valderrama, Y.; Vermund, S.H.; Gotuzzo, E. Short Report: High Prevalence of HIV and Syphilis in a Remote Native Community of the Peruvian Amazon. Am. J. Trop. Med. Hyg. 2007, 76, 703–705. [Google Scholar] [CrossRef]
- Bartlett, E.C.; Zavaleta, C.; Fernández, C.; Razuri, H.; Vilcarromero, S.; Vermund, S.H.; Gotuzzo, E. Expansion of HIV and Syphilis into the Peruvian Amazon: A Survey of Four Communities of an Indigenous Amazonian Ethnic Group. Int. J. Infect. Dis. 2008, 12, e89–e94. [Google Scholar] [CrossRef]
- Ramos-Rincón, J.-M.; Ortiz-Martínez, S.; Vásquez-Chasnamote, M.-E.; de-Miguel-Balsa, E.; Gamboa-Paredes, O.-N.; Talledo-Albujar, M.-J.; López-Campana, G.; Celis-Salinas, J.C.; Prieto-Pérez, L.; Górgolas-Hernández, M.; et al. Screening for Human T-Cell Lymphotropic Virus (HTLV) in Pregnant Women in the Peruvian Amazon and Systematic Review with Meta-Analysis of HTLV Infection in Peru. Pathogens 2021, 10, 260. [Google Scholar] [CrossRef]
- Gotuzzo, E.; Terashima, A.; Alvarez, H.; Tello, R.; Infante, R.; Watts, D.M.; Freedman, D.O. Strongyloides Stercoralis Hyperinfection Associated with Human T Cell Lymphotropic Virus Type-1 Infection in Peru. Am. J. Trop. Med. Hyg. 1999, 60, 146–149. [Google Scholar] [CrossRef]
- Ye, L.; Taylor, G.P.; Rosadas, C. Human T-Cell Lymphotropic Virus Type 1 and Strongyloides Stercoralis Co-Infection: A Systematic Review and Meta-Analysis. Front. Med. 2022, 9, 832430. [Google Scholar] [CrossRef] [PubMed]
- Quiros-Roldan, E.; Moretti, F.; Torti, C.; Casari, S.; Castelli, F.; Beltrame, A.; Carosi, G. HIV/HTLV Co-Infection: Frequency and Epidemiological Characteristics among Patients Admitted to an Italian Hospital. Infection 2003, 31, 172–173. [Google Scholar] [CrossRef]
- Pereira, F.M.; Santos, F.L.N.; Silva, Â.A.O.; Nascimento, N.M.; da Conceição Chagas Almeida, M.; Carreiro, R.P.; Galvão-Castro, B.; Rios Grassi, M.F. Distribution of Human Immunodeficiency Virus and Human T-Leukemia Virus Co-Infection in Bahia, Brazil. Front. Med. 2021, 8, 788176. [Google Scholar] [CrossRef] [PubMed]
- La Rosa, A.M.; Zunt, J.R.; Peinado, J.; Lama, J.R.; Ton, T.G.N.; Suarez, L.; Pun, M.; Cabezas, C.; Sanchez, J. Retroviral Infection in Peruvian Men Who Have Sex with Men. Clin. Infect. Dis. 2009, 49, 112–117. [Google Scholar] [CrossRef]
- Blas, M.M.; Alva, I.E.; García, P.J.; Cárcamo, C.; Montano, S.M.; Mori, N.; Muñante, R.; Zunt, J.R. High Prevalence of Human T-Lymphotropic Virus Infection in Indigenous Women from the Peruvian Amazon. PLoS ONE 2013, 8, e73978. [Google Scholar] [CrossRef] [PubMed]
- Medeot, S.; Nates, S.; Recalde, A.; Gallego, S.; Maturano, E.; Giordano, M.; Serra, H.; Reategui, J.; Cabezas, C. Prevalence of Antibody to Human T Cell Lymphotropic Virus Types 1/2 among Aboriginal Groups Inhabiting Northern Argentina and the Amazon Region of Peru. Am. J. Trop. Med. Hyg. 1999, 60, 623–629. [Google Scholar] [CrossRef] [PubMed]
- Maloney, E.M.; Biggar, R.J.; Neel, J.V.; Taylor, M.E.; Hahn, B.H.; Shaw, G.M.; Blattner, W.A. Endemic Human T Cell Lymphotropic Virus Type II Infection among Isolated Brazilian Amerindians. J. Infect. Dis. 1992, 166, 100–107. [Google Scholar] [CrossRef]
- Fani, M.; Rezayi, M.; Meshkat, Z.; Rezaee, S.A.; Makvandi, M.; Abouzari-Lotf, E.; Ferns, G.A. Current Approaches for Detection of Human T-Lymphotropic Virus Type 1: A Systematic Review. J. Cell Physiol. 2019, 234, 12433–12441. [Google Scholar] [CrossRef]
- Campos, K.R.; Gonçalves, M.G.; Caterino-de-Araujo, A. Short Communication: Failures in Detecting HTLV-1 and HTLV-2 in Patients Infected with HIV-1. AIDS Res. Hum. Retroviruses 2017, 33, 382–385. [Google Scholar] [CrossRef]
- Hall, W.W.; Ishak, R.; Zhu, S.W.; Novoa, P.; Eiraku, N.; Takahashi, H.; da Costa Ferreira, M.; Azevedo, V.; Ishak, M.O.; da Costa Ferreira, O.; et al. Human T Lymphotropic Virus Type II (HTLV-II): Epidemiology, Molecular Properties, and Clinical Features of Infection. JAIDS J. Acquir. Immune Defic. Syndr. 1996, 13 (Suppl. S1), S204–S214. [Google Scholar] [CrossRef]
- Sanchez-Palacios, C. Seroprevalence and Risk Factors for Human T-Cell Lymphotropic Virus (HTLV-I) Infection among Ethnically and Geographically Diverse Peruvian Women. Int. J. Infect. Dis. 2003, 7, 132–137. [Google Scholar] [CrossRef]
- Miranda, C.; Utsch-Gonçalves, D.; Piassi, F.C.C.; Loureiro, P.; Gomes, I.; Ribeiro, M.A.; de Almeida-Neto, C.; Blatyta, P.; Amorim, L.; Garcia Mateos, S.O.; et al. Prevalence and Risk Factors for Human T-Cell Lymphotropic Virus (HTLV) in Blood Donors in Brazil—A 10-Year Study (2007–2016). Front. Med. 2022, 9, 844265. [Google Scholar] [CrossRef] [PubMed]
- Valcarcel, B.; Enriquez-Vera, D.; De-la-Cruz-Ku, G.; Chambergo-Michilot, D.; Calderón-Huaycochea, H.; Malpica, L. Epidemiological Features and Outcomes of HTLV-1 Carriers Diagnosed With Cancer: A Retrospective Cohort Study in an Endemic Country. JCO Glob. Oncol. 2023, 9, e2200369. [Google Scholar] [CrossRef] [PubMed]
- Cholette, F.; Périnet, S.; Neufeld, B.; Bryson, M.; Macri, J.; Sibley, K.M.; Kim, J.; Driedger, S.M.; Becker, M.L.; Sandstrom, P.; et al. Validity of Dried Blood Spot Testing for Sexually Transmitted and Blood-Borne Infections: A Narrative Systematic Review. PLoS Glob. Public Health 2024, 4, e0003320. [Google Scholar] [CrossRef] [PubMed]

| Variables | Overall (N = 293) | HTLV Positive (N = 14) | HTLV Negative (N = 279) | p Value |
|---|---|---|---|---|
| Epidemiology | ||||
| Sex, male, n (%) | 196 (66.9%) | 9 (64.3) | 187 (66,9) | 0.789 |
| Age, median (IQR), years | 40 (30–49) | 55 (52–61) | 39 (29–47) | <0.001 |
| Age ≥ 50 years, n (%) | 72 (24.6) | 12 (85.7) | 60 (21.5) | <0.001 |
| Residence, n (%) | ||||
| Iquitos district | 97 (33.1) | 7 (50.0) | 90 (32.3) | 0.932 |
| Punchana district | 84 (28.7) | 4 (28.6) | 80 (28.7) | |
| San Juan district | 64 (21.8) | 1 (7.1) | 63 (22.6) | |
| Belen district | 33 (11.3) | 2 (14.3) | 31 (11.1) | |
| Outside of Iquitos city | 15 (5.1) | 0 (0.0) | 15 (5.3) | |
| Occupation, n (%) | ||||
| Unemployed or student | 111 (37.9) | 5 (35.7) | 106 (38.0) | 0.54 |
| Self-employment | 100 (34.1) | 5 (35.7) | 95 (34.1) | |
| Cattle, agriculture or construction | 47 (16.0) | 3 (21.4) | 44 (15.8) | |
| Intellectual work | 28 (9.8) | 0 (0.0) | 28 (10.7) | |
| Craft work | 7 (2.4) | 1 (7.1) | 6 (2.2) | |
| Education, n (%) | ||||
| None or only attended primary school | 49 (16.7) | 5 (35.7) | 44 (15.8) | 0.05 |
| Attended secondary school or university | 244 (83.3) | 9 (64.3) | 235 (84.2) | |
| Epidemiological risk factors, n (%) | ||||
| Breastfeeding | 277 (94.5) | 13 (92.9) | 264 (94.6) | 0.55 |
| Blood transfusion | 64 (21.8) | 3 (21.4) | 61 (21.9) | 1.0 |
| Comorbidity, n (%) | ||||
| Diabetes or high blood pressure | 21 (7.2) | 2 (14.3) | 19 (6.8) | 0.26 |
| Digestive disease | 12 (4.1) | 2 (14.3) | 10 (3.6) | 0.10 |
| Other cardiovascular disease | 10 (3.49) | 1 (7.1) | 9 (3.2) | 0.39 |
| Previous infections, n (%) | ||||
| Strongyloides serology positive | 167 (57.0) | 6 (42.9) | 161 (57.7) | 0.29 |
| Tuberculosis test positive | 55 (18.8) | 4 (28.6) | 51 (18.3) | 0.30 |
| Prior gonorrhea | 33 (11.3) | 3 (21.4) | 30 (10.8) | 0.20 |
| Prior syphilis | 41 (14.0) | 3 (21.3) | 38 (13.6) | 0.42 |
| Chronic hepatitis | 19 (6.5) | 2 (14.3) | 17 (6.7) | 0.23 |
| Prior cerebral toxoplasmosis | 13 (4.4) | 0 (0.0) | 13 (4.7) | 0.41 |
| HIV acquisition, n (%) | ||||
| Sexual | 263 (89.9) | 12 (85.7) | 251 (90.0) | 0.71 |
| Vertical | 2 (1.0) | 0 (0.0) | 3 (1.1) | |
| Unknown | 27 (9.2) | 2 (14.39 | 25 (9.0) | |
| Virology, Immunology and Adherence of Treatment | ||||
| Nadir CD4+/uL, median (IQR) | 228 (109–363) | 213 (123–360) | 230 (109–363) | 0.91 |
| Current CD4+, median (IQR) | 446 (303–597) | 455 (385–613) | 441 (299–593) | 0.47 |
| Current CD4+ < 200/mL n (%) | 22 (10.7) | 0 (0.0) | 22 (11.3) | 0.61 |
| Current undetectable HIV viral load (<20 copies/mL), n (%) | 216 (76.3) | 12 (92.39 | 204 (75.6) | 0.31 |
| Poor ART adherence, ≤95%), n (%) | 22 (13.4) | 2 (15.4) | 30 (13.3) | 0.89 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Otero-Rodriguez, S.; Casapia-Morales, M.; de Mendoza, C.; Pinedo-Cancino, V.; Mego-Campos, S.; Soriano, V.; Merino, E.; Ramos-Rincón, J.-M. High Rate of Human T-Cell Lymphotropic Virus-2 in Patients with HIV in the Peruvian Amazon. Trop. Med. Infect. Dis. 2025, 10, 267. https://doi.org/10.3390/tropicalmed10090267
Otero-Rodriguez S, Casapia-Morales M, de Mendoza C, Pinedo-Cancino V, Mego-Campos S, Soriano V, Merino E, Ramos-Rincón J-M. High Rate of Human T-Cell Lymphotropic Virus-2 in Patients with HIV in the Peruvian Amazon. Tropical Medicine and Infectious Disease. 2025; 10(9):267. https://doi.org/10.3390/tropicalmed10090267
Chicago/Turabian StyleOtero-Rodriguez, Silvia, Martin Casapia-Morales, Carmen de Mendoza, Viviana Pinedo-Cancino, Seyer Mego-Campos, Vicente Soriano, Esperanza Merino, and José-Manuel Ramos-Rincón. 2025. "High Rate of Human T-Cell Lymphotropic Virus-2 in Patients with HIV in the Peruvian Amazon" Tropical Medicine and Infectious Disease 10, no. 9: 267. https://doi.org/10.3390/tropicalmed10090267
APA StyleOtero-Rodriguez, S., Casapia-Morales, M., de Mendoza, C., Pinedo-Cancino, V., Mego-Campos, S., Soriano, V., Merino, E., & Ramos-Rincón, J.-M. (2025). High Rate of Human T-Cell Lymphotropic Virus-2 in Patients with HIV in the Peruvian Amazon. Tropical Medicine and Infectious Disease, 10(9), 267. https://doi.org/10.3390/tropicalmed10090267









