Hospital Resilience in a Multi-Hazard Era: Water Security Planning in Northern Thailand
Abstract
1. Introduction
1.1. Global Context
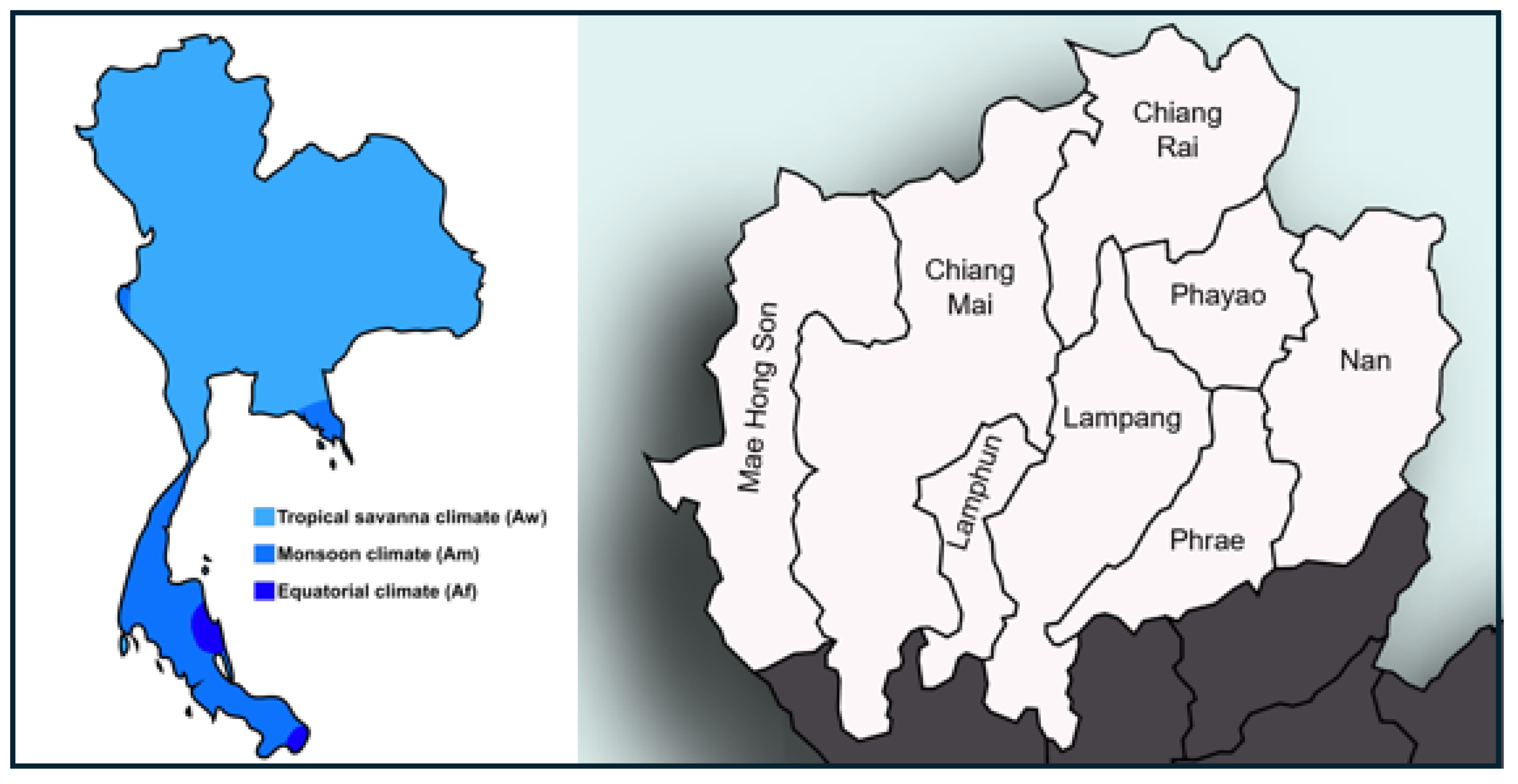
1.2. Thailand Context
1.3. Objectives
- What are the typical patterns of water use in hospitals across northern Thailand, and how do they compare with international benchmarks?
- To what extent did hospitals experience water shortages during the 2019–2020 compound drought–pandemic period?
- What preparedness and adaptation strategies are needed to improve hospital water security and resilience?
2. Background
2.1. Water Availability
2.2. Drought and Flood Risk
2.3. Water Supply Management in Thailand
2.4. Overview of the Thai Hospital System
3. Materials and Methods
3.1. Data Collection
3.2. Response
4. Findings
4.1. Hospitals Reporting COVID-19 Activity
4.2. Water Use Patterns
4.3. Water Sufficiency, Quality, and Planning
5. Discussion
5.1. Efficiency, Strategic Planning, and Risk Reduction
5.2. Hazard Management Team Model
5.3. Sustainability Issues
5.4. Limitations
6. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Information Sought from Hospital Administrators for the Study
- Timestamp
- Name of your hospital
- Province in which your hospital is located
- What is the level/type of your hospital?
- How many patient beds does your hospital have?
- Has your hospital been designated to screen or admit COVID-19 patients?
- How sufficient is your hospital’s water supply?
- What is your hospital’s primary water source?
- Does your hospital have sufficient water quantity and quality for its needs?
- Does your hospital use any water recycling or reuse techniques to augment supply?
- Has drought affected water sufficiency at your hospital?
- Has the COVID-19 situation further affected your hospital’s water sufficiency?
- Does your hospital have a water management plan (describe)?
- Does your hospital have a water management plan specifically for crisis or disaster scenarios?
- During the drought and COVID-19 situation, has your hospital implemented additional water management measures beyond normal operations (describe)?
- Are there any government measures or policies supporting your hospital’s water use?
- What is your hospital’s average monthly water consumption (in volume)?
- What is your hospital’s average water use per patient?
Appendix B. Additional Information That Could Be Collected to Study Water Consumption
- 19.
- Types of services offered (e.g., emergency, surgery, long-term care, maternity, dialysis, intensive care).
- 20.
- Total number of beds and average occupancy rate (%).
- 21.
- Total number of staff (clinical, administrative, cleaning, etc.).
- 22.
- Total built area (m2) and site area (outdoor grounds if irrigated).
- 23.
- Main water supply source(s) (municipal well, surface water, rainwater, etc.).
- 24.
- Drinking water source and treatment method (e.g., RO, UV, bottled).
- 25.
- Use of filtered vs. unfiltered water (with specification of treatment technologies).
- 26.
- Monthly water usage disaggregated by season or key operational periods.
- 27.
- Average daily water use per patient (per inpatients, outpatients, ICU patients).
- 28.
- Water use breakdown by sector (e.g., kitchen, laundry, HVAC, sterilization, patient care, sanitation).
- 29.
- Greywater recovery or recycling (volume, use areas, treatment method).
- 30.
- Presence of water-efficient fixtures/retrofits (e.g., low-flow taps, sensor-based flush).
- 31.
- Water loss monitoring and control (e.g., leaks, overflow prevention systems).
- 32.
- Type of wastewater treatment (onsite, municipal, septic, advanced treatment).
- 33.
- Separation or special handling for high-risk wastewater (e.g., infectious disease wards, labs, radioactive waste).
- 34.
- Wastewater reuse (if any) and discharge standards compliance.
- 35.
- Water budget (annual cost, allocation by sector if available).
- 36.
- Emergency and drought contingency measures (e.g., water trucks, prioritized services, emergency tanks).
References
- Milsten, A. Hospital Responses to Acute-Onset Disasters: A Review. Prehospital Disaster Med. 2000, 15, 40–53. [Google Scholar] [CrossRef]
- Hsu, J.; Del Rosario, M.C.; Thomasson, E.; Bixler, D.; Haddy, L.; Duncan, M.A. Hospital impact after a chemical spill that compromised the potable water supply: West Virginia, January 2014. Disaster Med. Public Health Prep. 2017, 11, 621–624. [Google Scholar] [CrossRef] [PubMed]
- Bross, L.; Bäumer, J.; Voggenreiter, I.; Wienand, I.; Fekete, A. Public Health without Water? Emergency Water Supply and Minimum Supply Standards of Hospitals in High-Income Countries Using the Example of Germany and Austria. Water Policy 2021, 23, 205–221. [Google Scholar] [CrossRef]
- van der Heijden, S.; Cassivi, A.; Mayer, A.; Sandholz, S. Water Supply Emergency Preparedness and Response in Health Care Facilities: A Systematic Review on International Evidence. Front. Public Health 2022, 10, 1035212. [Google Scholar] [CrossRef]
- Luke, J.; Franklin, R.C.; Dyson, J.; Aitken, P. Building Toward a Disaster Resilient Health System: A Study of Hospital Resilience. Disaster Med. Public Health Prep. 2023, 17, e219. [Google Scholar] [CrossRef] [PubMed]
- Krause, S.; Joel, E.; Schaum, C.; Bäumer, J.; Rücker, N.; Wienand, I.; Sturm, C.; Jahn-Mühl, B.; Geiger, M.; Fekete, A.; et al. Water safety planning for healthcare facilities for extreme events. J. Water Health 2024, 22, 77–96. [Google Scholar] [CrossRef] [PubMed]
- Grigoletto, J.C.; Cabral, A.R.; Bonfim, C.V.; Rohlfs, D.B.; Silva, E.L.; Queiroz, F.B.D.; Magalhães, T.D.B. Management of Health Sector Actions in Drought Situations. Ciênc. Saúde Colet. 2016, 21, 709–718. [Google Scholar] [CrossRef]
- Wijesekara, N.W.A.N.Y.; Wedamulla, A.; Perera, S.; Pesigan, A.; Ofrin, R.H. Assessment of Drought Resilience of Hospitals in Sri Lanka: A Cross-Sectional Survey. WHO South-East Asia J. Public Health 2020, 9, 66–72. [Google Scholar] [CrossRef]
- Barten, D.G.; Paganini, M.; Khorram-Manesh, A.; Leledakis, G.; Ciottone, G. Hospital Vulnerabilities to a Changing Climate: Extreme Heat, Droughts, and Wildfires. Eur. J. Emerg. Med. 2024, 31, 383–384. [Google Scholar] [CrossRef]
- The Hindu Business Line. India’s Worsening Drought Forces Hospitals to Buy Water for Surgery. The Hindu Bus. Line 2020. Available online: https://www.thehindubusinessline.com/news/indias-worsening-drought-forces-hospitals-to-buy-water-for-surgery/article28350428.ece (accessed on 18 March 2025).
- The Jakarta Post. Millions Hit in Manila’s ‘Worst’ Water Shortage. Jakarta Post 2019. Available online: https://www.thejakartapost.com/seasia/2019/03/16/millions-hit-in-manilas-worst-water-shortage.html (accessed on 23 March 2025).
- Thackray, L. Water Quality and Availability Concerns in Drought for Dialysis Patients. ABC News 2019. Available online: https://www.abc.net.au/news/2019-07-15/dialysis-concerns-about-the-impact-of-water-shortage/11310952 (accessed on 20 March 2025).
- Njeru, G. Kenya’s Climate Change Water Crisis Impacts Hospital Maternal Care. Women News Network (WNN) 2010. Available online: https://truthout.org/articles/kenyas-climate-change-water-crisis-impacts-hospital-maternal-care/ (accessed on 20 March 2025).
- Bangkok Post. Nine Hospitals Face Water Shortages. Bangkok Post 2020. Available online: https://www.bangkokpost.com/thailand/general/1839194/nine-hospitals-face-water-shortages (accessed on 13 March 2025).
- Bangkok Post. Thailand Tackles Worst Drought in 40 Years. Bangkok Post 2020. Available online: https://www.bangkokpost.com/business/1853069/thailand-tackles-worst-drought-in-40-years (accessed on 23 March 2025).
- Bangkok Post. Relief Urged for Looming Water Crisis. Bangkok Post 2019. Available online: https://www.bangkokpost.com/thailand/general/1717039/relief-urged-for-looming-water-crisis (accessed on 18 May 2025).
- Bangkok Post. Surin Hospital Water Crisis ‘Relieved’, Prawit Says. Bangkok Post 2019. Available online: https://www.bangkokpost.com/thailand/general/1729535/surin-hospital-water-crisis-relieved-prawit-says (accessed on 23 February 2025).
- The Nation. Wells Dug to Provide Surin Hospital with Essential Water Supply. The Nation 2019. Available online: https://www.nationthailand.com/news/30374660 (accessed on 23 May 2025).
- Bangkok Post. Hospitals Hit by Water Crisis. Bangkok Post 2016. Available online: https://www.bangkokpost.com/thailand/general/872608/hospitals-hit-by-water-crisis (accessed on 23 February 2025).
- Berman, J.D.; Ebisu, K.; Peng, R.D.; Dominici, F.; Bell, M.L. Drought and the risk of hospital admissions and mortality in older adults in western USA from 2000 to 2013: A retrospective study. Lancet Planet. Health 2017, 1, e17–e25. [Google Scholar] [CrossRef]
- IPCC. Climate Change 2022: Impacts, Adaptation and Vulnerability. Intergovernmental Panel on Climate Change. Available online: https://www.ipcc.ch/report/sixth-assessment-report-working-group-ii/ (accessed on 11 March 2020).
- Hydro DataSci Section. Thailand Water Situation 2020; Royal Irrigation Department: Bangkok, Thailand, 2021; Available online: https://www.thaiwater.net/uploads/contents/current/YearlyReport2020/summary.html (accessed on 4 June 2025).
- Intawong, K.; Olson, D.; Chariyalertsak, S. Application Technology to Fight the COVID-19 Pandemic: Lessons Learned in Thailand. Biochem. Biophys. Res. Commun. 2021, 534, 830–836. [Google Scholar] [CrossRef] [PubMed]
- Apipattanavis, S.; Ketpratoom, S.; Kladkempetch, P. Water management in Thailand. Irrig. Drain. 2018, 67, 113–117. [Google Scholar] [CrossRef]
- Hayes, M.; Wilhelmi, O.; Knutson, C. Reducing Drought Disk: Bridging Theory and Practice. Nat. Hazards Rev. 2004, 5, 106–113. [Google Scholar] [CrossRef]
- Aquaduct. World Resource Institute. Available online: https://www.wri.org/aqueduct (accessed on 17 June 2025).
- Luo, T.; Young, R.; Reig, P. Aqueduct Projected Water Stress Country Rankings; Technical Note; World Resources Institute: Washington, DC, USA, 2015; Available online: https://www.wri.org/data/aqueduct-projected-water-stress-country-rankings (accessed on 17 June 2025).
- Lim, H.S.; Boochabun, K.; Ziegler, A. Modifiers and Amplifiers of High and Low Flows on the Ping River in Northern Thailand (1921–2009): The Roles of Climatic Events and Anthropogenic Activity. Water Resour. Manag. 2012, 26, 1177–1194. [Google Scholar] [CrossRef]
- Reliefweb. PM Prayut Orders All Units to Help Flood-Hit People in North. Reliefweb 2020. Available online: https://reliefweb.int/report/thailand/pm-prayut-orders-all-units-help-flood-hit-people-north (accessed on 25 August 2020).
- Chuah, C.J.; Ziegler, A.D. Temporal variability of faecal contamination from on-site sanitation systems in the groundwater of northern Thailand. Environ. Manag. 2018, 61, 939–953. [Google Scholar] [CrossRef]
- Kruawal, K.; Sacher, F.; Werner, A.; Müller, J.; Knepper, T.P. Chemical Water Quality in Thailand and Its Impacts on the Drinking Water Production. Sci. Total Environ. 2005, 340, 57–70. [Google Scholar] [CrossRef] [PubMed]
- Prakirake, C.; Chaiprasert, P.; Tripetchkul, S. Development of Specific Water Quality Index for Water Supply in Thailand. Songklanakarin J. Sci. Technol. 2009, 31, 91–104. [Google Scholar]
- Ministry of Public Health (MoPH). Health Service System of Thailand. Office of the Permanent Secretary, Ministry of Public Health, Nonthaburi, Thailand. 2016. Available online: https://hss.moph.go.th/fileupload_doc_slider/2016-12-08--465.pdf (accessed on 8 June 2025).
- Boonmee, C.; Kasemset, C. The Improvement of Healthcare Management in Thailand via IE Tools: A Survey. In Proceedings of the International Conference on Industrial Engineering and Operations Management, Bangkok, Thailand, 5–7 March 2019; IEOM Society International: Bangkok, Thailand, 2019. [Google Scholar]
- Tangcharoensathien, V.; Witthayapipopsakul, W.; Panichkriangkrai, W.; Patcharanarumol, W.; Mills, A. Health Systems Development in Thailand: A Solid Platform for Successful Implementation of Universal Health Coverage. Lancet 2018, 391, 1205–1223. [Google Scholar] [CrossRef]
- Batista, K.J.M.; Rosa da Silva, S.; Rabbani, E.R.K.; Zlatar, T. Systematic Review of Indicators for the Assessment of Water Consumption Rates at Hospitals. Water Supply 2020, 20, 373–382. [Google Scholar] [CrossRef]
- González, A.G.; García-Sanz-Calcedo, J.; Salgado, D.R. Quantitative Determination of Potable Cold Water Consumption in German Hospitals. Sustainability 2018, 10, 932. [Google Scholar] [CrossRef]
- Heyne, L. Energieverbrauch undkosten auf dem Prüfstand [Consumption and Costs of Energy and Water Assessed]. Krankenh. Tech. 1995, 6, 101–106. [Google Scholar]
- Dettenkofer, M.; Kuemmerer, K.; Schuster, A.; Mueller, W.; Muehlich, M.; Scherrer, M.; Daschner, F.D. Environmental Auditing in Hospitals: First Results in a University Hospital. Environ. Manag. 2000, 25, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Collett, S.; Samarin, I.; Bhalchandra, R.; Soundaranayagam, J.; Garai, S.; Chandy, M.; Bhattachary, S. Water Usage in a Multi-Speciality Hospital and Its Effective Management. J. Acad. Clin. Microbiol. 2016, 18, 135. [Google Scholar] [CrossRef]
- D’Alessandro, D.; Tedesco, P.; Rebecchi, A. Water Use and Water Saving in Italian Hospitals: A Preliminary Investigation. Ann. Ist. Super. Sanità 2016, 52, 56–62. [Google Scholar] [CrossRef]
- Mohee, R. Medical Wastes Characterisation in Healthcare Institutions in Mauritius. Waste Manag. 2005, 25, 575–581. [Google Scholar] [CrossRef]
- Oliveira, C.A.G.R. Water Supply to Portuguese Regional Hospitals: A Contribution for the Knowledge of the Water Consumption Patterns in Portuguese Regional Hospitals. Ph.D. Thesis, Kingston University, Kingston, UK, 2010. [Google Scholar]
- González, A.G.; García-Sanz-Calcedo, J.; Salgado, D.R.; Mena, A. A Quantitative Analysis of Cold Water for Human Consumption in Hospitals in Spain. J. Healthc. Eng. 2016, 2016, 6534823. [Google Scholar] [CrossRef]
- García-Sanz-Calcedo, J.; López-Rodríguez, F.; Yusaf, T.F.; Al-Kassir, A. Analysis of the Average Annual Consumption of Water in the Hospitals of Extremadura (Spain). Energies 2017, 10, 479. [Google Scholar] [CrossRef]
- Gómez-Chaparro, M.; García Sanz-Calcedo, J.; Armenta-Márquez, L. Study on the Use and Consumption of Water in Spanish Private Hospitals as Related to Healthcare Activity. Urban Water J. 2018, 15, 963–970. [Google Scholar] [CrossRef]
- Teksoy, A.; Altan, K. Assessment of Sustainable Water Management in Public Hospitals: The Case of Turkey. Environ. Eng. Manag. J. 2022, 21, 1751–1760. [Google Scholar] [CrossRef]
- CBCL Limited. Study on Water Quality and Demand on Public Water Supplies with Variable Flow Regimes and Water Demand. 2011. Available online: https://www.gov.nl.ca/ecc/files/waterres-training-adww-decade-16-stephanie-gora.pdf (accessed on 6 June 2025).
- Washington State Department of Health. Water Design Manual. DOH Pub 331-123. Revised June 2020. Available online: https://doh.wa.gov/sites/default/files/2022-02/331-123.pdf (accessed on 9 June 2025).
- Sänger, N.; Heinzel, C.; Sandholz, S. Advancing Resilience of Critical Health Infrastructures to Cascading Impacts of Water Supply Outages—Insights from a Systematic Literature Review. Infrastructures 2021, 6, 177. [Google Scholar] [CrossRef]
- Shahverdi, B.; Tariverdi, M.; Miller-Hooks, E. Assessing Hospital System Resilience to Disaster Events Involving Physical Damage and Demand Surge. Socio-Econ. Plan. Sci. 2019, 68, 100708. [Google Scholar] [CrossRef]
- Chand, A.M.; Loosemore, M. A Socio-Ecological Analysis of Hospital Resilience to Extreme Weather Events. Constr. Manag. Econ. 2015, 33, 907–920. [Google Scholar] [CrossRef]
- Bezuidenhout, S.T.; Dippenaar, A. The Development of a Robust Risk Management Plan for the Continuous Supply of Water to Hospitals in the Western Cape Province. S. Afr. J. Ind. Eng. 2019, 30, 190–204. [Google Scholar] [CrossRef]
- McGain, F.; Naylor, C. Environmental sustainability in hospitals—A systematic review and research agenda. J. Health Serv. Res. Policy 2014, 19, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Priyalal, W.G.S.S.; de Silva, M.L.; Rajini, P.A.D. A Study on Water Management Strategies Practiced in Healthcare Facilities: A Literature Review. In Proceedings of the 6th International Conference on Structural Engineering and Construction Management (ICSECM 2015), Kandy, Sri Lanka, 11–13 December 2015. [Google Scholar]
- CDC/AWWA. Emergency Water Supply Planning Guide for Hospitals and Healthcare Facilities, Updated 2019 ed.; U.S. Department of Health and Human Services: Atlanta, GA, USA, 2019. Available online: https://www.cdc.gov/water-emergency/hcp/toolkit/index.html (accessed on 23 March 2025).
- Welter, G.; Bieber, S.; Bonnaffon, H.; Deguida, N.; Socher, M. Cross-sector emergency planning for water providers and healthcare facilities. J. AWWA 2010, 102, 68–78. [Google Scholar] [CrossRef]
- Achour, N.; Miyajima, M.; Pascale, F.; Price, A.D.F. Hospital resilience to natural hazards: Classification and performance of utilities. Disaster Prev. Manag. 2014, 23, 40–52. [Google Scholar] [CrossRef]
- Quintana, A.V.; Mayhew, S.H.; Kovats, S.; Gilson, L. Resilient Health Systems in Action: How Actor Relationships and Organizational Qdaptation Shaped the Health Sector’s Response to the 2015–2018 Western Cape Drought. Oxf. Open Clim. Change 2025, 5, kgaf014. [Google Scholar] [CrossRef]
- Agar, D.A. Personal viewpoint: Hemodialysis—Water, power, and waste disposal: Rethinking our environmental responsibilities. Hemodial. Int. 2012, 16, 6–10. [Google Scholar] [CrossRef]
- Pynkyawati, T.; Suwito, R.J.; Firmansyah, H.; Rachmabillah, M.S. Sustainable Concept Application to Wastewater Treatment in NURI Building at Dr. M. Salamun Bandung Hospital. J. Archit. Res. Educ. 2020, 2, 72–81. [Google Scholar] [CrossRef]
- de Lima da Silva, A.M.; Gomes Costa, B.; Muniz Machado, A.V.; Souza Carvalho, P.A.; Oliveira de Farias, R. Reuse of Grey Water and rainwater in Health Units: A Case Study in Upas in the Municipality of São Gonçalo. Environ. Soc. Manag. J./Rev. Gestão Soc. Ambient. 2025, 19, 1–11. [Google Scholar] [CrossRef]
- Altin, A.; Altin, S. Sustainable Water and Wastewater Management in Hospitals. Turk. J. Occup. Environ. Med. Saf. 2017, 2, 1–7. [Google Scholar]
- Corvalan, C.; Hales, S.; Xuereb, P. Climate Resilient Health Systems: Towards Climate Resilient and Environmentally Sustainable Health Care Facilities. Int. J. Environ. Res. Public Health 2020, 17, 17–8849. [Google Scholar] [CrossRef] [PubMed]
- Chías, P.; Abad, T. Green hospitals, green healthcare. Int. J. Energy Prod. Manag. 2017, 2, 196–205. [Google Scholar] [CrossRef]
- Al Shamas, M.R. Evaluation of Sustainability Standards in Hospital Design: Case Study in Jordan. Master’s Thesis, Faculty of Engineering, Isra University, Amman, Jordon, 2020; 120p. [Google Scholar]
- Abbasi, F.; Samaei, M.R.; Mehdizadeh, A. The Main Challenges and Suggested Solutions for Optimization of Water Management in an Educational hospital. J. Environ. Health Sustain. Dev. 2018, 3, 585–592. [Google Scholar]
- Vallée, M. Green hospitals face to climate change: Between sobriety and resilience. Heliyon 2024, 10, e24769. [Google Scholar] [CrossRef]
- Pascale, F.; Achour, N. Envisioning the Sustainable and Climate Resilient Hospital of the Future. Public Health 2024, 237, 435–442. [Google Scholar] [CrossRef]
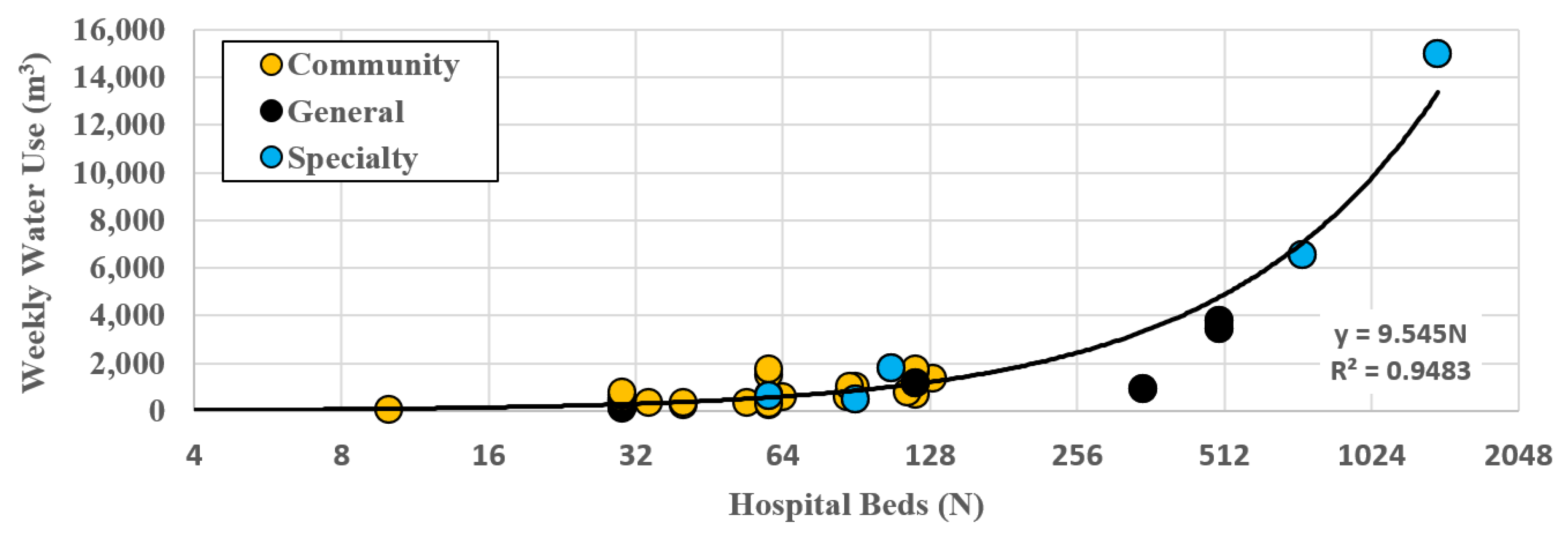
| Median | Min | Max | IQR | |
|---|---|---|---|---|
| All Hospitals (67) | 460 | 69 | 14,959 | 306–777 |
| Community Hospitals (58) | 414 | 69 | 2992 | 269–621 |
| General Hospitals (4) | 2301 | 921 | 3797 | 1093–3538 |
| Specialty Hospitals (5) | 1202 | 312 | 14,959 | 513–5341 |
| Median | Min | Max | IQR | |
|---|---|---|---|---|
| All Hospitals (67) | 9.2 | 2.6 | 28.8 | 6.9–12.1 |
| Community Hospitals (58) | 9.2 | 3.5 | 28.8 | 6.9–12.4 |
| General Hospitals (4) | 7.3 | 2.6 | 9.6 | 5.8–8.1 |
| Specialty Hospitals (5) | 10.6 | 5.3 | 20.8 | 9.2–15.2 |
| Country | Hospital Count | Bed ** Number | Water Use ** (m3/Bed/Week) | Study Focus | Hospital Type |
|---|---|---|---|---|---|
| Thailand * | 67 | 34 (10–1400) | 9.6 (2.6–28.8) | Total water usage | Various |
| Germany [37] | 19 | 396 (45–1003) | 2.7 (2.2–4.3) | Water consumption | Various |
| Germany [38] | 64 | NA | 2.8 (1.0–4.8) | Water consumption | Unknown |
| Germany [39] | 1 | 1709 | 5.7 | Water consumption | University |
| India [40] | 1 | 183 | 7.8 | Filtered water use | Cancer |
| Italy [41] | 36 | 383 | 8.8 | Water use | Public |
| Mauritius [42] | 1 | 435 | 4.5 | Water audit | Unknown |
| Portugal [43] | 1 | 776 | 8.3 | Water consumption | Regional |
| Spain [44] | 20 | 39 (193–1075) | 4.1. (1.2–7.6) | Water consumption | Mixed |
| Spain [45] | 13 | ~30–500 | 5.0 | Water consumption | Unknown |
| Spain [46] | 14 | 20–194 | 2.2 | Water consumption | Private |
| Turkey [47] | 13 | 169 (5–810) | 3.7 | Total water usage | Public |
| n | Planned Action |
|---|---|
| 20 | Build a water reserve system (tanks or reservoir) * |
| 15 | Drill a well |
| 5 | Connect to Provincial Water Authority system |
| 3 | Request a water vehicle from the municipality |
| 2 | Connect with municipal water supply system |
| 2 | Request raw water from the municipality (e.g., via tank truck) |
| 1 | Drill a well and connect with the Provincial Water Authority system |
| 1 | Drill a well and request a water truck from the municipality |
| 1 | Build a water reserve system and request a water truck from the municipality * |
| 1 | Build a rainwater collection system |
| A. Governance and Planning |
|
|
|
|
|
|
| B. Infrastructure and Systems |
|
|
|
|
|
|
|
| C. Data and Monitoring |
|
|
|
| D. Operational Preparedness |
|
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ziegler, A.D.; Wangsan, K.; Supinit, P.; Potapohn, M. Hospital Resilience in a Multi-Hazard Era: Water Security Planning in Northern Thailand. Urban Sci. 2025, 9, 240. https://doi.org/10.3390/urbansci9070240
Ziegler AD, Wangsan K, Supinit P, Potapohn M. Hospital Resilience in a Multi-Hazard Era: Water Security Planning in Northern Thailand. Urban Science. 2025; 9(7):240. https://doi.org/10.3390/urbansci9070240
Chicago/Turabian StyleZiegler, Alan D., Kampanat Wangsan, Phadungpon Supinit, and Manoj Potapohn. 2025. "Hospital Resilience in a Multi-Hazard Era: Water Security Planning in Northern Thailand" Urban Science 9, no. 7: 240. https://doi.org/10.3390/urbansci9070240
APA StyleZiegler, A. D., Wangsan, K., Supinit, P., & Potapohn, M. (2025). Hospital Resilience in a Multi-Hazard Era: Water Security Planning in Northern Thailand. Urban Science, 9(7), 240. https://doi.org/10.3390/urbansci9070240






