Towards a Live Feedback Training System: Interchangeability of Orbbec Persee and Microsoft Kinect for Exercise Monitoring
Abstract
1. Introduction
2. Materials and Methods
2.1. Technical Specifications of Microsoft Kinect v2 and Orbbec Persee
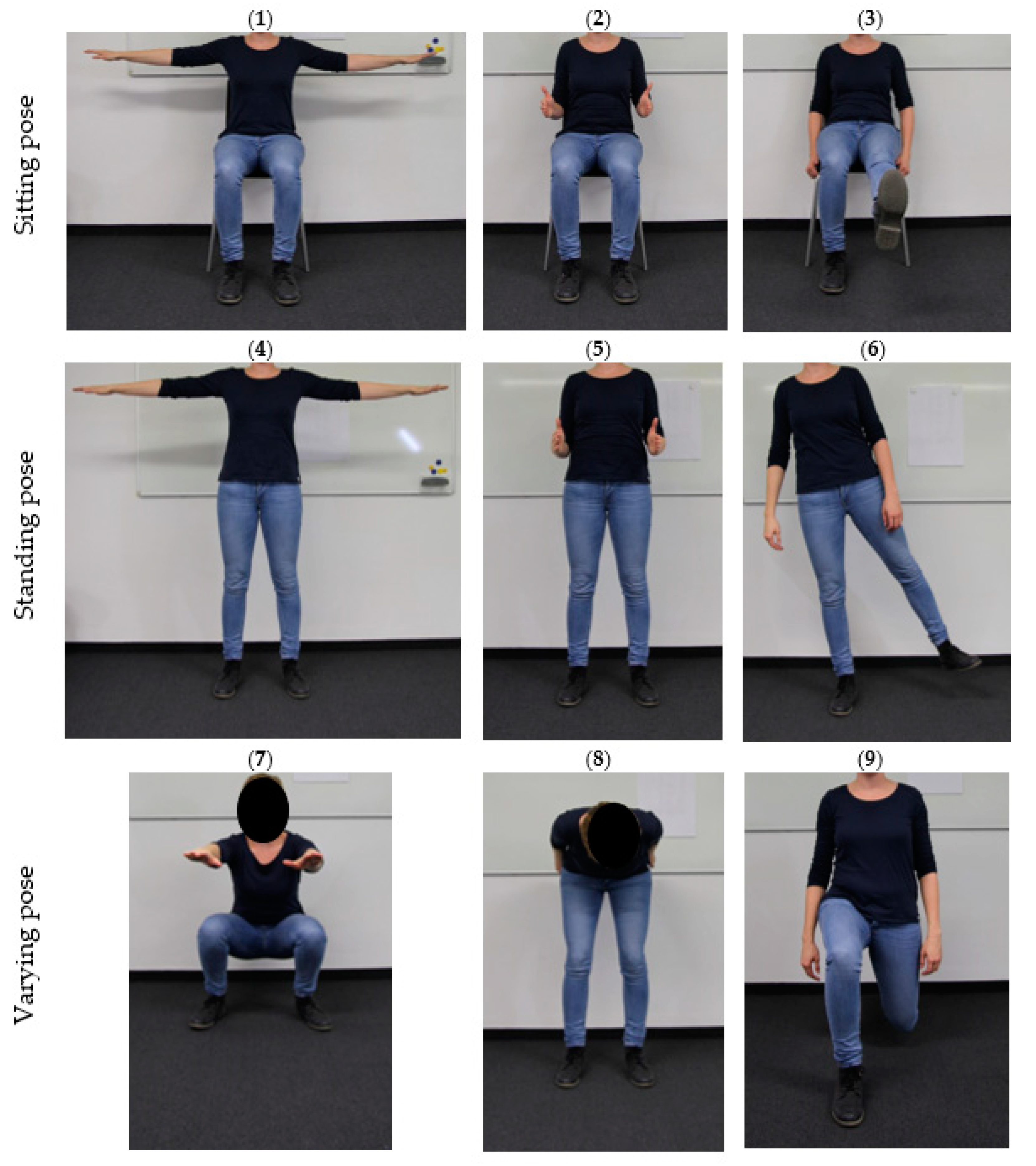
2.2. Skeleton Data Collection
2.3. Interchangeability Analysis
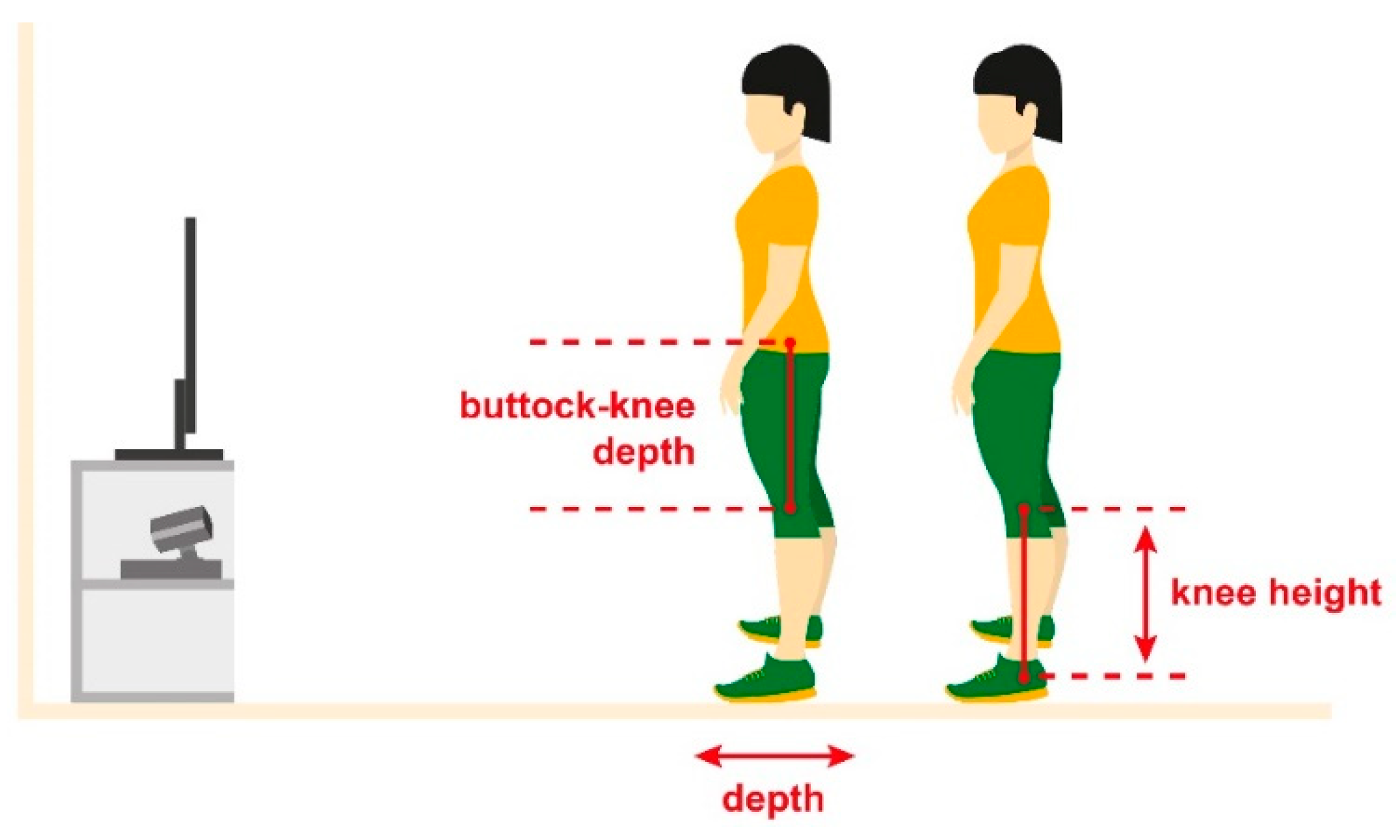
- Standing recognition (see Figure 3): In addition to the criterion that the mean buttock–knee depth information had to be less than 275 mm, the left and right knee had to be approximately at the same height with a set tolerated difference of 20 mm. This avoids a standing detection when one of the two legs is raised.
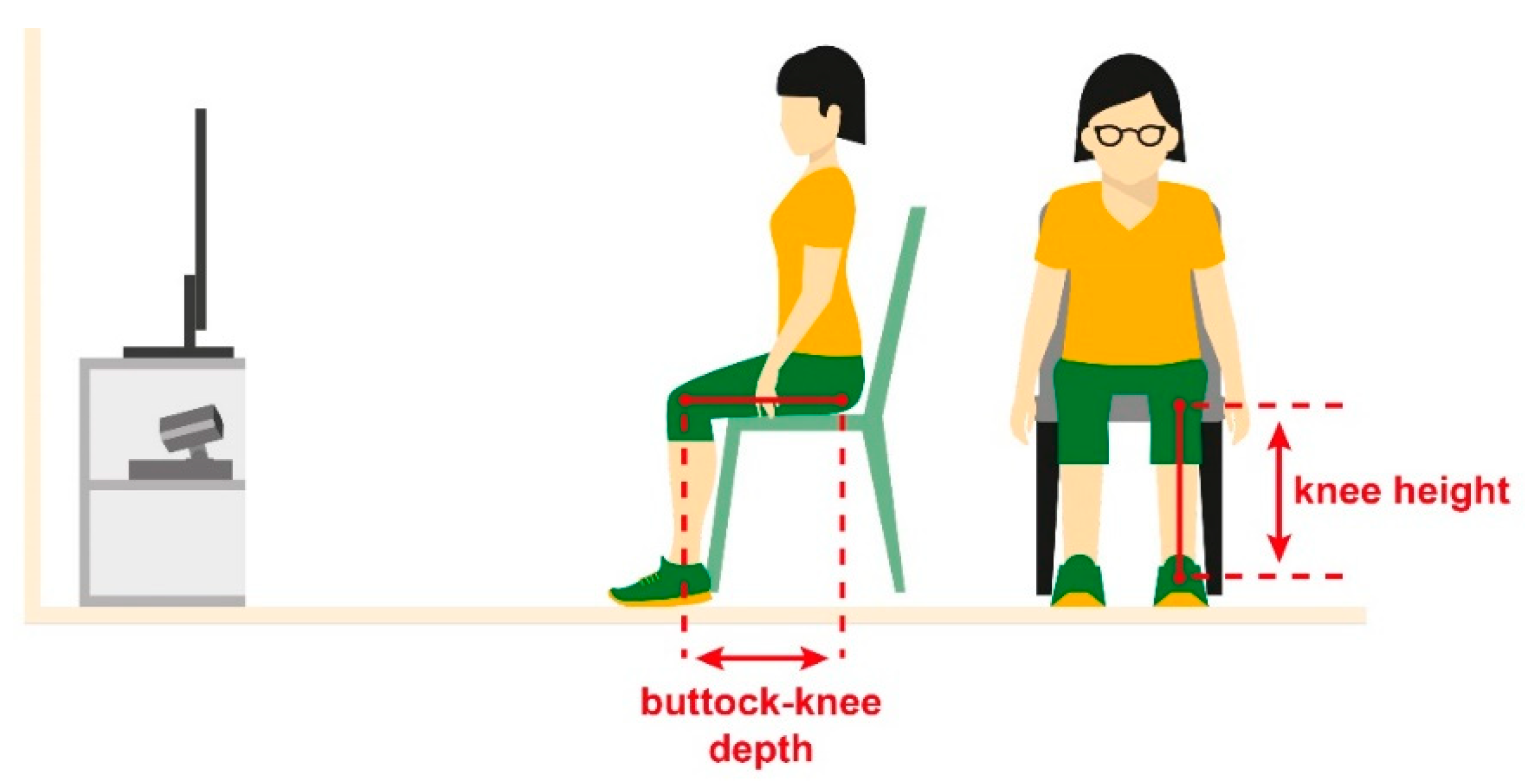
- Sitting recognition (see Figure 4): In addition to the criterion that the mean buttock–knee depth information had to be more than 275 mm, the knees had to be approximately at the same height with a tolerated difference of 20 mm. This does not only avoid detection of sitting when one of the legs is raised, but also identifies if a lunge rather than a sitting position is performed.
- Upward movement: From the starting position, joint heights along the longitudinal axis are monitored. If they exceed the transition criterion, another repetition is count.
- Lateral movement: From the starting position, joint positions along the frontal axis are monitored. If they exceed the transition criterion, another repetition is count.
- Downward movement: From the starting position, joint heights along the longitudinal axis are monitored. If they are below the transition criterion, another repetition is count.
3. Results
3.1. Tracking State Analysis
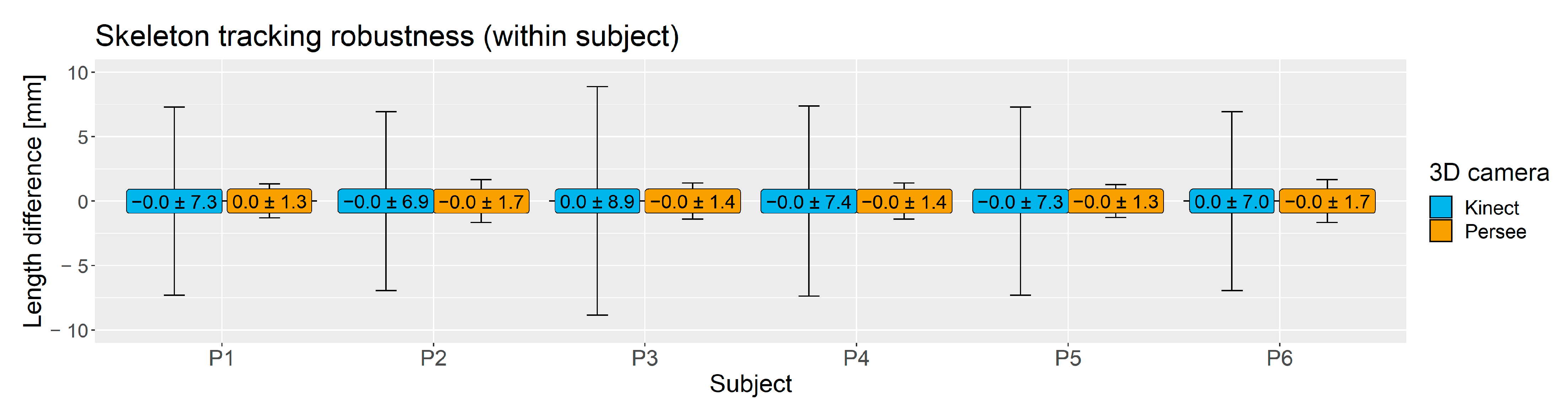
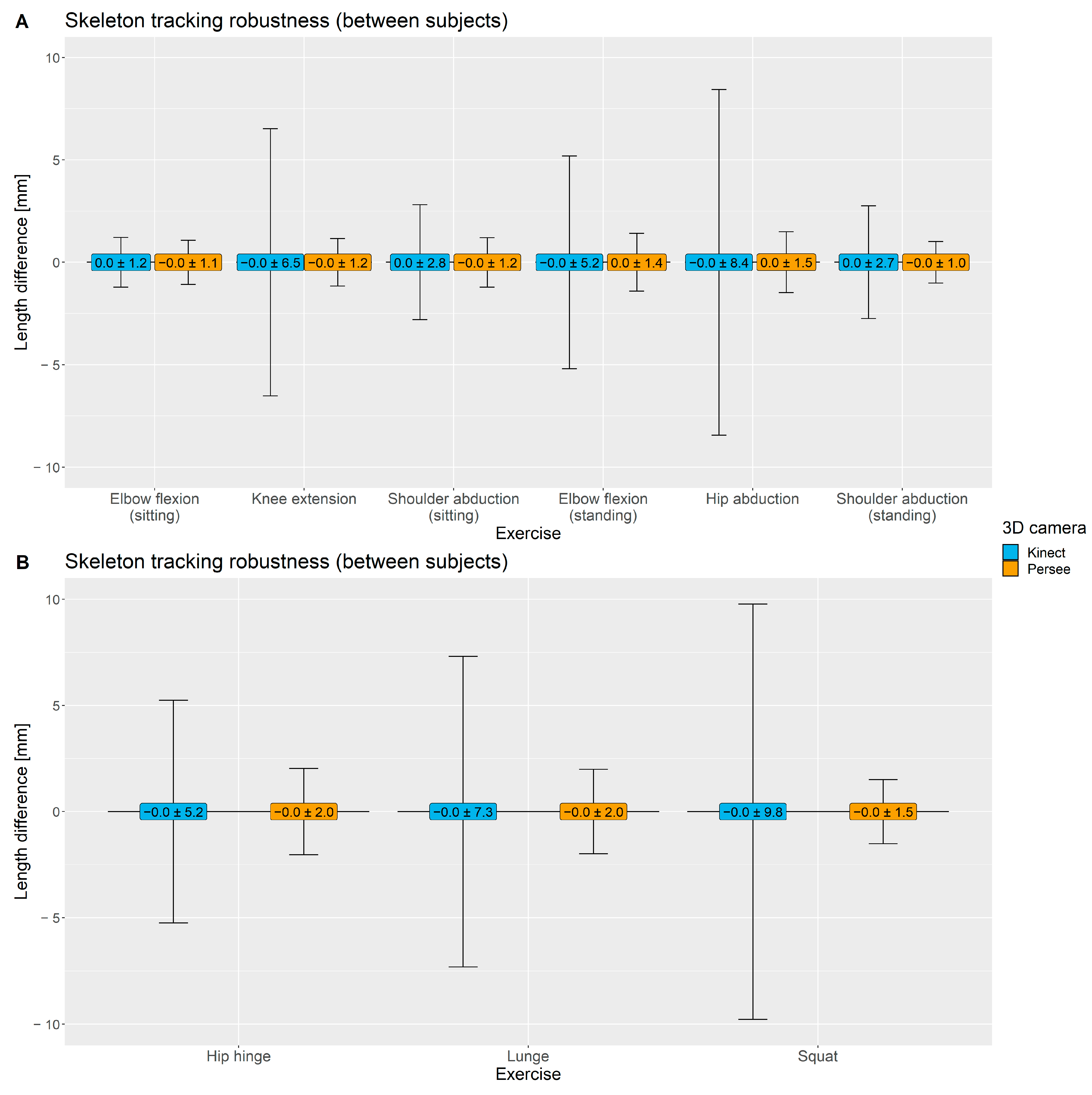
3.2. Skeleton Tracking Robustness
3.3. Accuracies of ILSE Exercise Monitoring
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Egger, G.; Dixon, J. Beyond obesity and lifestyle: A review of 21st century chronic disease determinants. Biomed. Res. Int. 2014, 2014, 731685. [Google Scholar] [CrossRef] [PubMed]
- Park, S.W.; Goodpaster, B.H.; Lee, J.S.; Kuller, L.H.; Boudreau, R.; de Rekeneire, N.; Harris, T.B.; Kritchevsky, S.; Tylavsky, F.A.; Nevitt, M.; et al. Excessive Loss of Skeletal Muscle Mass in Older Adults with Type 2 Diabetes. Diabetes Care 2009, 32, 1993–1997. [Google Scholar] [CrossRef]
- WHO. Vienna Declaration on Nutrition and Noncommunicable Diseases in the Context of Health 2020. In Proceedings of the WHO Ministerial Conference on Nutrition and Noncommunicable Diseases in the Context of Health 2020, Vienna, Austria, 4–5 July 2013. [Google Scholar]
- Hallal, P.C.; Andersen, L.B.; Bull, F.C.; Guthold, R.; Haskell, W. Physical activity levels of the world’ s population Surveillance progress, gaps and prospects. Lancet 2012, 380, 247–257. [Google Scholar] [CrossRef]
- Gomes, M.; Figueiredo, D.; Teixeira, L.; Poveda, V.; Paúl, C.; Santos-Silva, A.; Costa, E. Physical inactivity among older adults across Europe based on the SHARE database. Age Ageing 2017, 46, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Chung, S.; Domino, M.E.; Stearns, S.C.; Popkin, B.M. Retirement and Physical Activity. Am. J. Prev. Med. 2009, 36, 422–428. [Google Scholar] [CrossRef] [PubMed]
- WHO. Global Recommendations on Physical Activity for Health; WHO: Geneva, Switzerland, 2010; Volume 60. [Google Scholar]
- Ciolac, E. Exercise training as a preventive tool for age-related disorders: A brief review. Clinics 2013, 68, 710–717. [Google Scholar] [CrossRef]
- Paganini-Hill, A.; Greenia, D.E.; Perry, S.; Sajjadi, S.A.; Kawas, C.H.; Corrada, M.M. Lower likelihood of falling at age 90+ is associated with daily exercise a quarter of a century earlier: The 90+ Study. Age Ageing 2017, 46, 951–957. [Google Scholar] [CrossRef]
- De Groot, G.C.L.; Fagerström, L. Older adults’ motivating factors and barriers to exercise to prevent falls. Scand. J. Occup. Ther. 2011, 18, 153–160. [Google Scholar] [CrossRef]
- Belza, B.; Walwick, J.; Shiu-Thornton, S.; Schwartz, S.; Taylor, M.; LoGerfo, J. Older adult perspectives on physical activity and exercise: Voices from multiple cultures. Prev. Chronic Dis. 2004, 1, A09. [Google Scholar]
- Resnick, B.; Spellbring, A.M. Understanding what motivates older adults to exercise. J. Gerontol. Nurs. 2000, 26, 34–42. [Google Scholar] [CrossRef]
- Taylor, D. Physical activity is medicine for older adults. Postgrad. Med. J. 2014, 90, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Bäck, M.; Öberg, B.; Krevers, B. Important aspects in relation to patients’ attendance at exercise-based cardiac rehabilitation—Facilitators, barriers and physiotherapist’s role: A qualitative study. BMC Cardiovasc. Disord. 2017, 17, 77. [Google Scholar] [CrossRef]
- Thakur, S.; Rao, S.N. Ambient Assisted Living Roadmap; The European Ambient Assisted Living Innovation Alliance: Berlin, Germany, 2014. [Google Scholar]
- Tang, R.; Tang, A.; Yang, X.-D.; Bateman, S.; Jorge, J. Physio@Home: Exploring visual guidance and feedback techniques for physiotherapy exercises. In Proceedings of the Extended Abstracts of the 33rd Annual ACM Conference on Human Factors in Computing Systems—CHI EA ’15, Seoul, Korea, 18–23 April 2015; pp. 1651–1656. [Google Scholar]
- Zhao, W.; Reinthal, M.A.; Espy, D.D.; Luo, X. Rule-Based Human Motion Tracking for Rehabilitation Exercises: Realtime Assessment, Feedback, and Guidance. IEEE Access 2017, 5, 21382–21394. [Google Scholar] [CrossRef]
- Tannous, H.; Istrate, D.; Tho, M.H.B.; Dao, T.T. Serious game and functional rehabilitation for the lower limbs. Eur. Res. Telemed. Rech. Eur. Télémédecine 2016, 5, 65–69. [Google Scholar] [CrossRef]
- Sixsmith, J.; Sixsmith, A.; Fänge, A.M.; Naumann, D.; Kucsera, C.; Tomsone, S.; Haak, M.; Dahlin-Ivanoff, S.; Woolrych, R. Healthy ageing and home: The perspectives of very old people in five european countries. Soc. Sci. Med. 2014, 106, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Geraedts, H.A.E.; Zijlstra, W.; Zhang, W.; Spoorenberg, S.L.W.; Báez, M.; Far, I.K.; Baldus, H.; Stevens, M. A Home-Based Exercise Program Driven by Tablet Application and Mobility Monitoring for Frail Older Adults: Feasibility and Practical Implications. Prev. Chronic Dis. 2017, 14, 160227. [Google Scholar] [CrossRef]
- Weber, M.; Belala, N.; Clemson, L.; Boulton, E.; Hawley-Hague, H.; Becker, C.; Schwenk, M. Feasibility and Effectiveness of Intervention Programmes Integrating Functional Exercise into Daily Life of Older Adults: A Systematic Review. Gerontology 2018, 64, 172–187. [Google Scholar] [CrossRef]
- Toots, A.; Littbrand, H.; Lindelöf, N.; Wiklund, R.; Holmberg, H.; Nordström, P.; Lundin-Olsson, L.; Gustafson, Y.; Rosendahl, E. Effects of a High-Intensity Functional Exercise Program on Dependence in Activities of Daily Living and Balance in Older Adults with Dementia. J. Am. Geriatr. Soc. 2016, 64, 55–64. [Google Scholar] [CrossRef]
- Park, S.-H.; Han, K.S.; Kang, C.-B. Effects of exercise programs on depressive symptoms, quality of life, and self-esteem in older people: A systematic review of randomized controlled trials. Appl. Nurs. Res. 2014, 27, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Schneider, C.; Trukeschitz, B.; Rieser, H. Measuring the use of the active and assisted living prototype CARIMO for home care service users: Evaluation framework and results. Appl. Sci. 2020, 10, 38. [Google Scholar] [CrossRef]
- Kritikos, J.; Mehmeti, A.; Nikolaou, G.; Koutsouris, D. Fully portable low-cost motion capture system with real-time feedback for rehabilitation treatment. In Proceedings of the International Conference on Virtual Rehabilitation, ICVR, Tel Aviv, Israel, 21–24 July 2019; pp. 1–8. [Google Scholar]
- Johannesson, P.; Perjons, E. An Introduction to Design Science; Springer International Publishing: Cham, Switzerland, 2014; Volume 9783319106, ISBN 9783319106328. [Google Scholar]
- Giancola, S.; Valenti, M.; Sala, R. State-of-the-Art Devices Comparison. In A Survey on 3D Cameras: Metrological Comparison of Time-of-Flight, Structured-Light and Active Stereoscopy Technologies; Springer Briefs in Computer Science; Springer: Cham, Switerland, 2018; pp. 29–39. ISBN 978-3-319-91761-0. [Google Scholar]
- Lo Presti, L.; La Cascia, M. 3D skeleton-based human action classification: A survey. Pattern Recognit. 2016, 53, 130–147. [Google Scholar] [CrossRef]
- Planinc, R.; Chaaraoui, A.A.; Kampel, M.; Florez-Revuelta, F. Computer vision for active and assisted living. Act. Assist. Living Technol. Appl. 2016, 57, 1–23. [Google Scholar]
- Sabatini, A.M. Quaternion-based extended Kalman filter for determining orientation by inertial and magnetic sensing. IEEE Trans. Biomed. Eng. 2006, 53, 1346–1356. [Google Scholar] [CrossRef]
- Cebanov, E.; Dobre, C.; Gradinaru, A.; Ciobanu, R.I.; Stanciu, V.D. Activity recognition for ambient assisted living using off-the-shelf motion sensing input devices. In Proceedings of the 2019 Global IoT Summit (GIoTS), Aarhus, Denmark, 17–21 June 2019. [Google Scholar]
- Calin, A.D.; Coroiu, A. Interchangeability of Kinect and Orbbec Sensors for Gesture Recognition. In Proceedings of the 2018 IEEE 14th International Conference on Intelligent Computer Communication and Processing (ICCP), Cluj-Napoca, Romania, 6–8 September 2018; pp. 309–315. [Google Scholar]
- Wang, Q.; Kurillo, G.; Ofli, F.; Bajcsy, R. Evaluation of pose tracking accuracy in the first and second generations of microsoft Kinect. In Proceedings of the 2015 International Conference on Healthcare Informatics, Dallas, TX, USA, 21–23 October 2015; pp. 380–389. [Google Scholar]
- Pagliari, D.; Pinto, L. Calibration of Kinect for Xbox One and comparison between the two generations of microsoft sensors. Sensors 2015, 15, 27569–27589. [Google Scholar] [CrossRef]
- Bonnechère, B.; Jansen, B.; Salvia, P.; Bouzahouene, H.; Omelina, L.; Moiseev, F.; Sholukha, V.; Cornelis, J.; Rooze, M.; Van Sint Jan, S. Validity and reliability of the Kinect within functional assessment activities: Comparison with standard stereophotogrammetry. Gait Posture 2014, 39, 593–598. [Google Scholar] [CrossRef] [PubMed]
- Obdrzalek, S.; Kurillo, G.; Ofli, F.; Bajcsy, R.; Seto, E.; Jimison, H.; Pavel, M. Accuracy and robustness of Kinect pose estimation in the context of coaching of elderly population. In Proceedings of the 2012 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, San Diego, CA, USA, 28 August–1 September 2012; pp. 1188–1193. [Google Scholar]
- Xu, X.; McGorry, R.W. The validity of the first and second generation Microsoft Kinect for identifying joint center locations during static postures. Appl. Ergon. 2015, 49, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Lange, W.; Windel, A. Kleine Ergonomische Datensammlung; Bundesanstalt für Arbeitsschutz und Arbeitsmedizin, TÜV Verlag: Köln, Germany, 2002; pp. 1–16. [Google Scholar]
- Albert, J.A.; Owolabi, V.; Gebel, A.; Brahms, C.M.; Granacher, U.; Arnrich, B. Evaluation of the pose tracking performance of the azure kinect and kinect v2 for gait analysis in comparison with a gold standard: A pilot study. Sensors 2020, 20, 5104. [Google Scholar] [CrossRef] [PubMed]
- Schlagenhauf, F.; Sahoo, P.P.; Singhose, W. Comparison of single-kinect and dual-kinect motion capture of upper-body joint tracking. In Proceedings of the 2017 11th Asian Control Conference (ASCC), Gold Coast, QLD, Australia, 17–20 December 2017; pp. 256–261. [Google Scholar]
- Wei, T.; Lee, B.; Qiao, Y.; Kitsikidis, A.; Dimitropoulos, K.; Grammalidis, N. Experimental study of skeleton tracking abilities from microsoft kinect non-frontal views. In Proceedings of the 2015 3DTV-Conference: The True Vision—Capture, Transmission and Display of 3D Video (3DTV-CON), Lisbon, Portugal, 8–10 July 2015; pp. 1–4. [Google Scholar]
- Yang, P.; Xie, L.; Wang, C.; Lu, S. IMU-Kinect: A motion sensor-based gait monitoring system for intelligent healthcare. In Adjunct Proceedings of the 2019 ACM International Joint Conference on Pervasive and Ubiquitous Computing and Proceedings of the 2019 ACM International Symposium on Wearable Computers; ACM Press: New York, NY, USA, 2019; pp. 350–353. [Google Scholar]
- Ting, H.Y.; Tan, Y.W.D.; Lau, B.Y.S. Potential and Limitations of Kinect for Badminton Performance Analysis and Profiling. Indian J. Sci. Technol. 2016, 9, 1–5. [Google Scholar] [CrossRef]
- Tannous, H.; Istrate, D.; Benlarbi-Delai, A.; Sarrazin, J.; Gamet, D.; Ho Ba Tho, M.C.; Dao, T.T. A new multi-sensor fusion scheme to improve the accuracy of knee flexion kinematics for functional rehabilitation movements. Sensors 2016, 16, 1914. [Google Scholar] [CrossRef]
- Naeemabadi, M.; Dinesen, B.; Andersen, O.K.; Najafi, S.; Hansen, J. Evaluating Accuracy and Usability of Microsoft Kinect Sensors and Wearable Sensor for Tele Knee Rehabilitation after Knee Operation. In Proceedings of the Proceedings of the 11th International Joint Conference on Biomedical Engineering Systems and Technologies, Biostec 2018, Funchal, Portugal, 19–21 January 2018; pp. 128–135. [Google Scholar]
- Müller, B.; Ilg, W.; Giese, M.A.; Ludolph, N. Validation of enhanced kinect sensor based motion capturing for gait assessment. PLoS ONE 2017, 12, e0175813. [Google Scholar] [CrossRef]

| Feature | Microsoft Kinect v2 | Orbbec Persee |
|---|---|---|
| Working principle | Time-of-Flight | Structured light |
| Size | 249 × 67 × 66 mm | 172 × 63 × 56 mm |
| Weight | 0.97 kg | 0.8 kg |
| Range | 0.4–4.5 m | 0.6–8.0 m (optimal 0.6–5.0 m) |
| Frame Rate | 30 FPS | 30 FPS |
| Stand-alone system | No | Yes (Android 5 or Ubuntu) |
| Skeleton tracking library | Kinect SDK (version 2.0 used for the comparison) | Orbbec Astra SDK or Nuitrack (version 1.3.1 used for the comparison) |
| Tracking capability | 25 joints per skeleton (up to 6 subjects) | 20 joints per skeleton (up to 2 subjects) |
| Exercise | Initial Static Posture | Number of Repetitions |
|---|---|---|
| Shoulder abduction | Sitting | 60 |
| Elbow flexion | Sitting | 62 |
| Knee extension | Sitting | 60 |
| Shoulder abduction | Standing | 59 |
| Elbow flexion | Standing | 60 |
| Hip abduction | Standing | 60 |
| Squat | Standing | 62 |
| Hip hinge | Standing | 59 |
| Lunge | Standing | 60 |
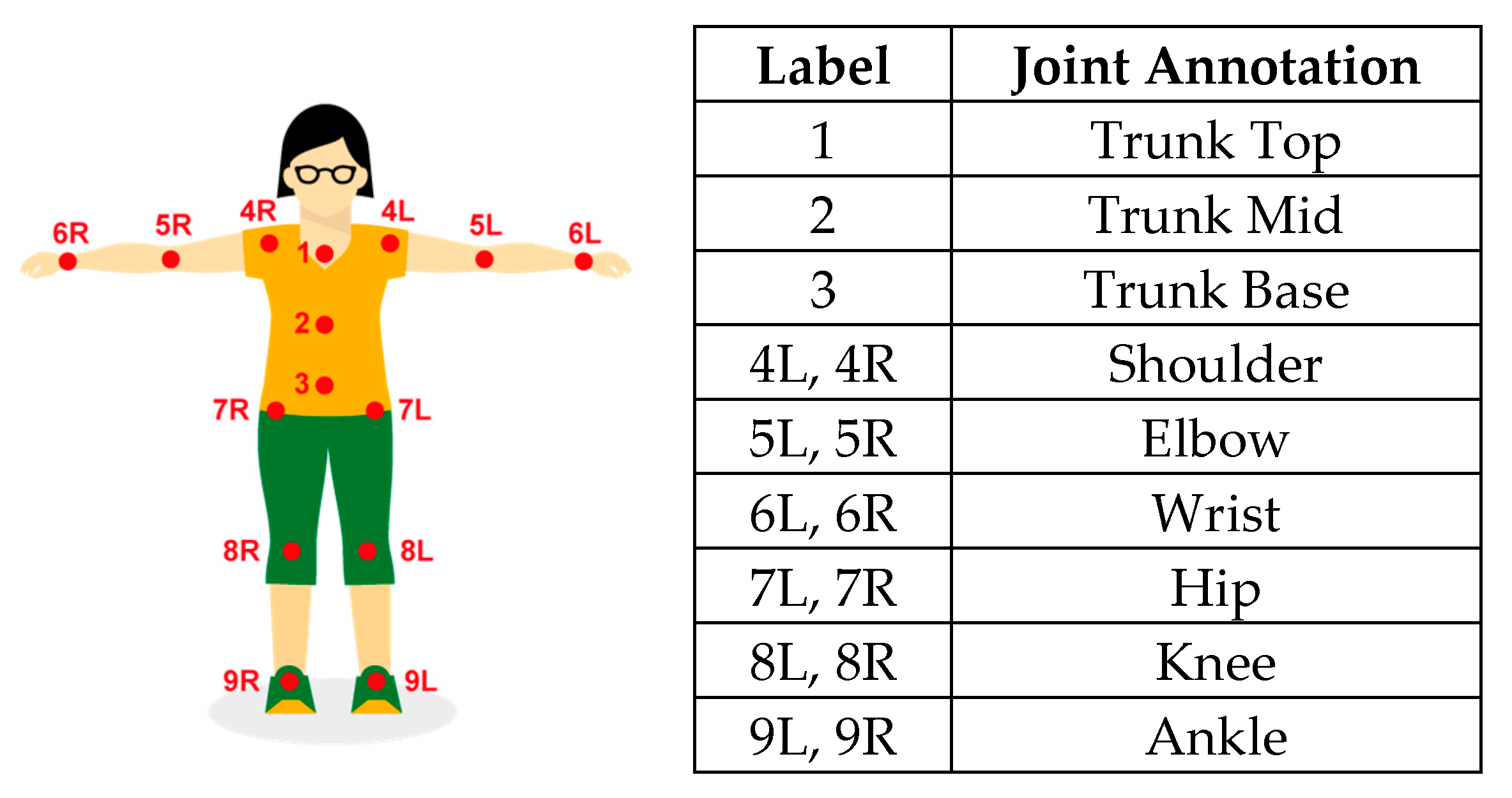
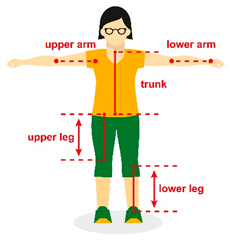 | Body Segment | Proximal Joint | Distal Joint |
|---|---|---|---|
| Upper Arm * | Shoulder | Elbow | |
| Lower Arm * | Elbow | Wrist | |
| Upper Leg * | Hip | Knee | |
| Lower Leg * | Knee | Ankle | |
| Trunk | Trunk Top | Trunk Base |
| Tracking State ‘Tracked’/0.75 over Motion Sequence | ||
|---|---|---|
| Motion Sequence | Kinect v2 | Persee |
| Knee extension (sitting) | - | All joints of P1 |
| Shoulder abduction (sitting) | - | All joints of P1, P2, P3, P5, P6 |
| Shoulder abduction (standing) | All joints of P6 | All joints of P1–P6 |
| Hip abduction (standing) | - | P1, P2, P3, P5, P6 |
| Hip hinge | - | All joints of P4 |
| Number of Correctly Counted Repetitions (Accuracy) | ||
|---|---|---|
| Exercise | Kinect v2 | Persee |
| Elbow flexion (sitting) | 49/62 (79%) | 23/62 (37%) |
| Knee extension (sitting) | 30/60 (50%) | 40/60 (67%) |
| Shoulder abduction (sitting) | 60/60 (100%) | 40/60 (67%) |
| Elbow flexion (standing) | 60/60 (100%) | 20/60 (33%) |
| Shoulder abduction (standing) | 59/59 (100%) | 59/59 (100%) |
| Hip abduction (standing) | 10/60 (17%) | 30/60 (50%) |
| Hip hinge | 19/59 (32%) | 9/59 (15%) |
| Lunge | 50/60 (83%) | 0/60 (0%) |
| Squat | 41/62 (66%) | 32/62 (52%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Venek, V.; Kremser, W.; Stöggl, T. Towards a Live Feedback Training System: Interchangeability of Orbbec Persee and Microsoft Kinect for Exercise Monitoring. Designs 2021, 5, 30. https://doi.org/10.3390/designs5020030
Venek V, Kremser W, Stöggl T. Towards a Live Feedback Training System: Interchangeability of Orbbec Persee and Microsoft Kinect for Exercise Monitoring. Designs. 2021; 5(2):30. https://doi.org/10.3390/designs5020030
Chicago/Turabian StyleVenek, Verena, Wolfgang Kremser, and Thomas Stöggl. 2021. "Towards a Live Feedback Training System: Interchangeability of Orbbec Persee and Microsoft Kinect for Exercise Monitoring" Designs 5, no. 2: 30. https://doi.org/10.3390/designs5020030
APA StyleVenek, V., Kremser, W., & Stöggl, T. (2021). Towards a Live Feedback Training System: Interchangeability of Orbbec Persee and Microsoft Kinect for Exercise Monitoring. Designs, 5(2), 30. https://doi.org/10.3390/designs5020030







